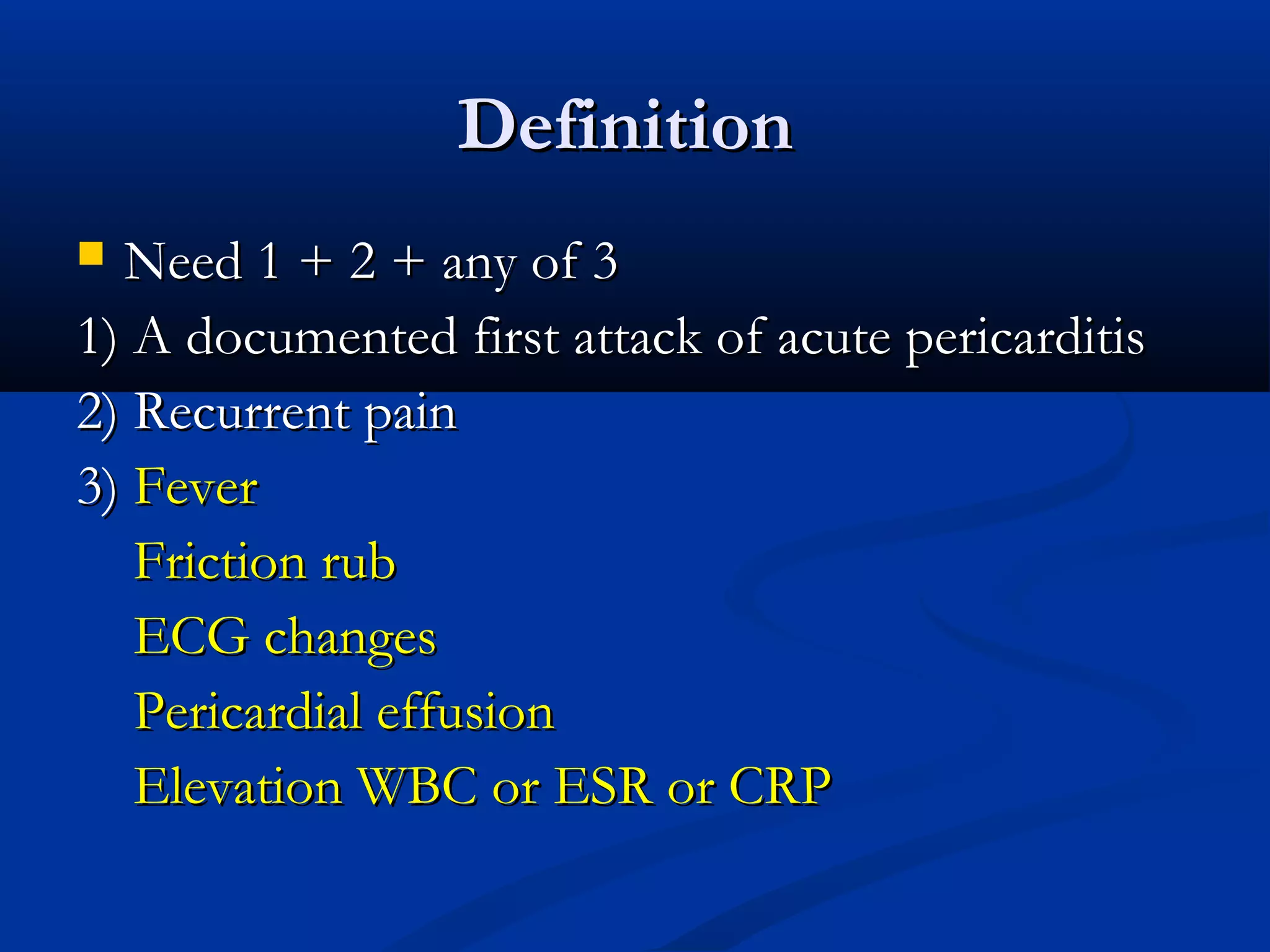
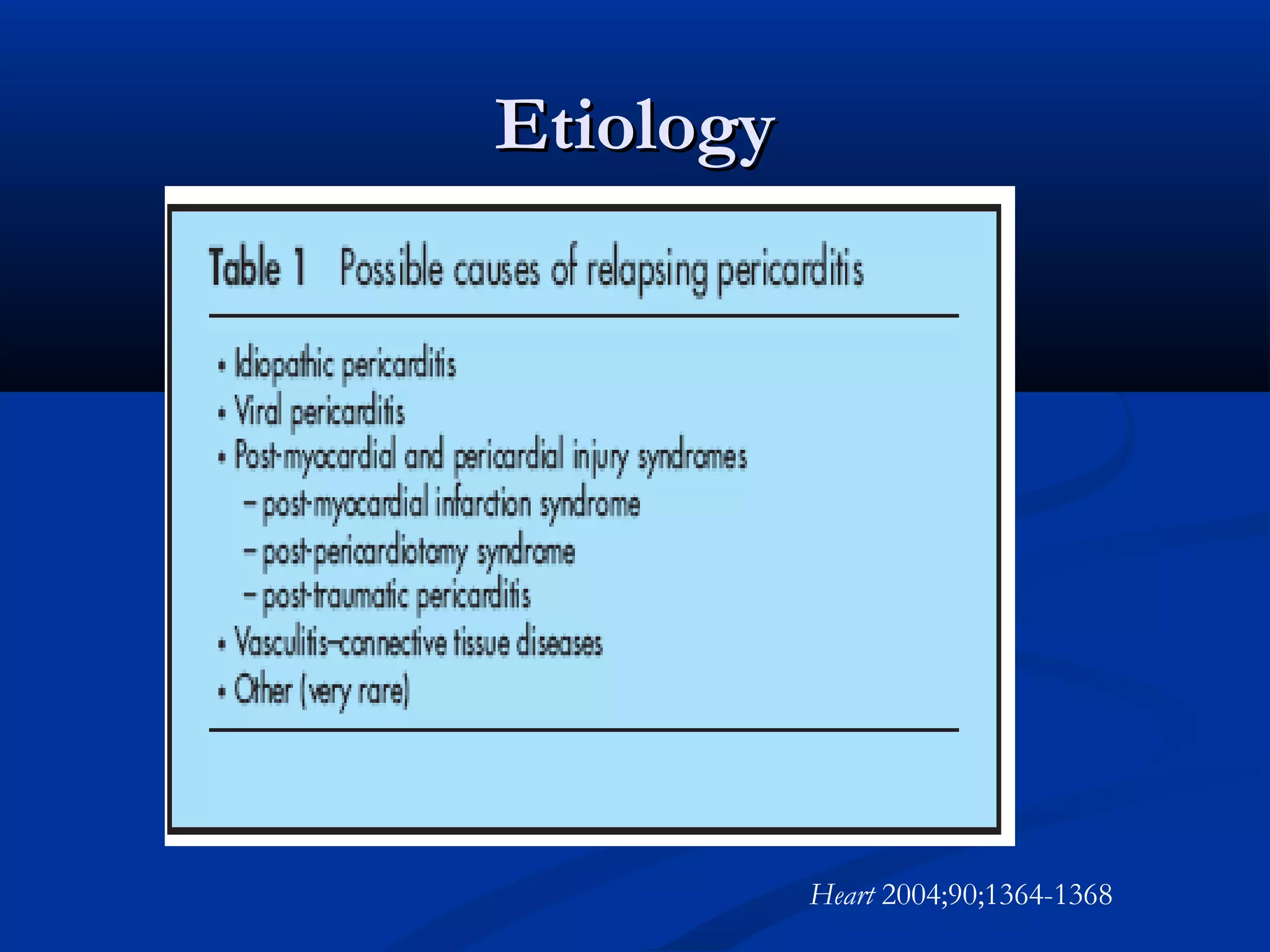
- The document discusses three cases of patients presenting with chest pain and suspected pericarditis.
