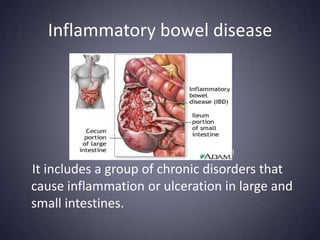
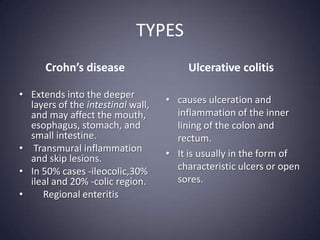
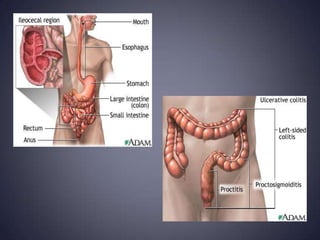
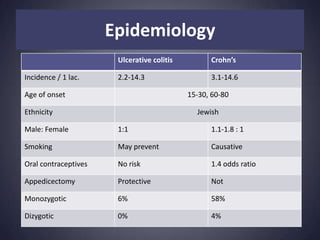
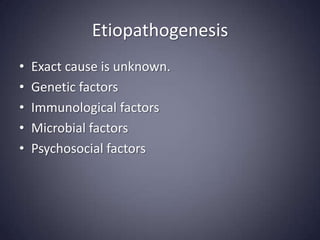
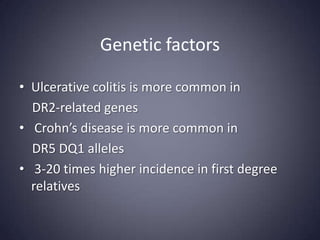
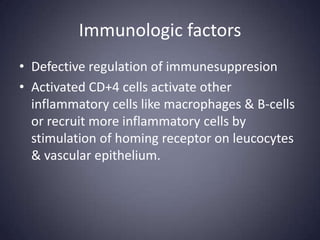
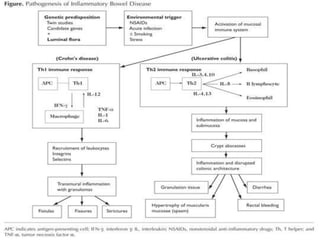
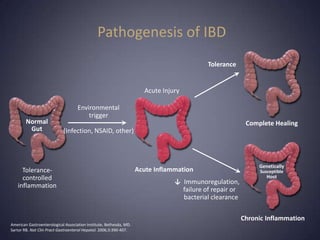
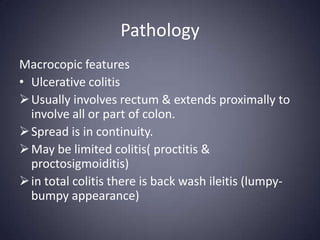
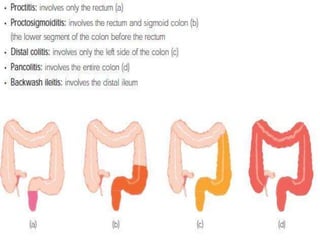
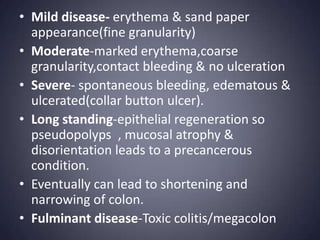
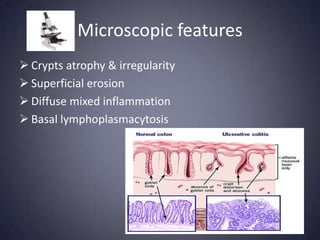
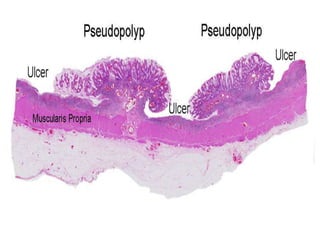
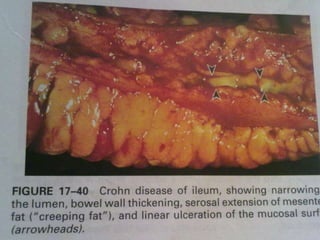
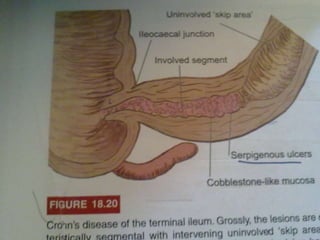
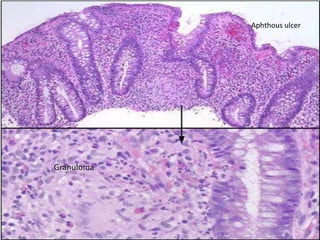
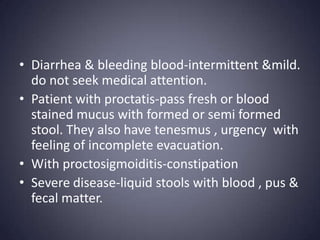
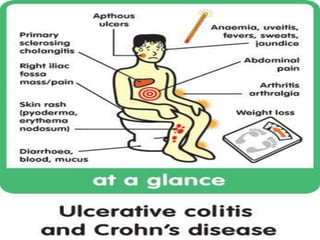
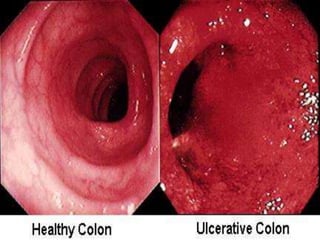
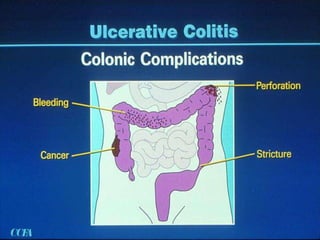
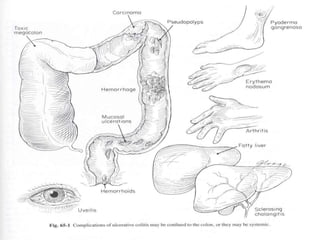
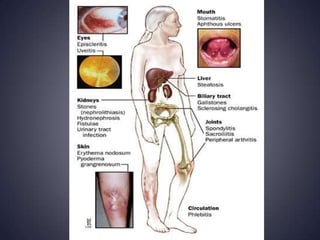
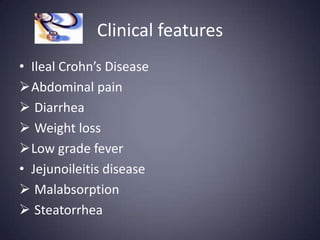
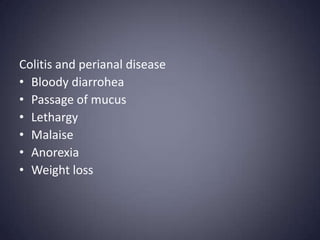
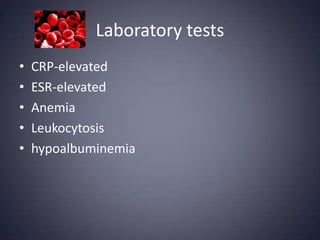
