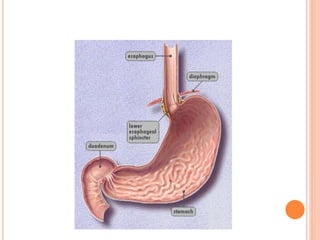
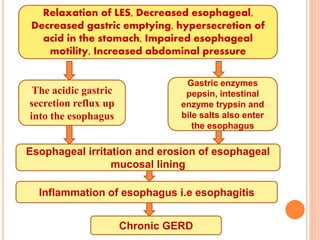
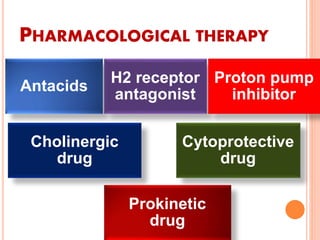
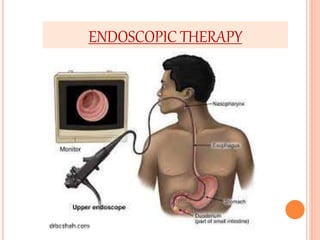
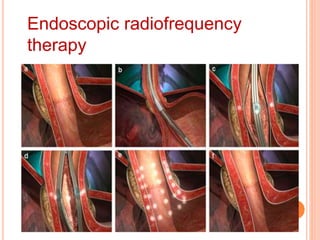
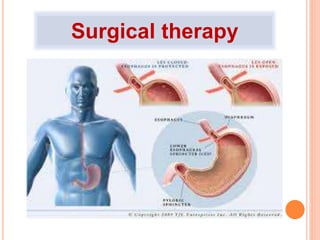
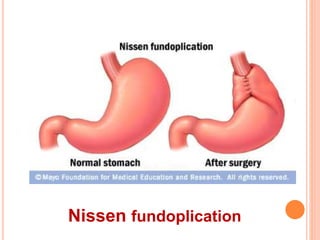
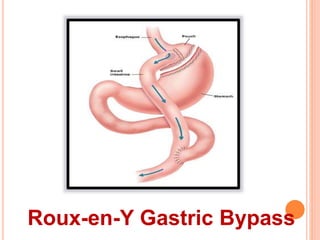
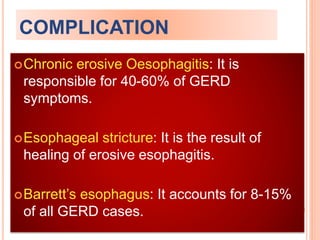
Gastroesophageal reflux disease (GERD) is a chronic condition characterized by the reflux of stomach acids into the esophagus, leading to symptoms such as heartburn and regurgitation. In India, 18.7% of the older population and a significant percentage of pregnant women experience GERD symptoms, with various causas including dietary factors and pregnancy. Management includes lifestyle modifications, pharmacological therapies, and possibly surgical interventions, all aimed at alleviating symptoms and preventing complications such as erosive esophagitis and Barrett's esophagus.

![INCIDENCE:
In India, 18.7% of the older adult population
suffers from GERD. Among pregnant
women, 9.5% women suffer in first trimester,
43.1% women suffer in second trimester
and 54.1% women suffer in third trimester
[according to Indian J Gastroentrol (May-
June 2011) 30(3):105-107]. Approximately
14% to 20% population in USA experience
GERD symptoms at least once a week.](https://image.slidesharecdn.com/gerd-ppt-141125090943-conversion-gate01/85/Gerd-ppt-5-320.jpg)