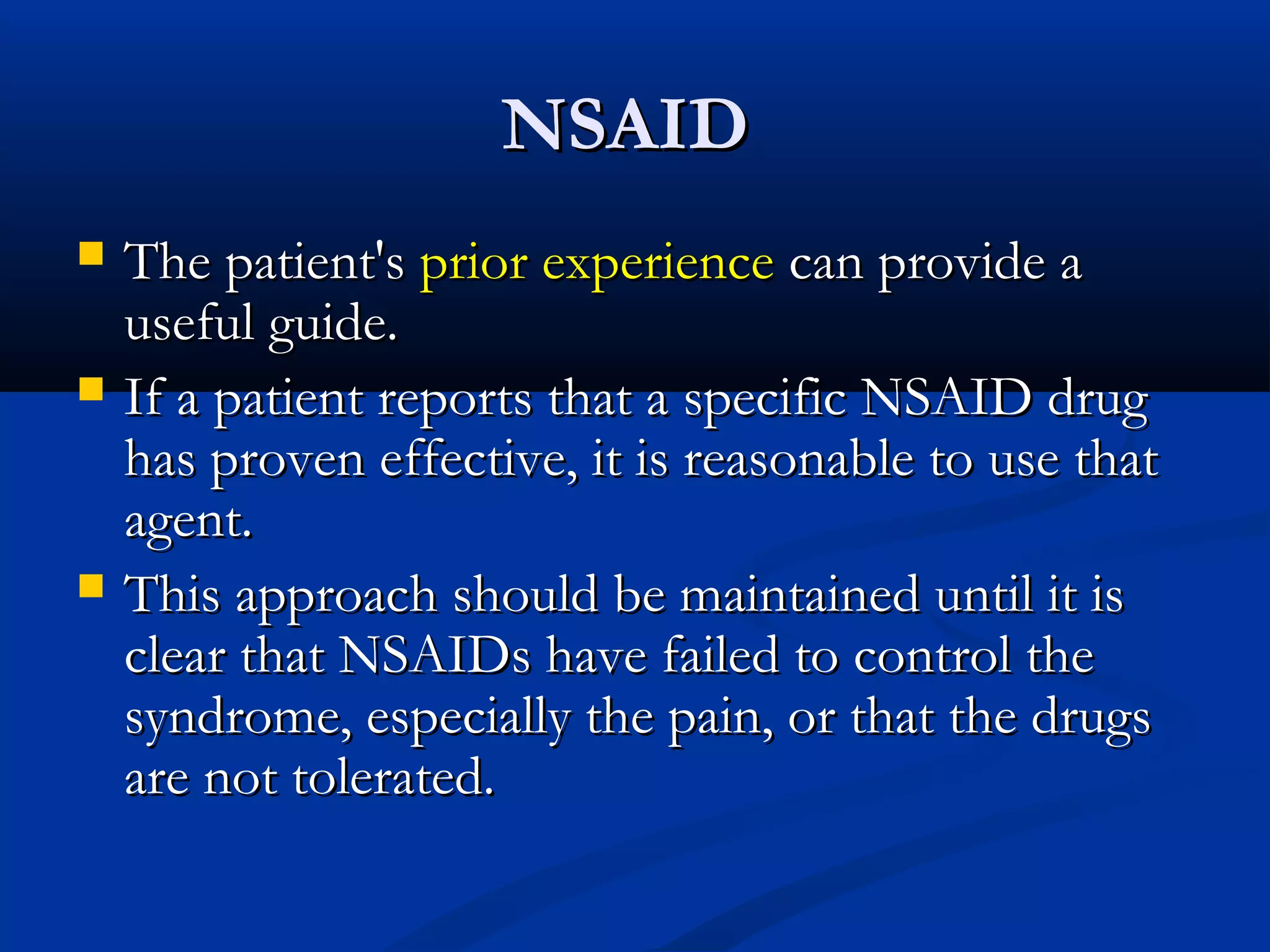
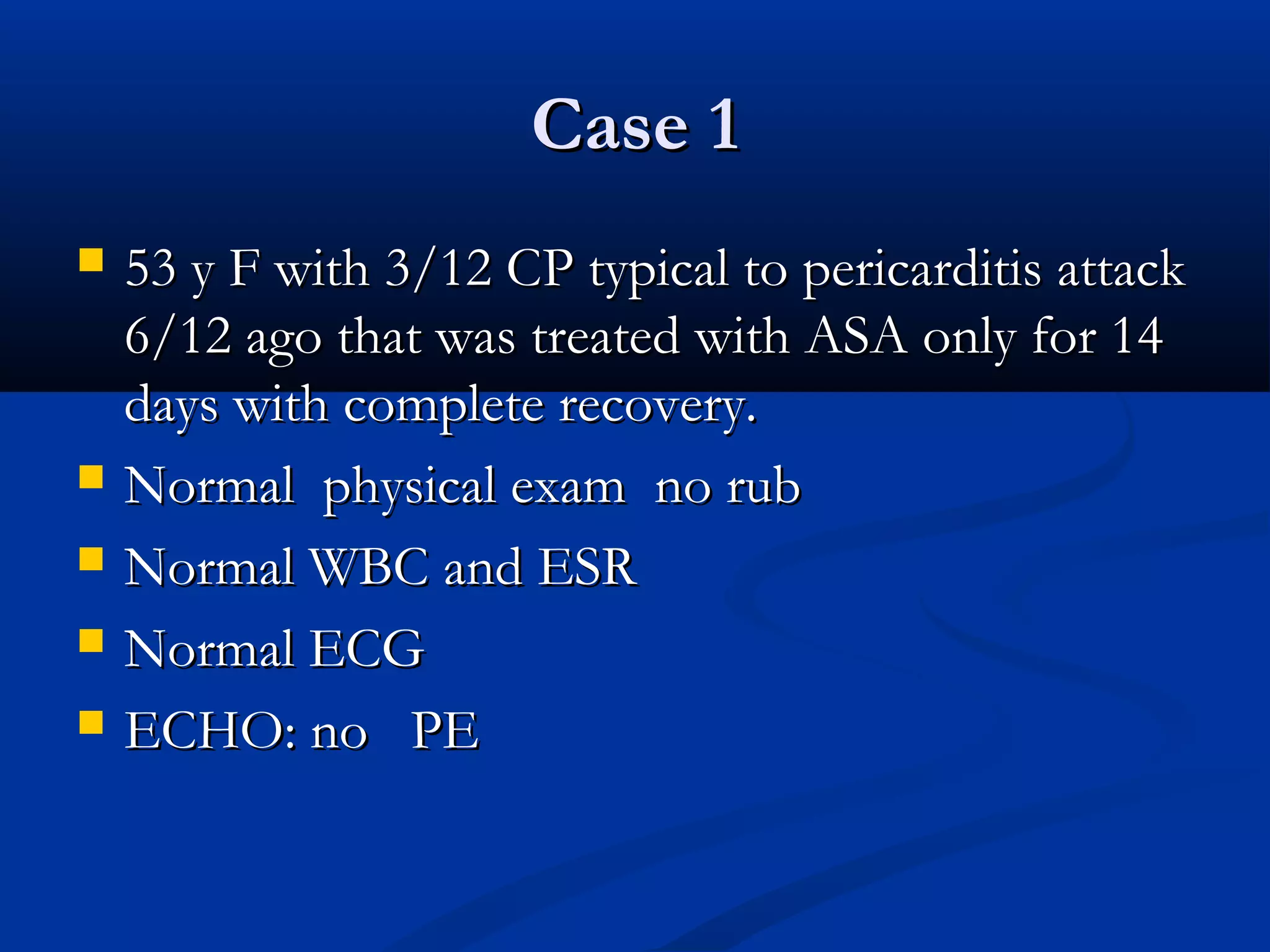
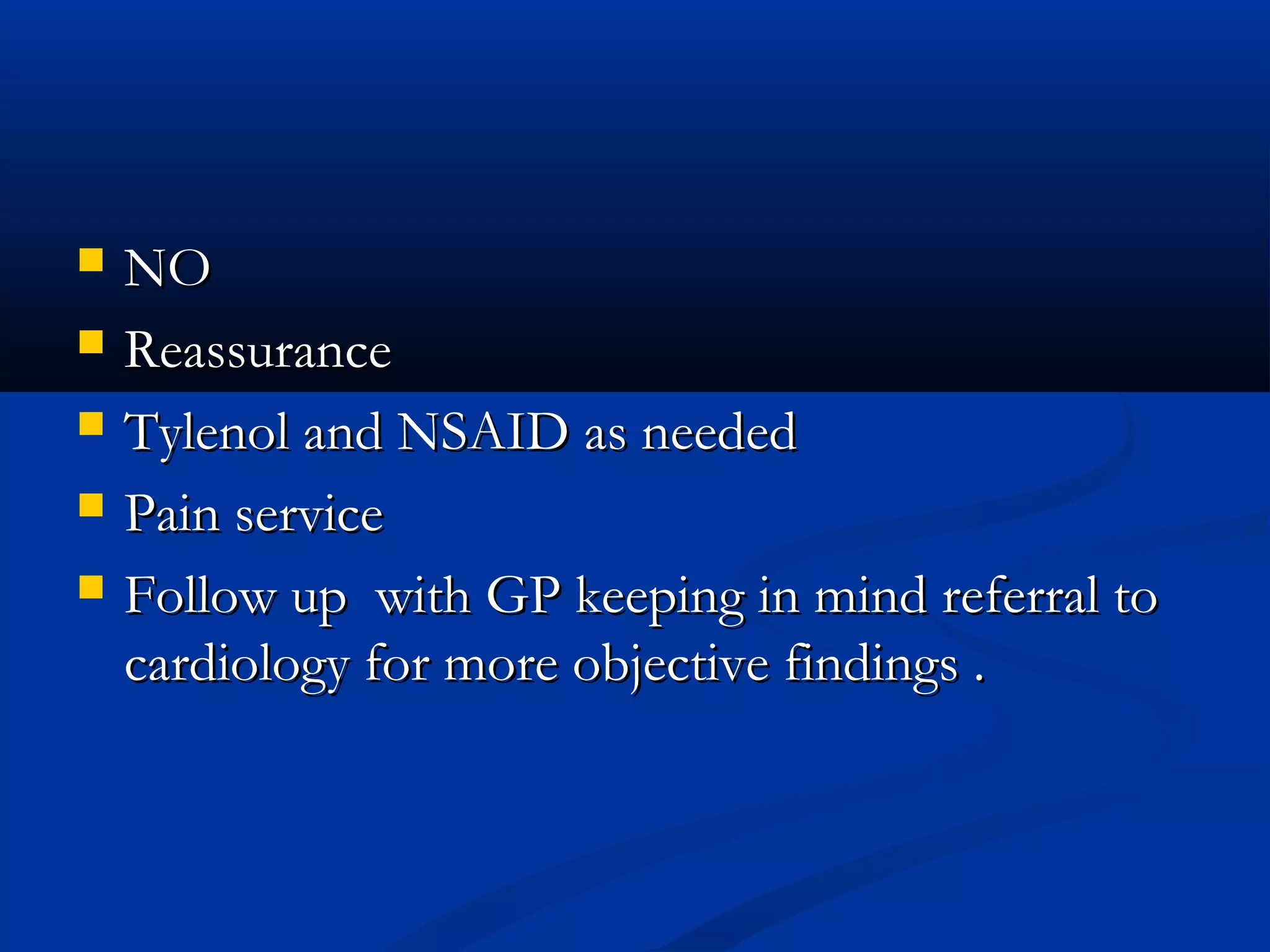
- For the first patient, the doctor would not diagnose recurrent pericarditis and would reassure the patient, treating pain with Tylenol or NSAIDs as needed.
