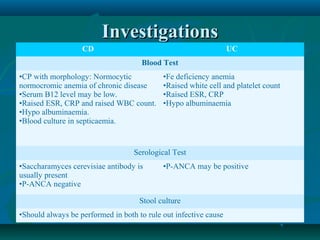
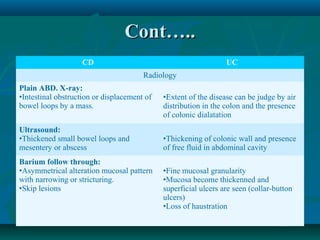
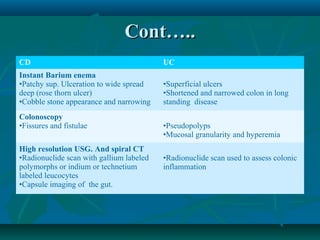
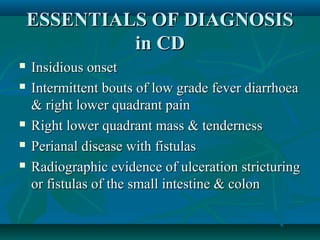
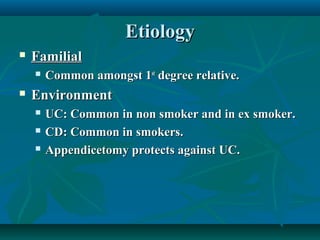
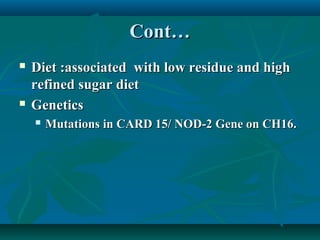
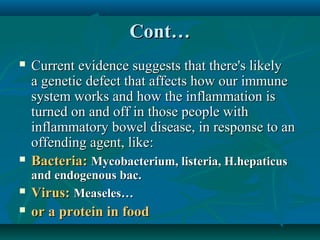
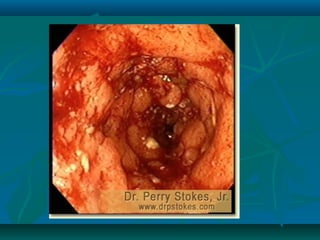
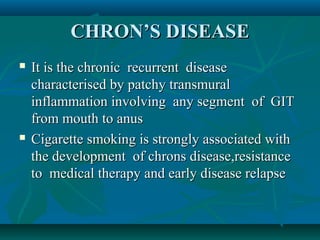
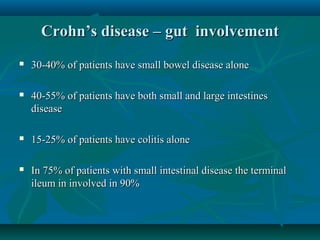
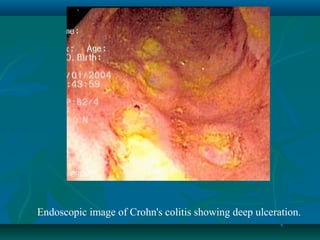
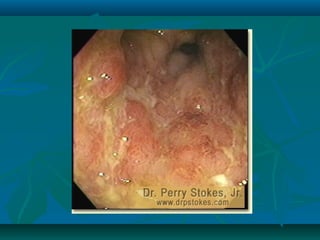
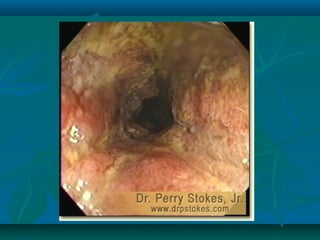
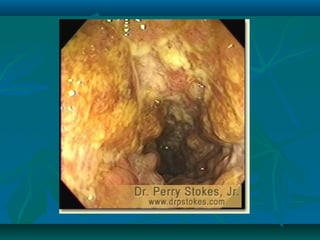
Inflammatory bowel disease refers to ulcerative colitis and Crohn's disease, which cause chronic inflammation of the intestines. Ulcerative colitis affects only the large intestine and causes ulcers, bleeding, and diarrhea. Crohn's disease can impact any part of the digestive tract and causes patchy inflammation that may lead to complications like fistulas or strictures. Both conditions are characterized by periods of remission and relapse of symptoms. Their causes are unknown but involve genetic and environmental factors. Diagnosis involves medical history, physical exam, blood tests, endoscopy, and imaging.




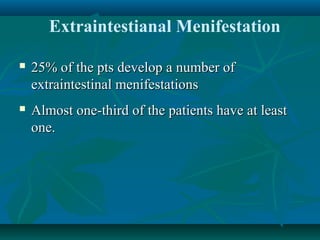
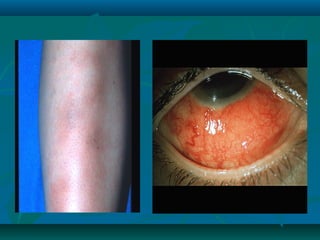
![Extraintestinal manifestation
•Eyes: Uveitis, Episcleritis, Conjuctivitis
•Joints: Peripheral arthropathy, arthralgia, ankylosing
spondylits, inflammatory Back pain
•Skin: Erythema nodosum, pyoderma gangrenosum
•Liver and Biliary tree: Sclerosing cholangitis [UC]
•Nephrolithiasis [Oxalate Stone in pt with small bowel
disease or after resection] (CD)
•Oral apthous leisions (CD)
•Gall stone(CD)
•Venous thrombosis](https://image.slidesharecdn.com/ibd2-140115103702-phpapp02/85/Inflammatory-Bowel-Disease-42-320.jpg)