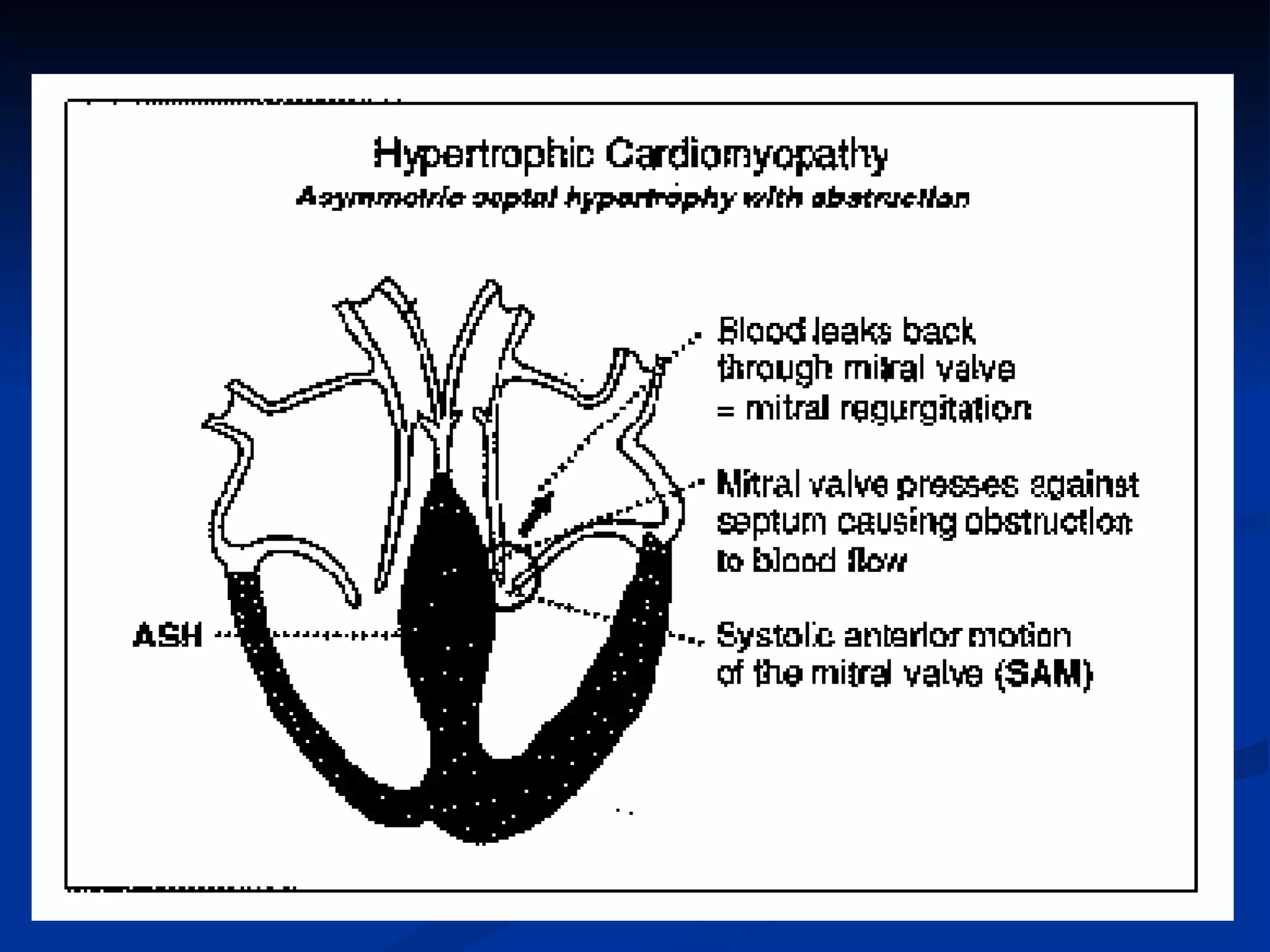