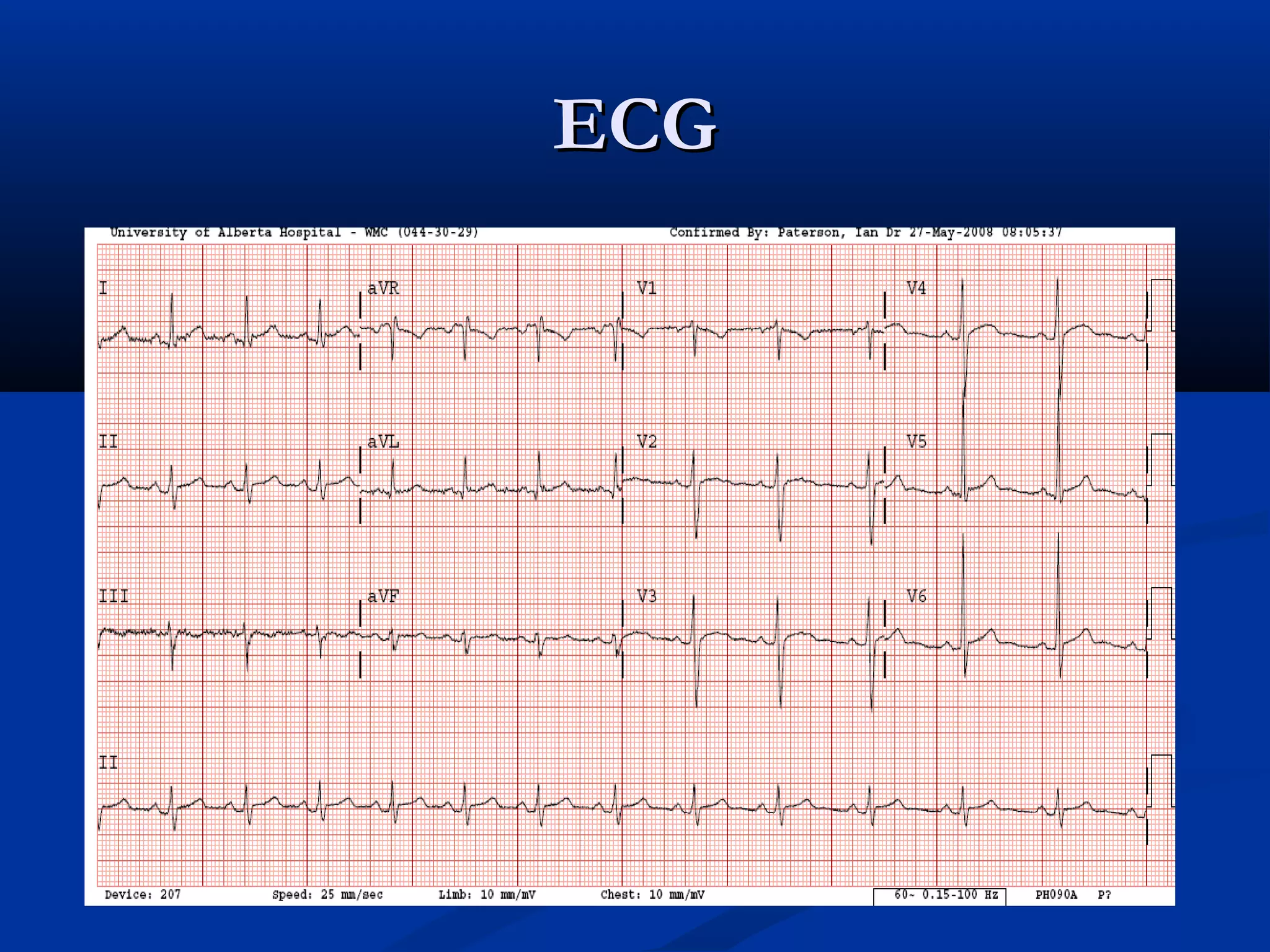
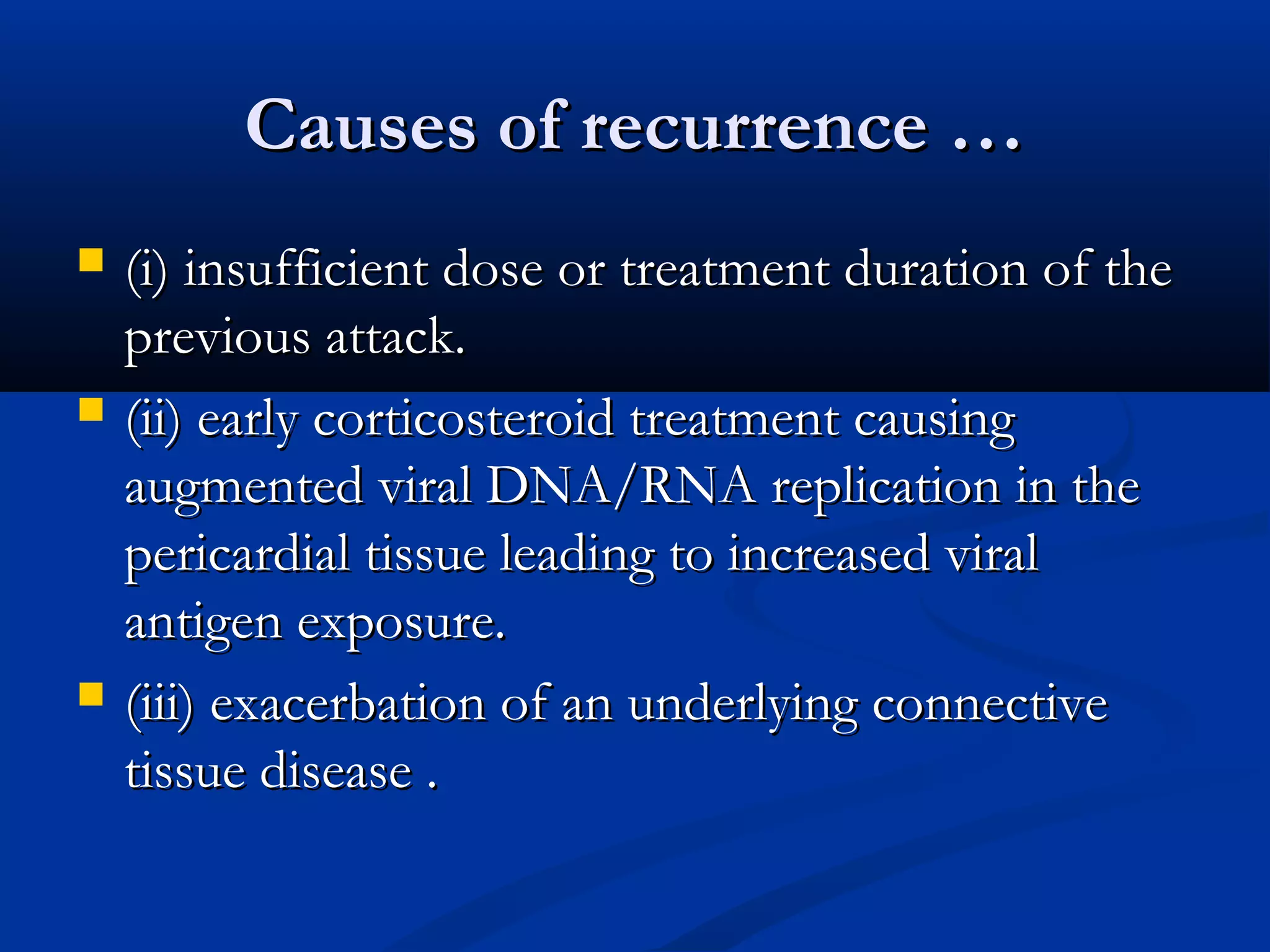
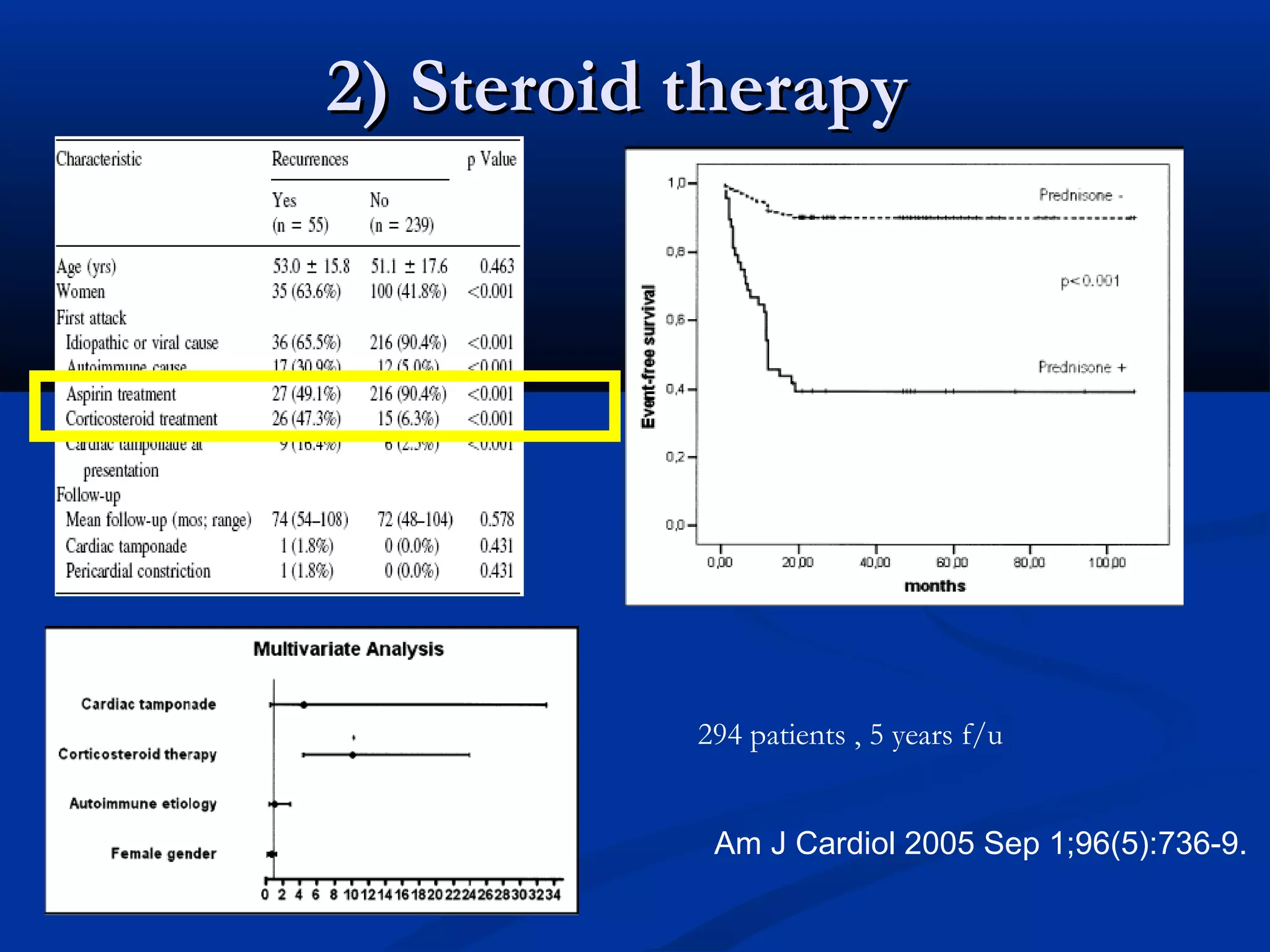
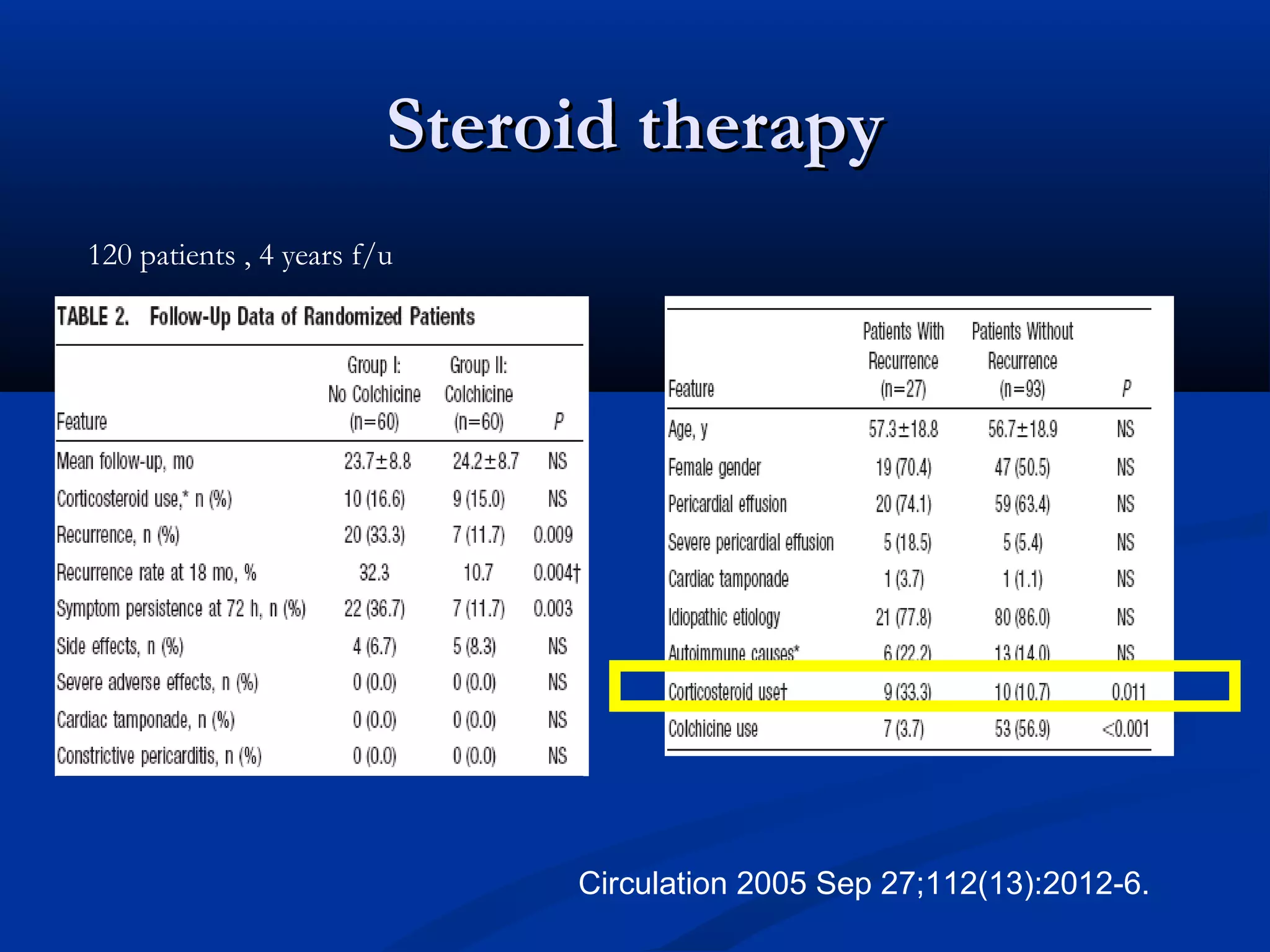
