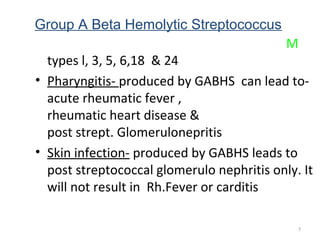
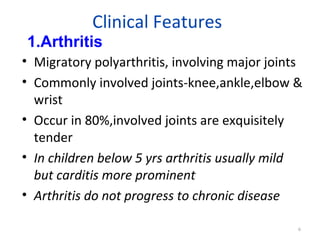
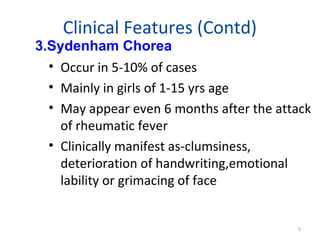
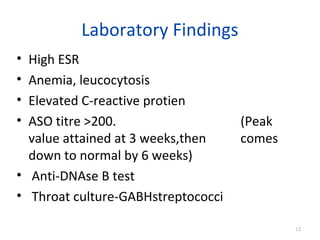
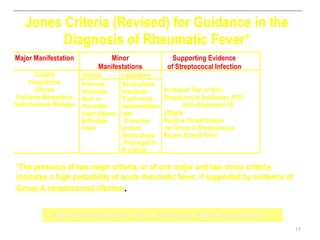
Rheumatic fever is an inflammatory disease that can occur following a streptococcal throat infection. It commonly affects children ages 5-15 and is more prevalent in developing countries. The disease involves the heart, joints, skin, and brain. Diagnosis is based on the modified Jones criteria of major and minor manifestations along with evidence of a prior streptococcal infection. Treatment involves eradicating streptococci, using anti-inflammatory drugs, supportive care, and long-term preventative antibiotics to avoid recurrent attacks. Prognosis depends on factors like age and whether carditis was present initially.