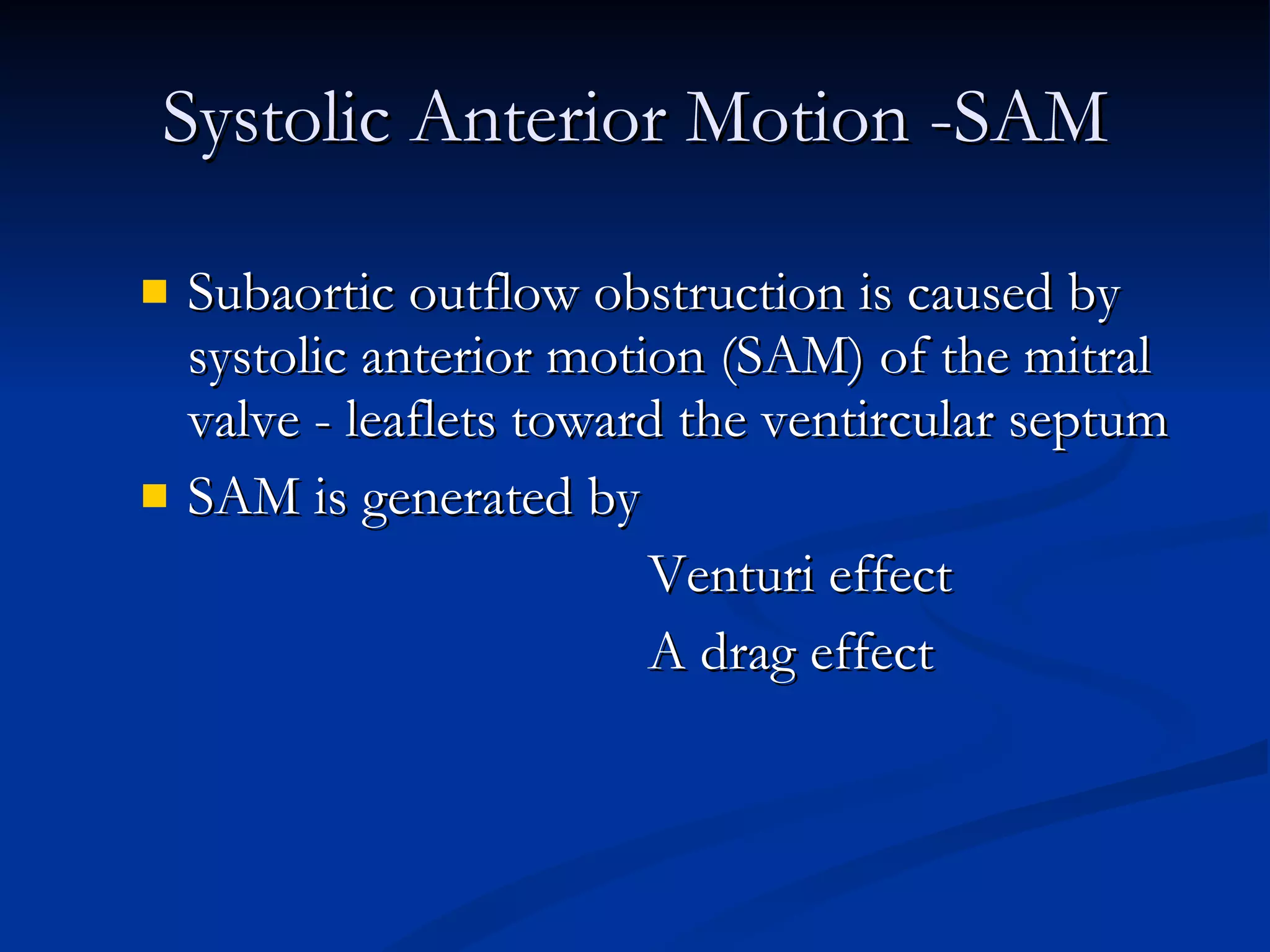