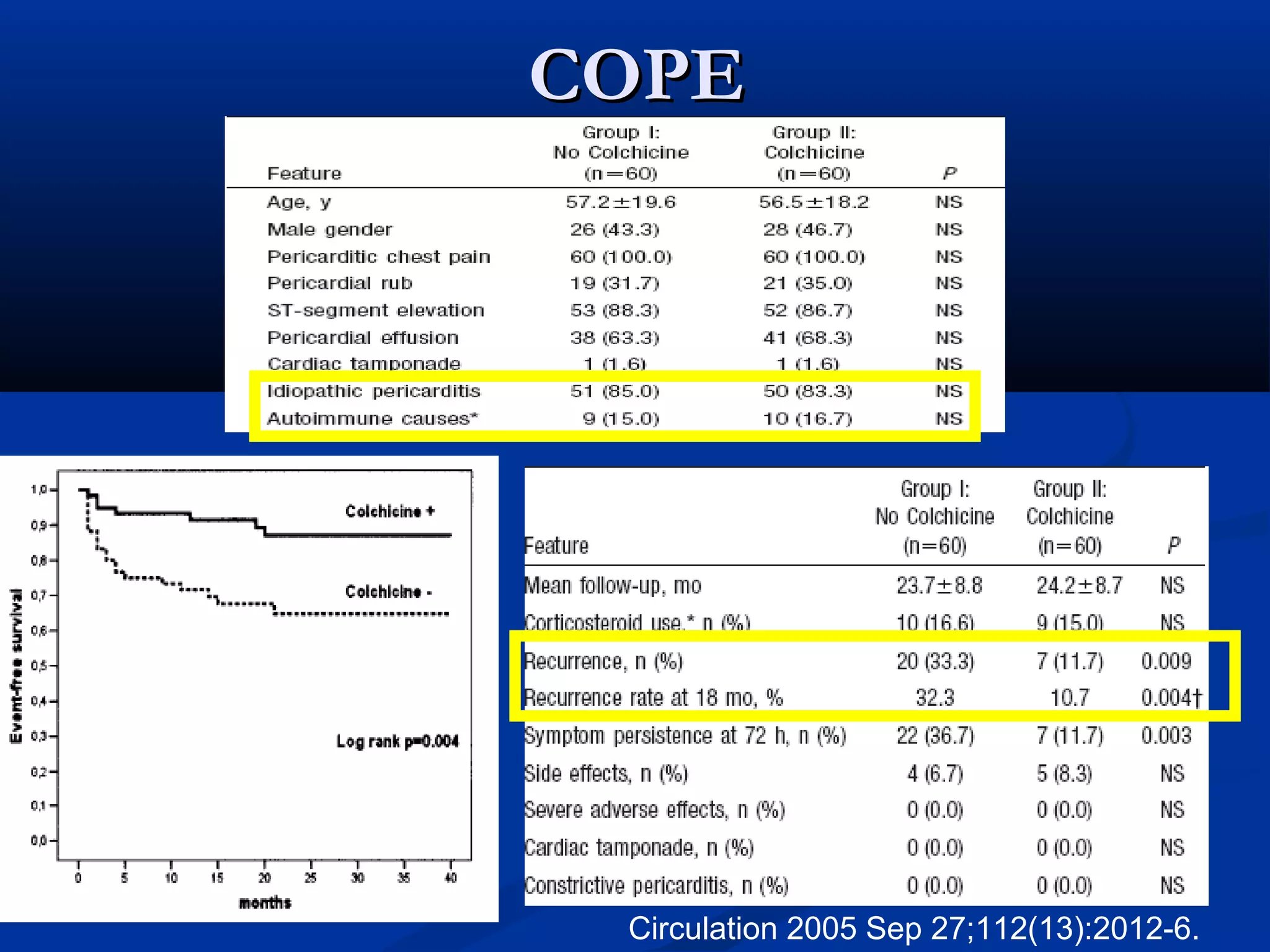
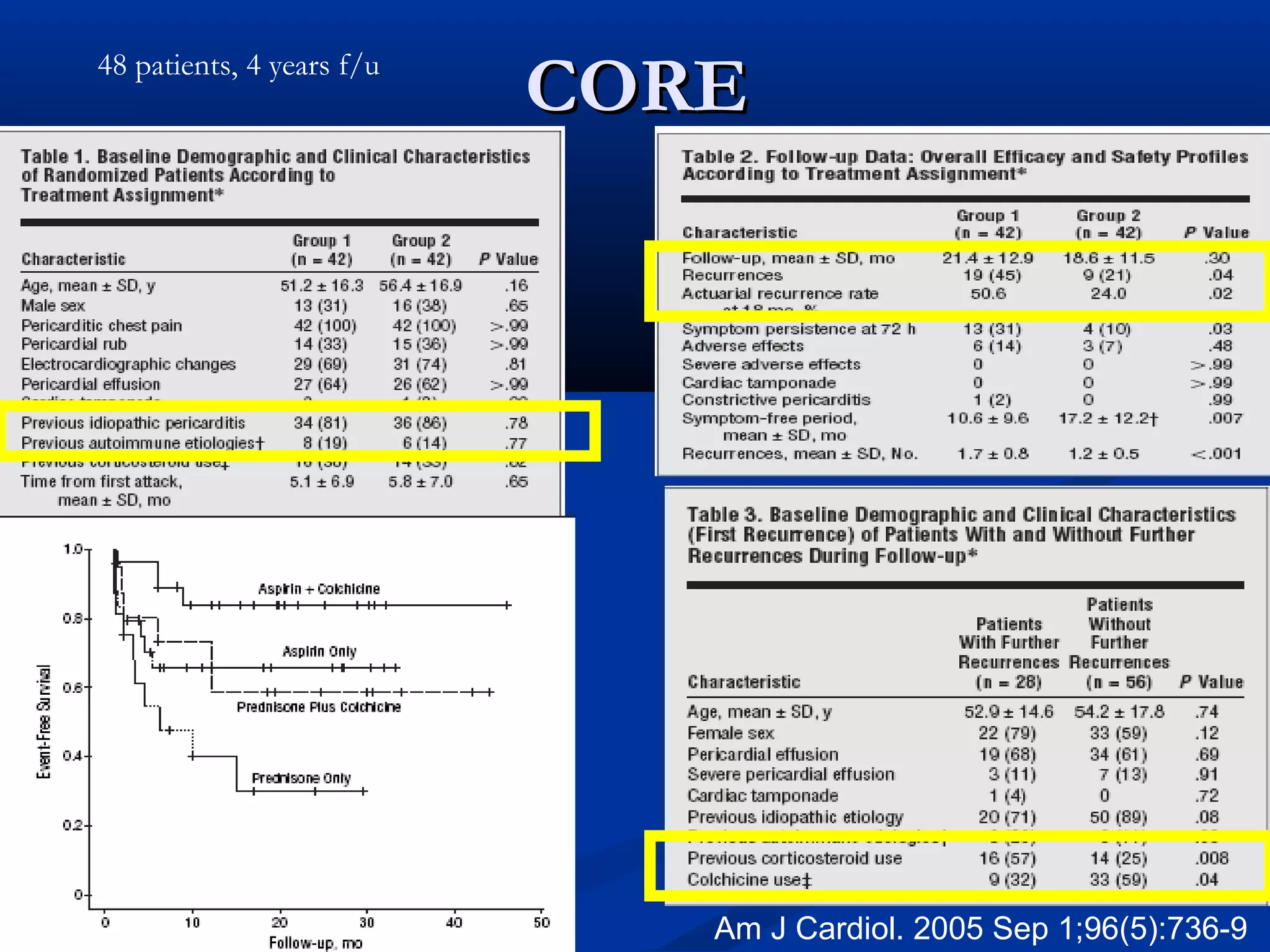
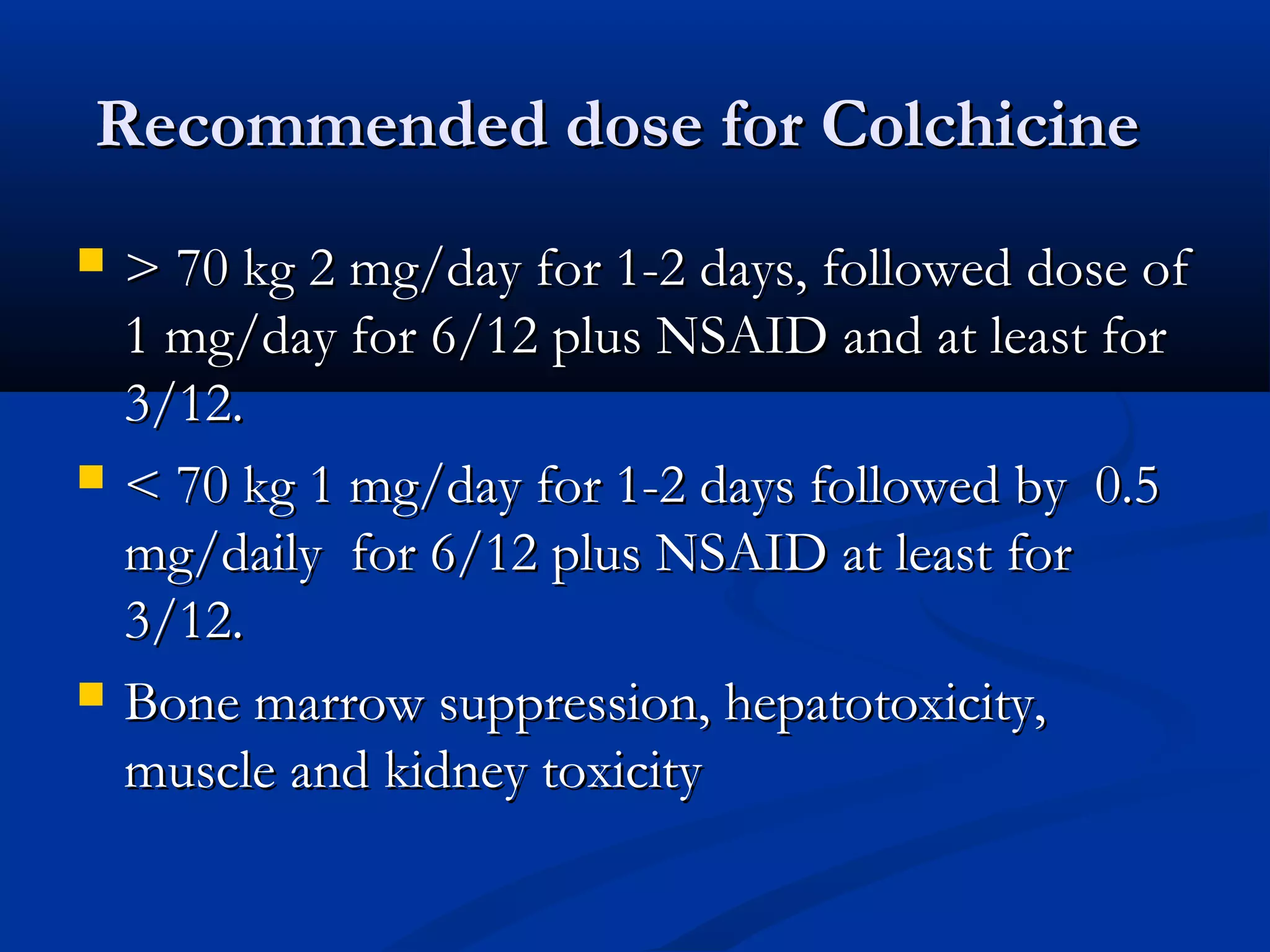
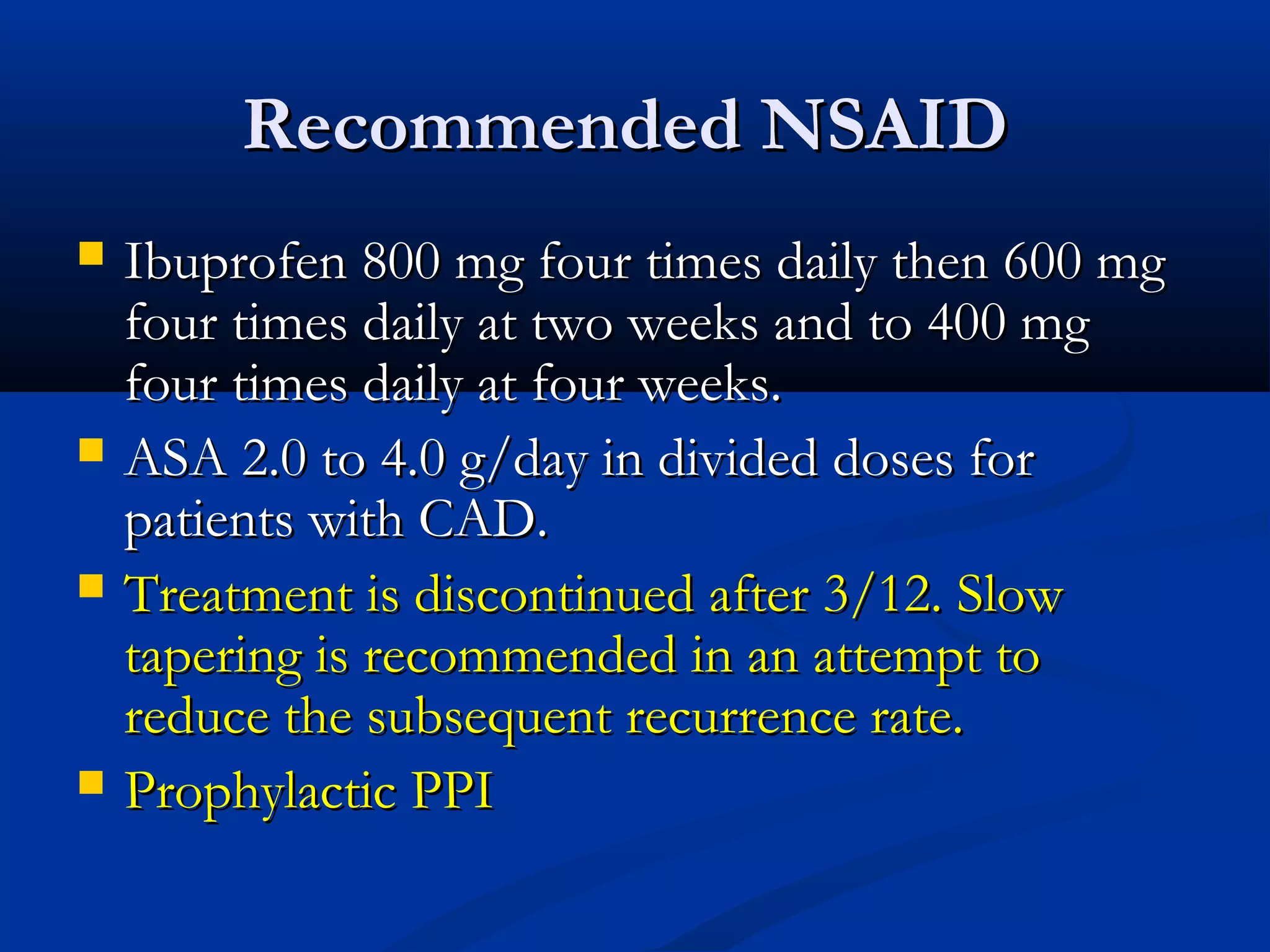
