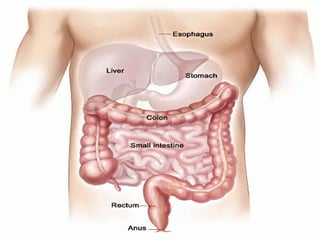
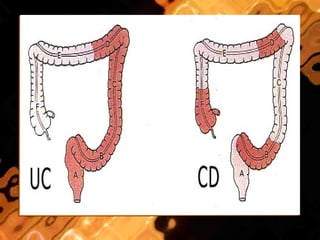
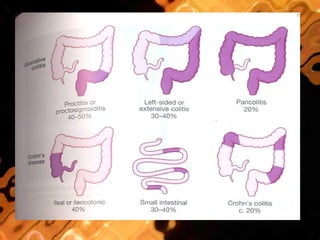
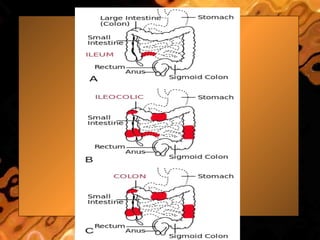
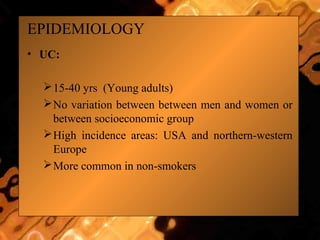
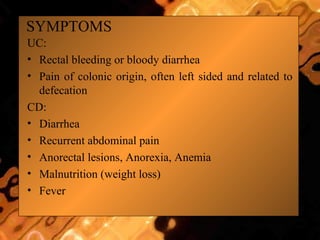
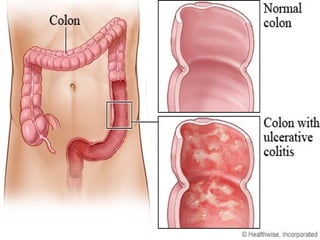
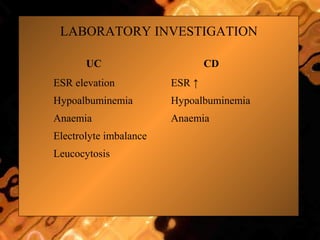
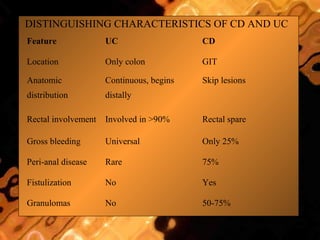
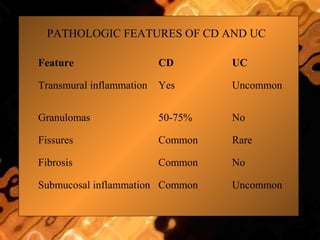
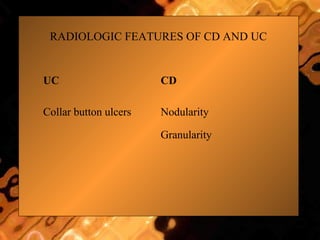
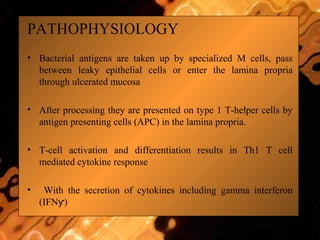
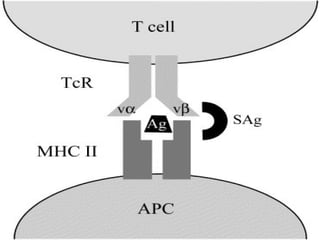
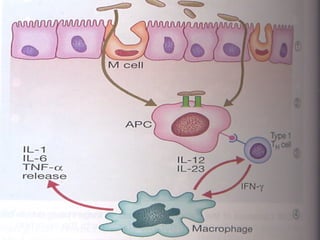
Inflammatory Bowel Disease (IBD) refers to two conditions: Crohn's disease and ulcerative colitis. Crohn's disease causes chronic inflammation of the gastrointestinal tract that can affect any location from mouth to anus in a discontinuous pattern. Ulcerative colitis causes non-granulomatous inflammation of the colon and rectum in a continuous pattern beginning in the rectum. The causes of IBD are not fully known but involve an immune reaction to environmental triggers in genetically predisposed individuals. Symptoms vary depending on the location and severity of inflammation. Management involves non-pharmacological approaches as well as medications to reduce inflammation like aminosalicates, corticosteroids, immunosuppress