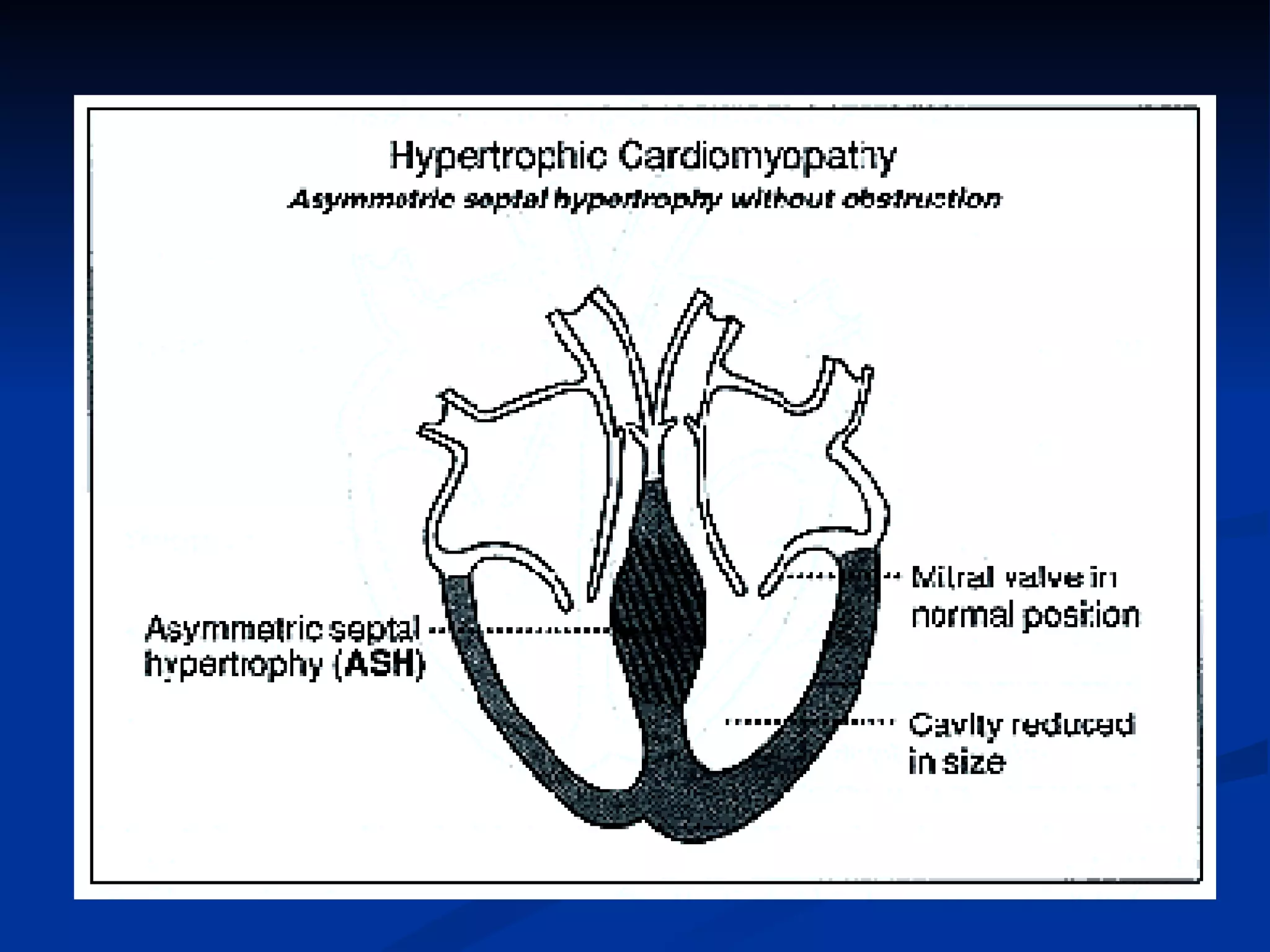