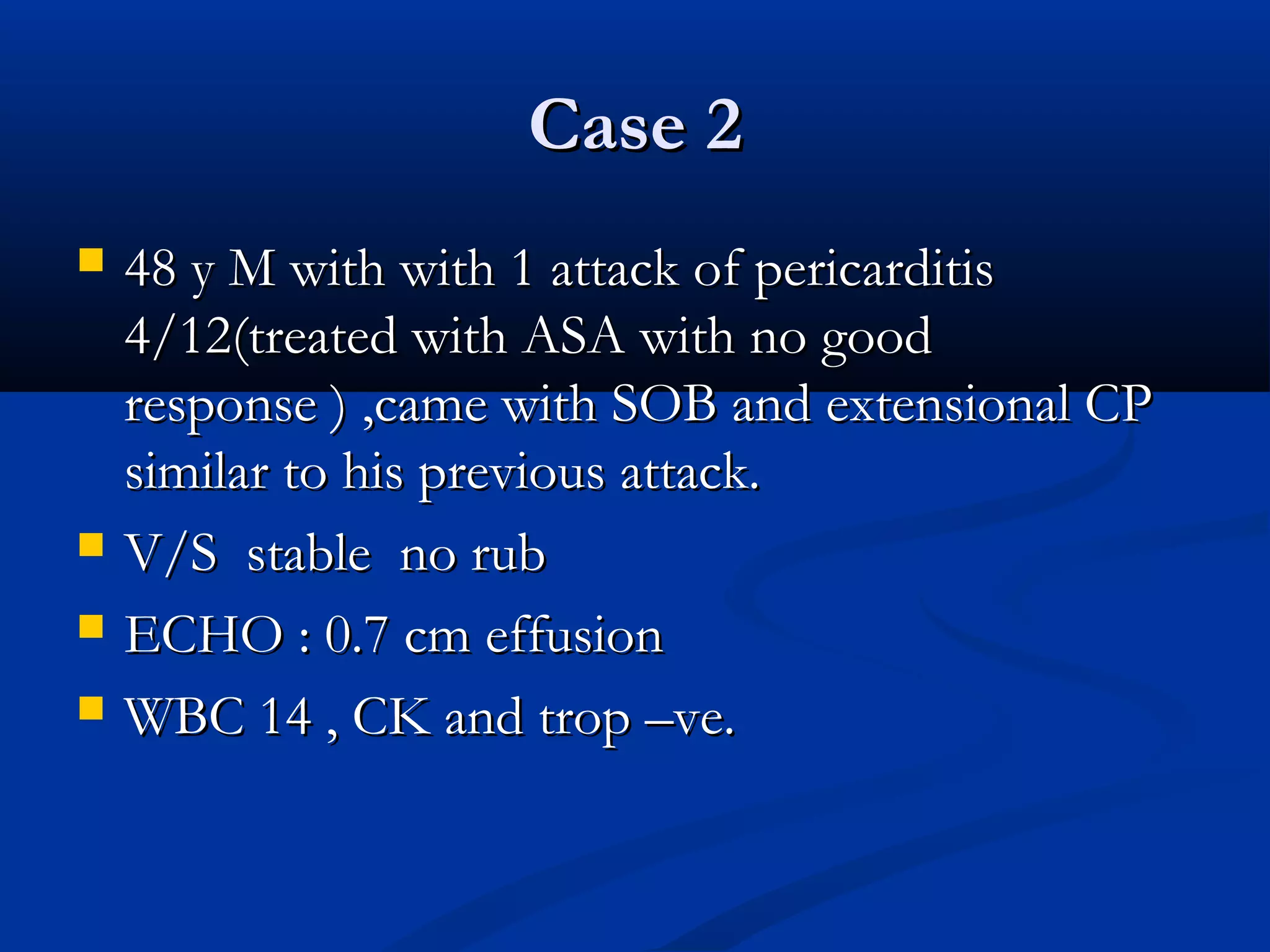
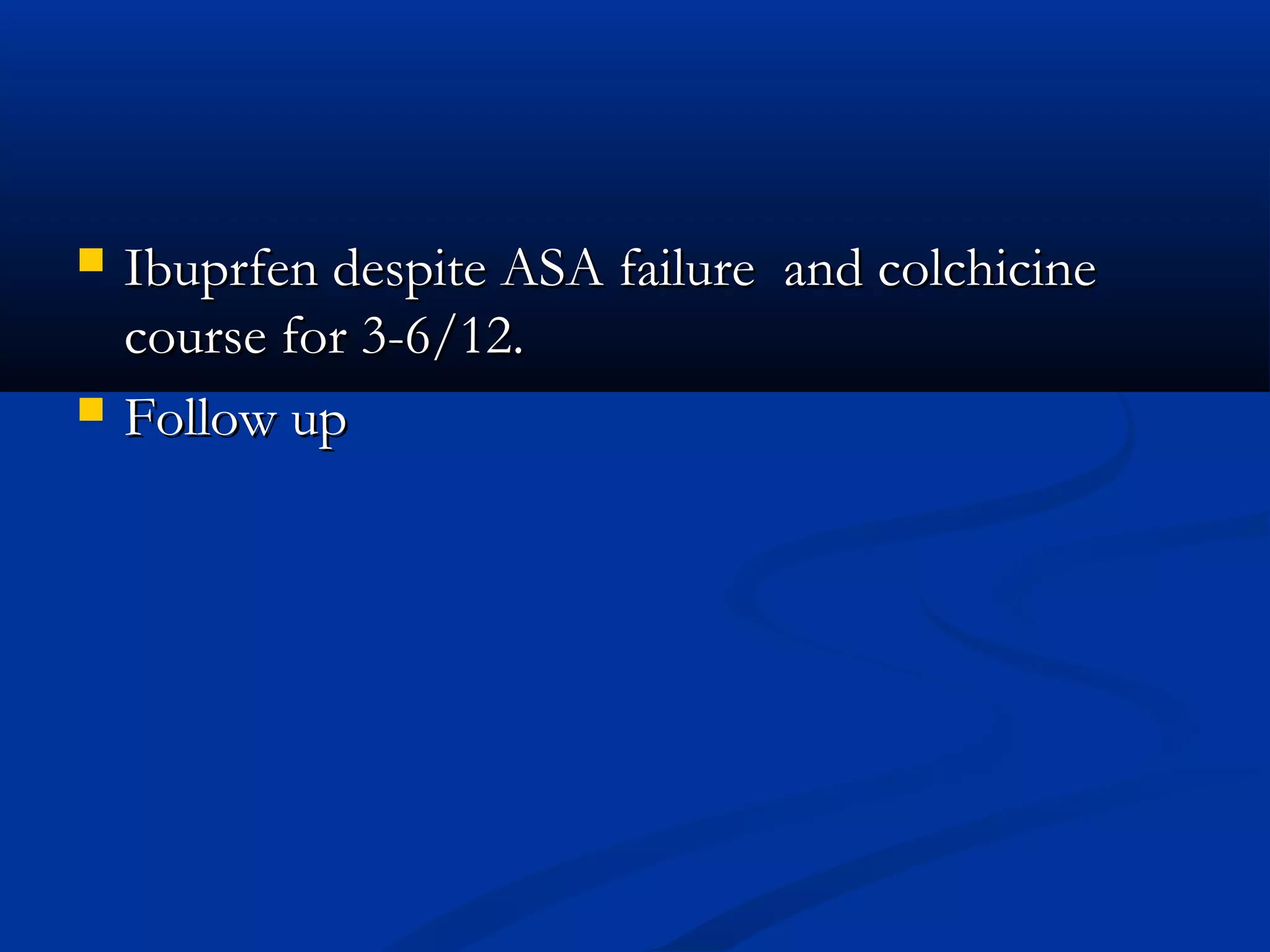
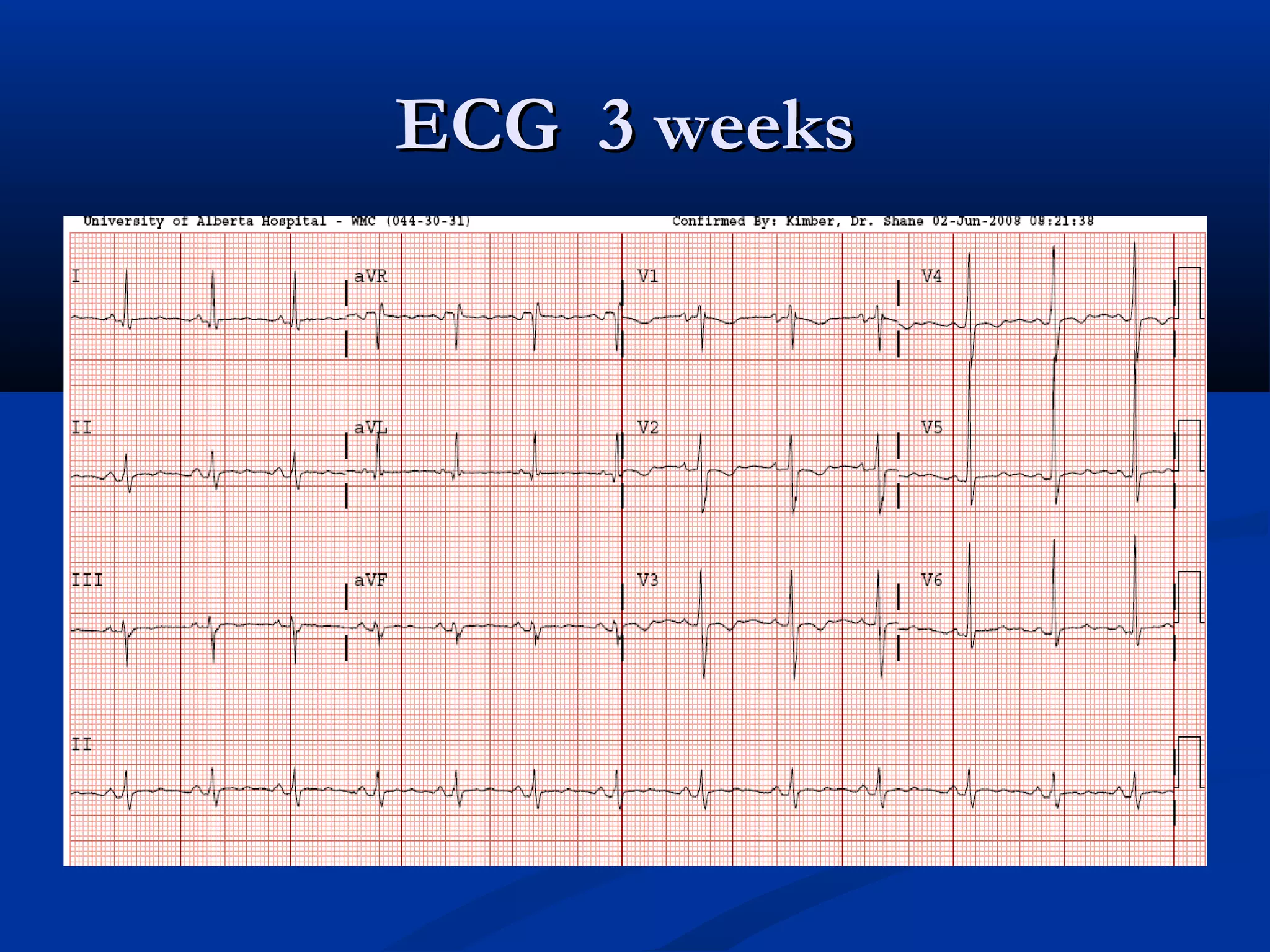
- The second patient is likely recurrent pericarditis given prior treatment failure, and would be treated with ibuprofen and colchicine for 3-6 months with follow up ECG.
