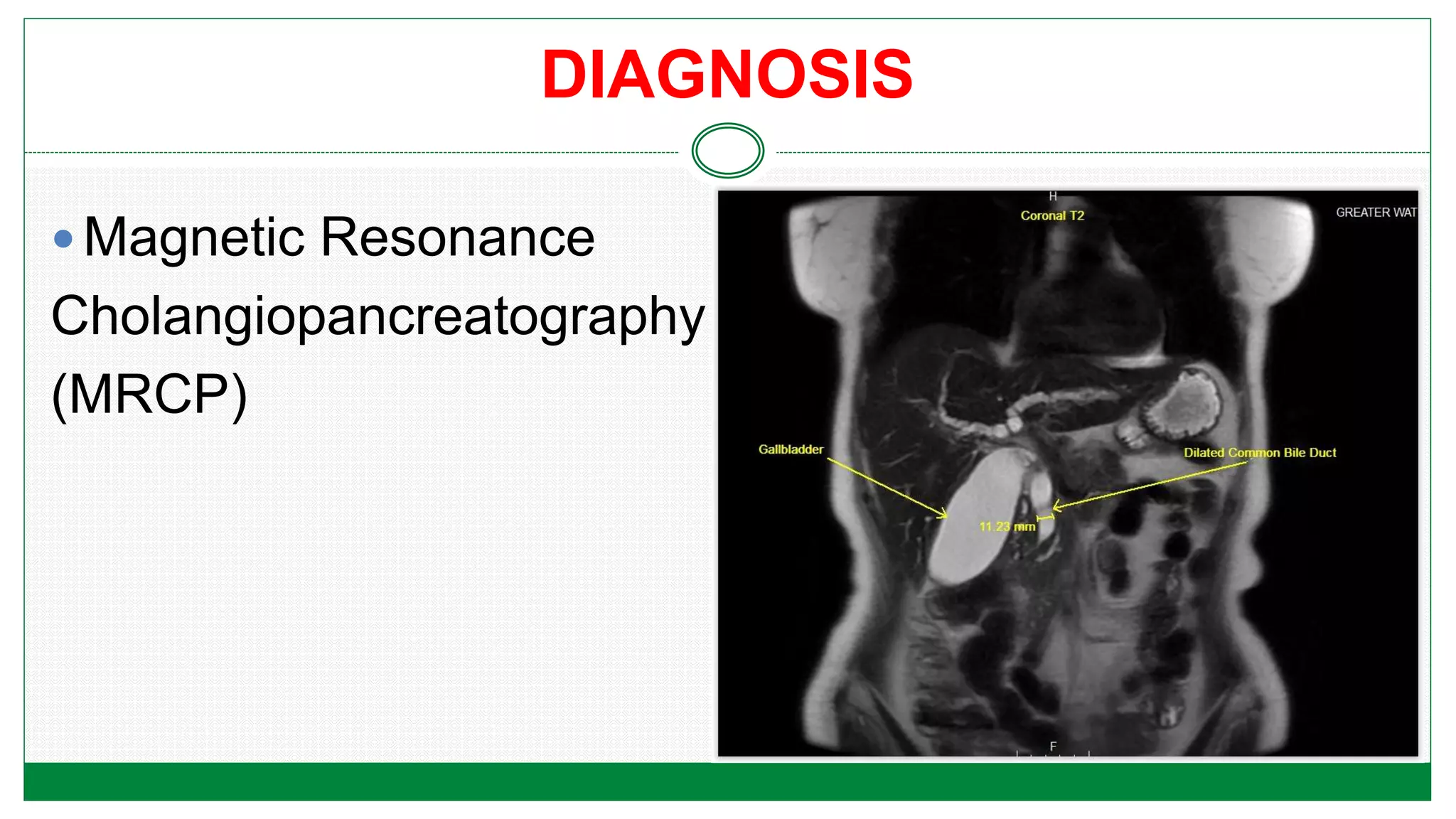
The document discusses pancreatitis, including defining acute pancreatitis as an inflammation of the pancreas that can range from mild edema to severe hemorrhagic necrosis. It outlines causes such as gallstones and alcohol, pathophysiology, clinical manifestations like abdominal pain and vomiting, potential complications, diagnostic tests, treatment including pain management and nutritional support, and discusses chronic pancreatitis.