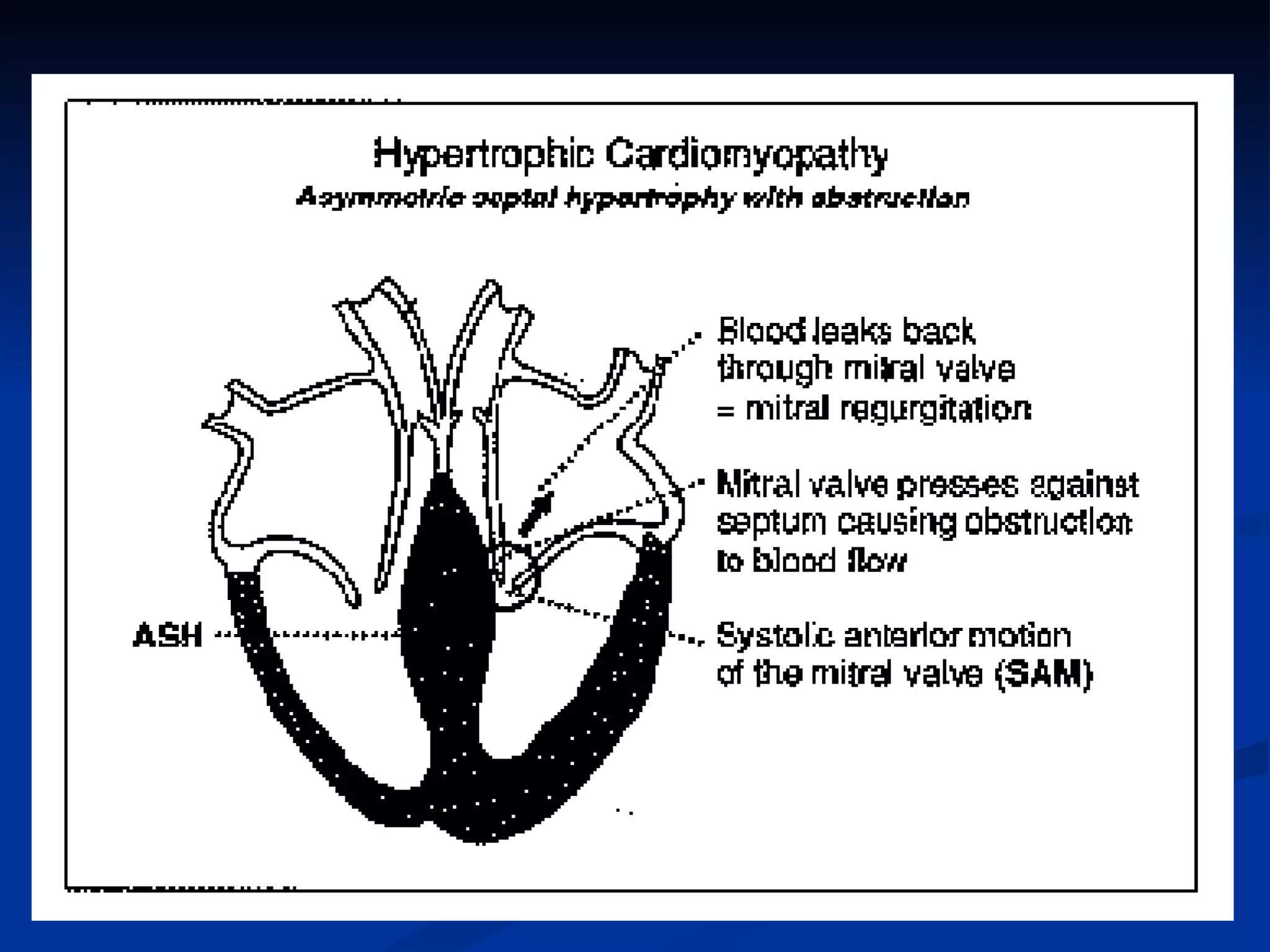