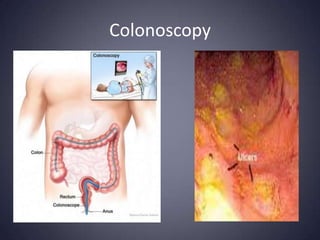
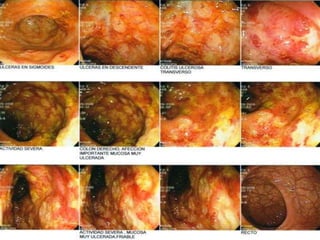
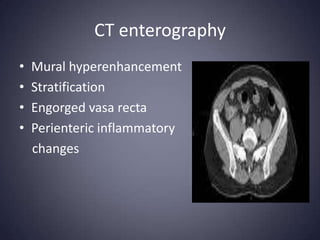
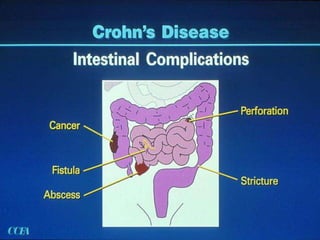
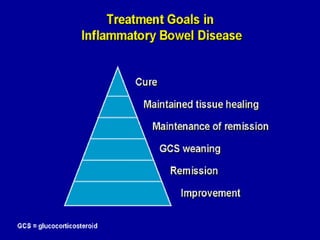
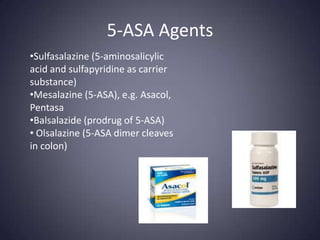
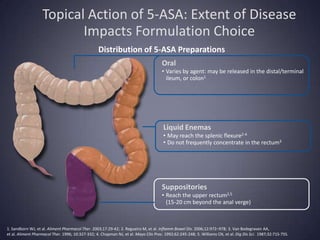
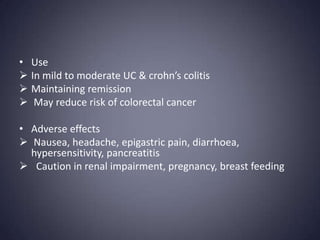
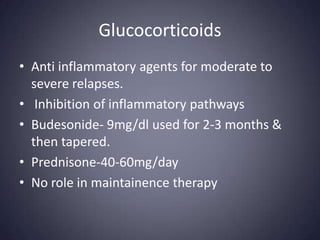
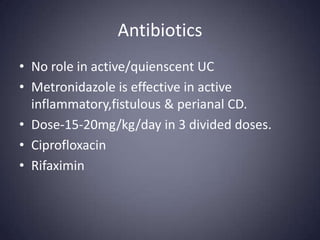
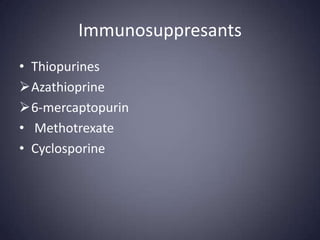
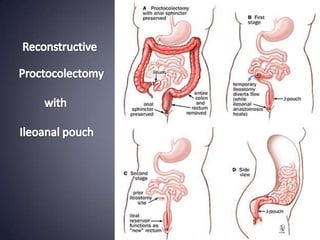
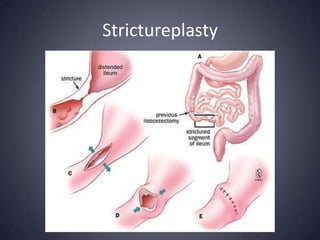
Inflammatory bowel disease includes Crohn's disease and ulcerative colitis, which cause inflammation in the intestines. Crohn's disease can affect any part of the gastrointestinal tract and causes transmural inflammation, while ulcerative colitis causes inflammation and ulcers only in the inner lining of the colon and rectum. Treatment involves lifestyle changes, medications like 5-ASA agents, glucocorticoids, antibiotics, immunosuppressants, and biological therapies. Surgery may be required for severe cases or complications that do not respond to medical management.