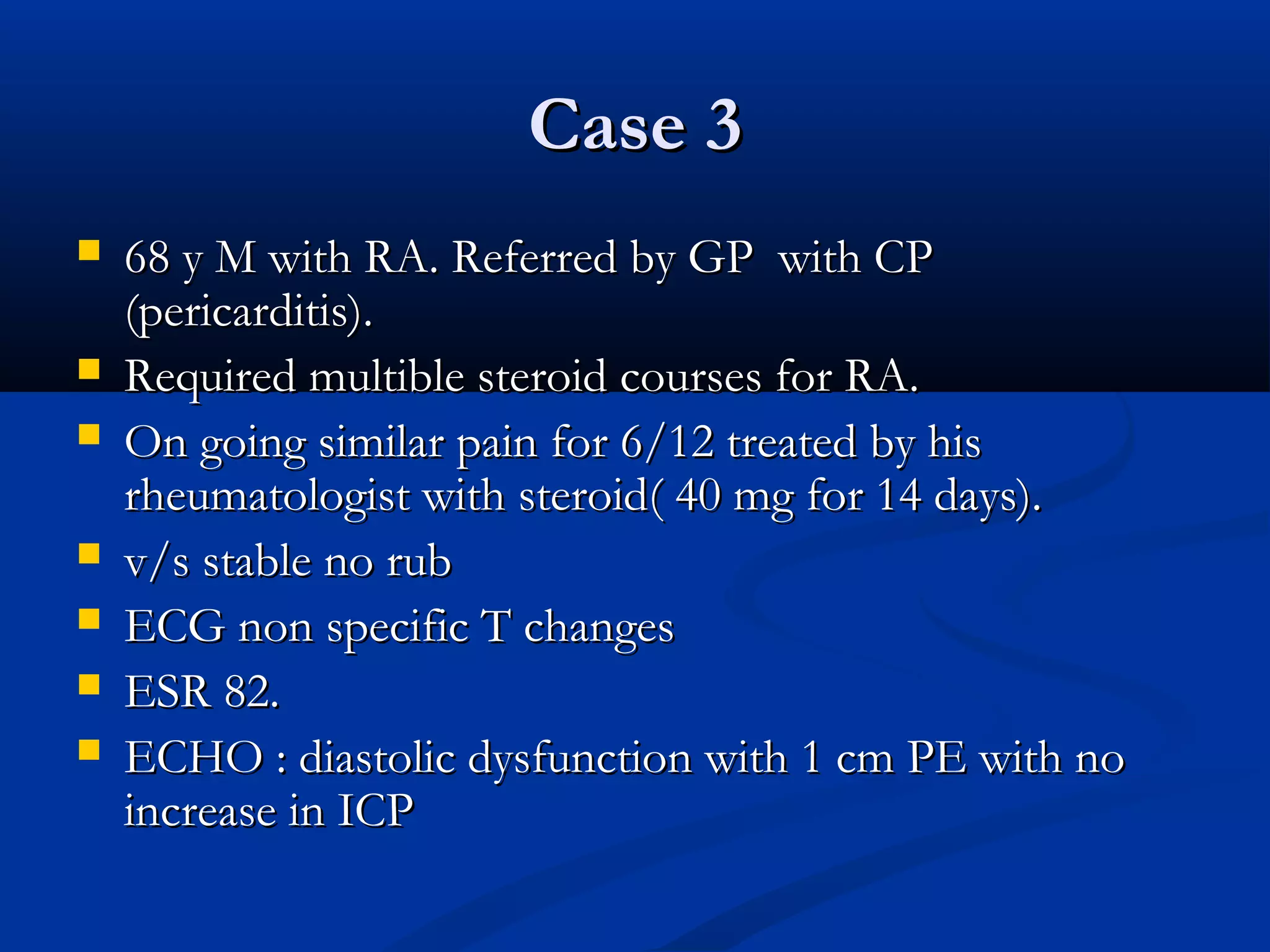
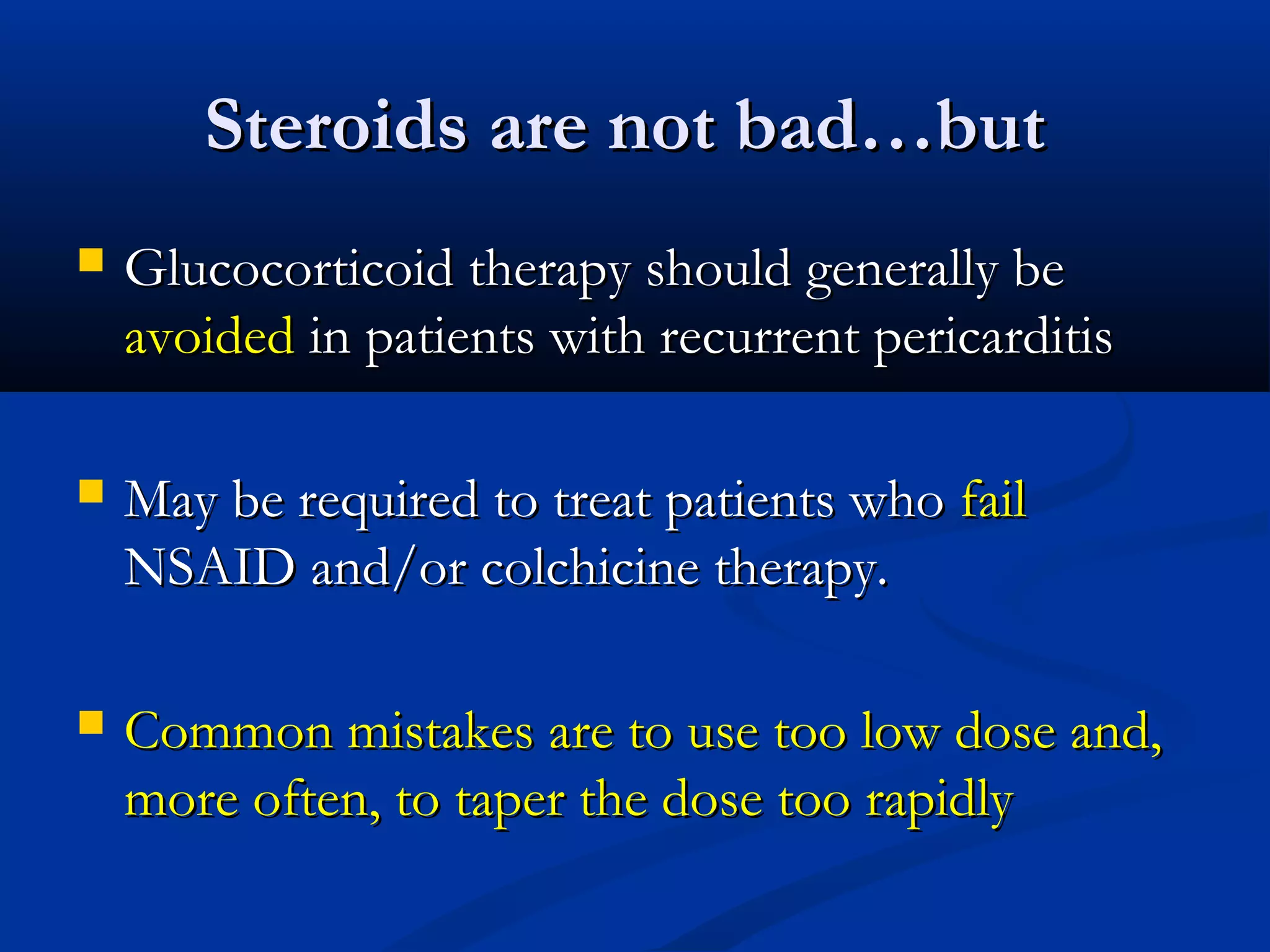
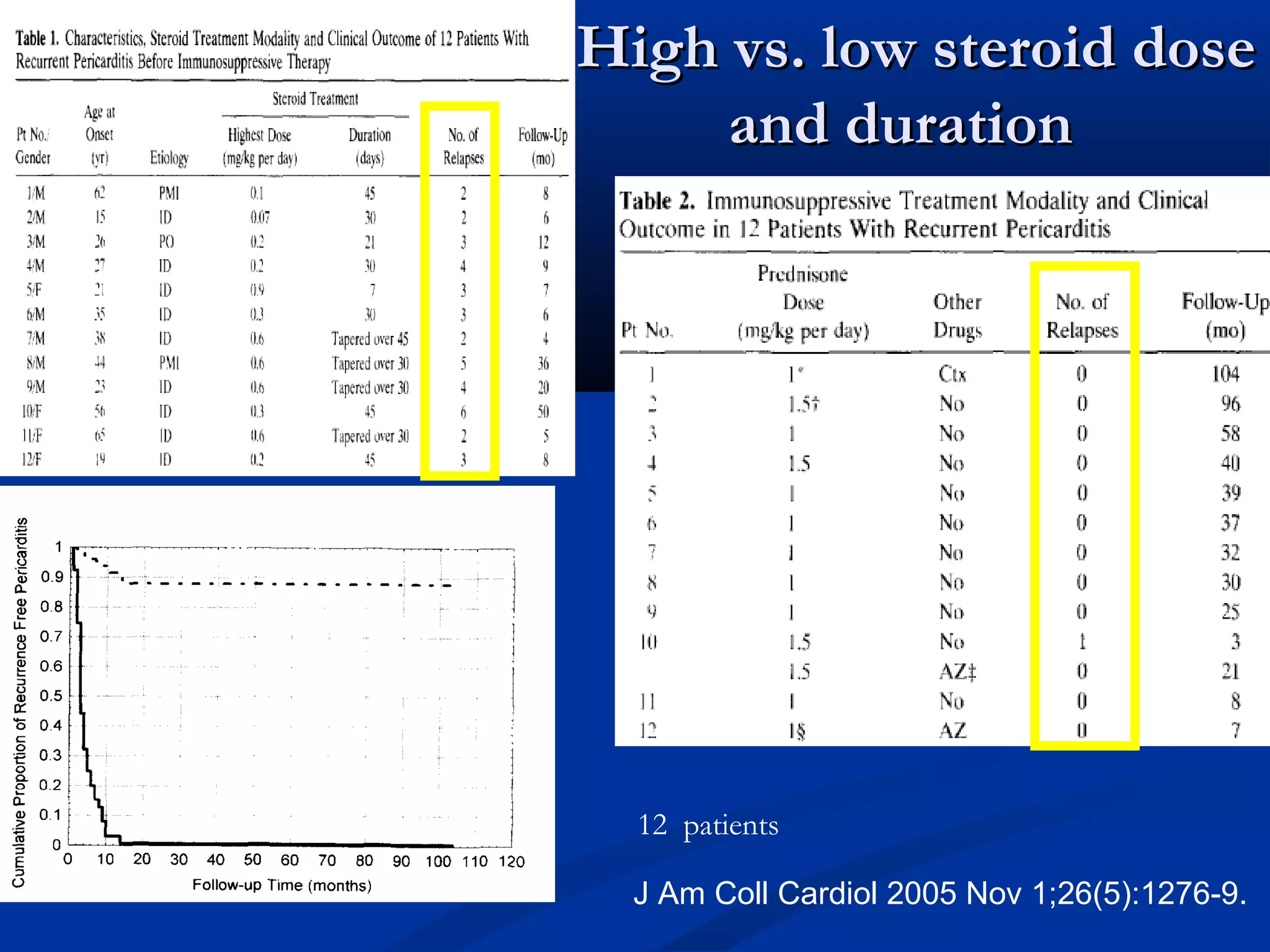
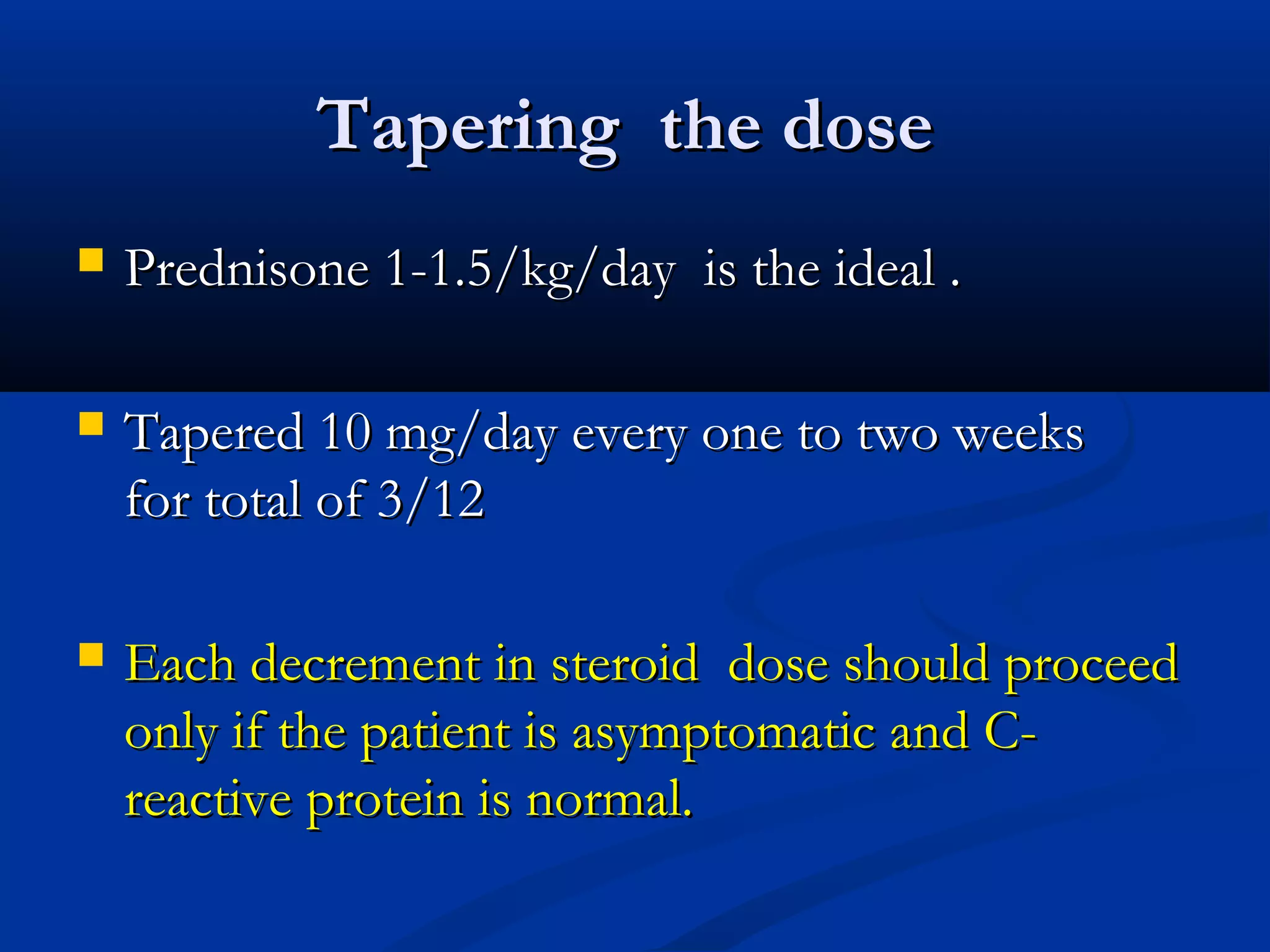
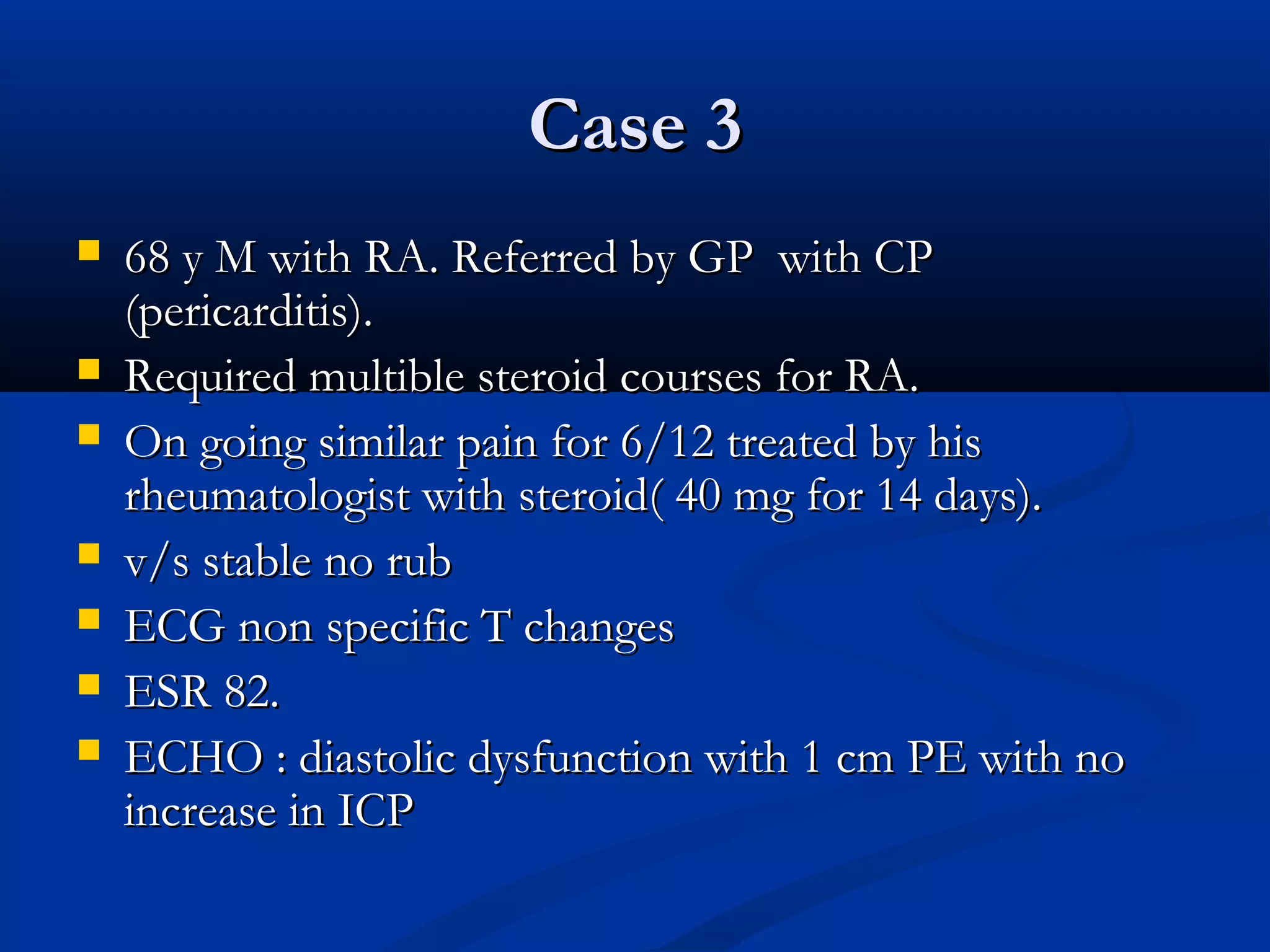
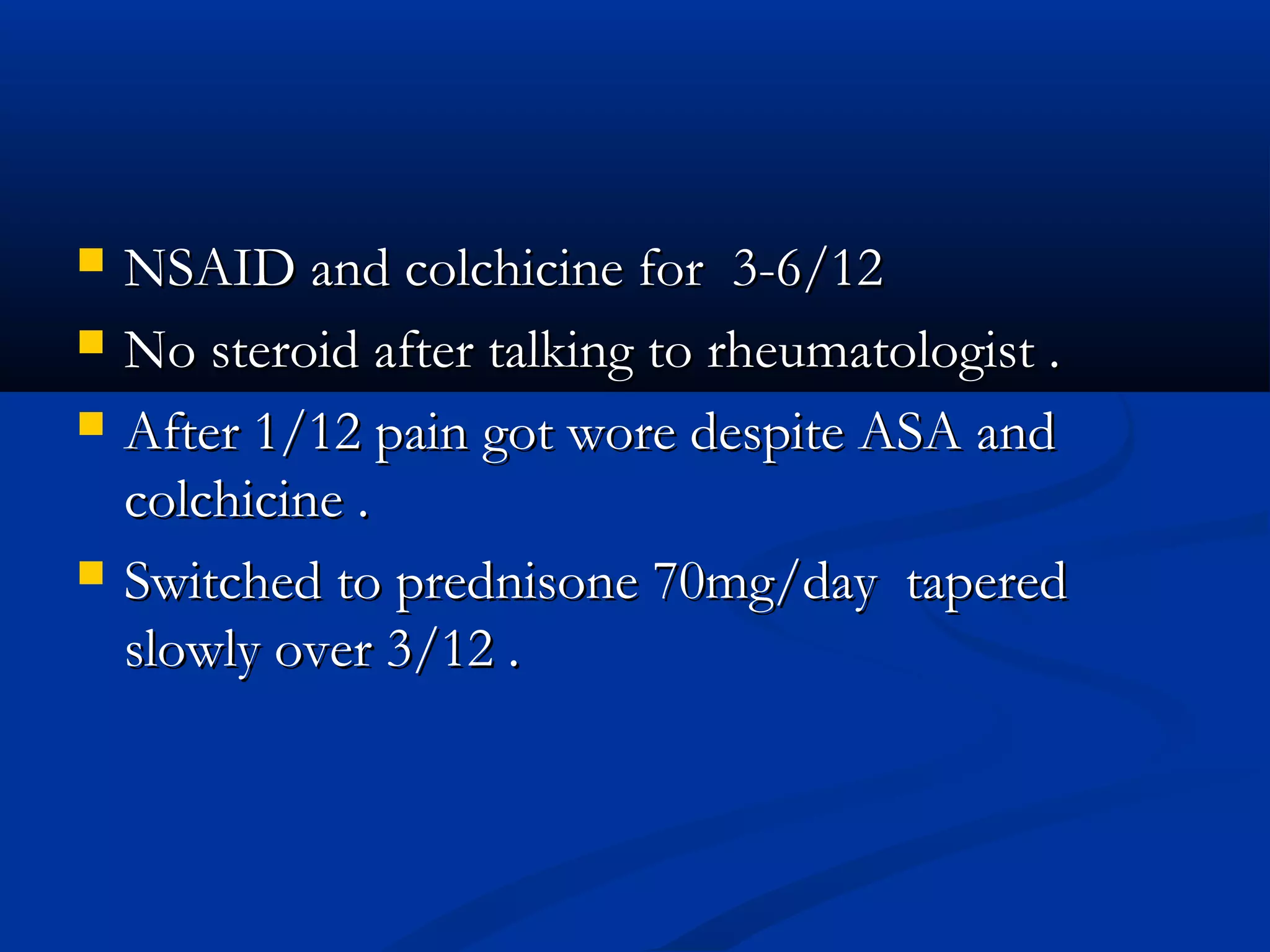
- The third patient has complex medical history of rheumatoid arthritis treated with steroids previously. NSAID and colchicine would be tried initially but steroids may be needed if pain persists after 1 month. Failure of