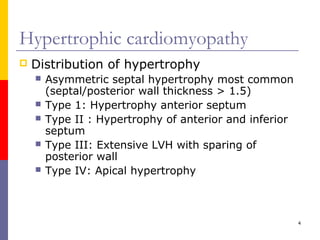
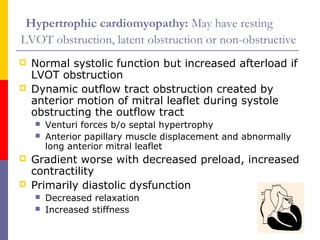
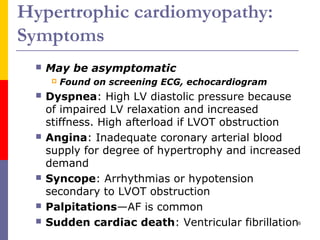
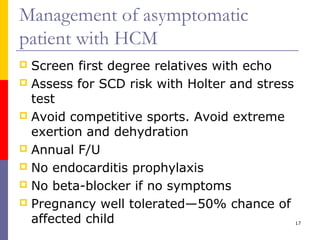
Hypertrophic cardiomyopathy is a genetic heart condition characterized by thickened heart muscle and potential outflow tract obstruction. It affects 0.2-0.5% of the population and is caused by mutations in genes encoding sarcomere proteins. Symptoms include chest pain, dizziness, and palpitations. Diagnosis is made via echocardiogram and genetic testing. Treatment focuses on symptom relief through medications or procedures to reduce outflow tract obstruction, as well as preventing sudden cardiac death through ICD implantation in high-risk patients.