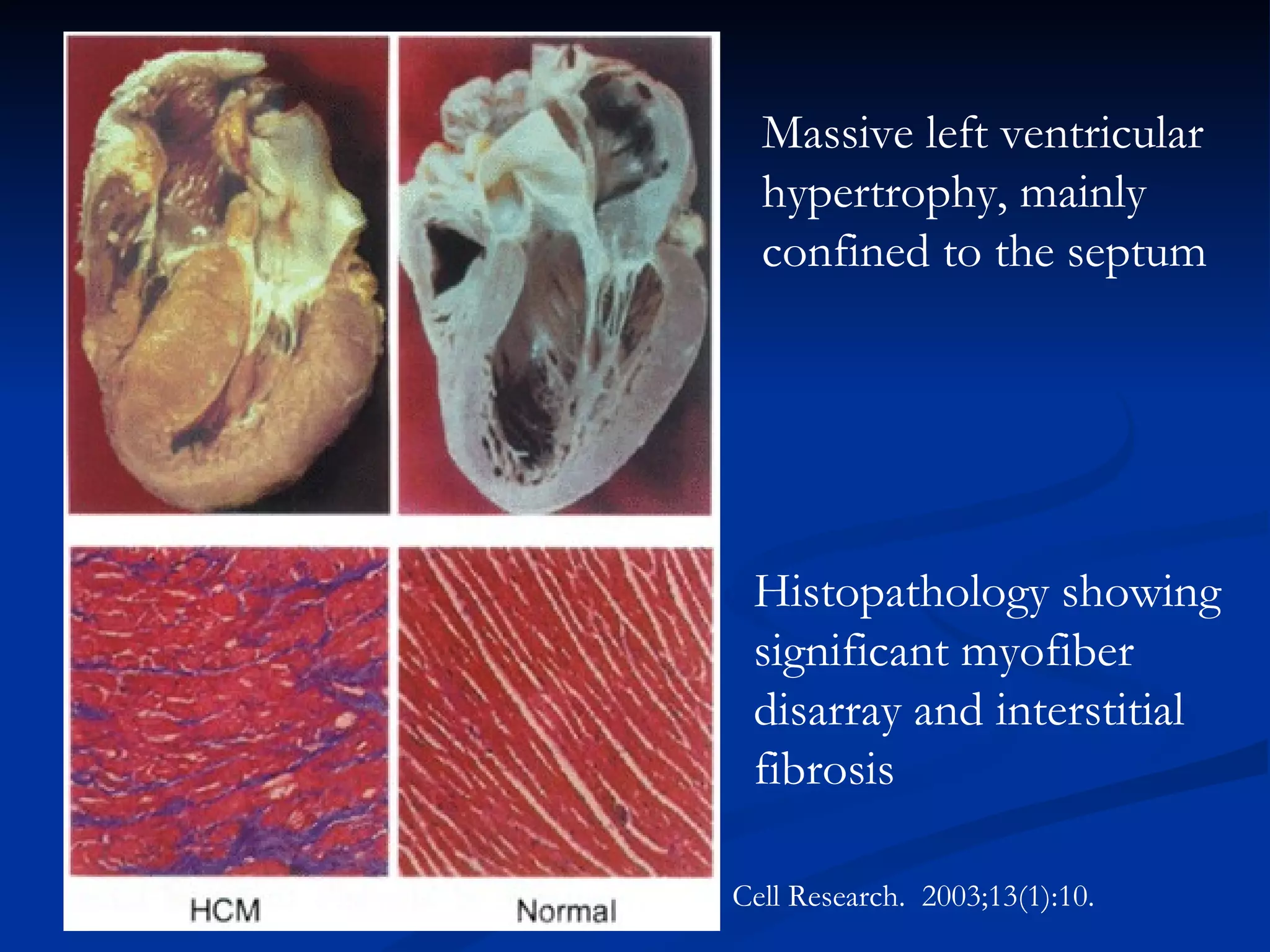
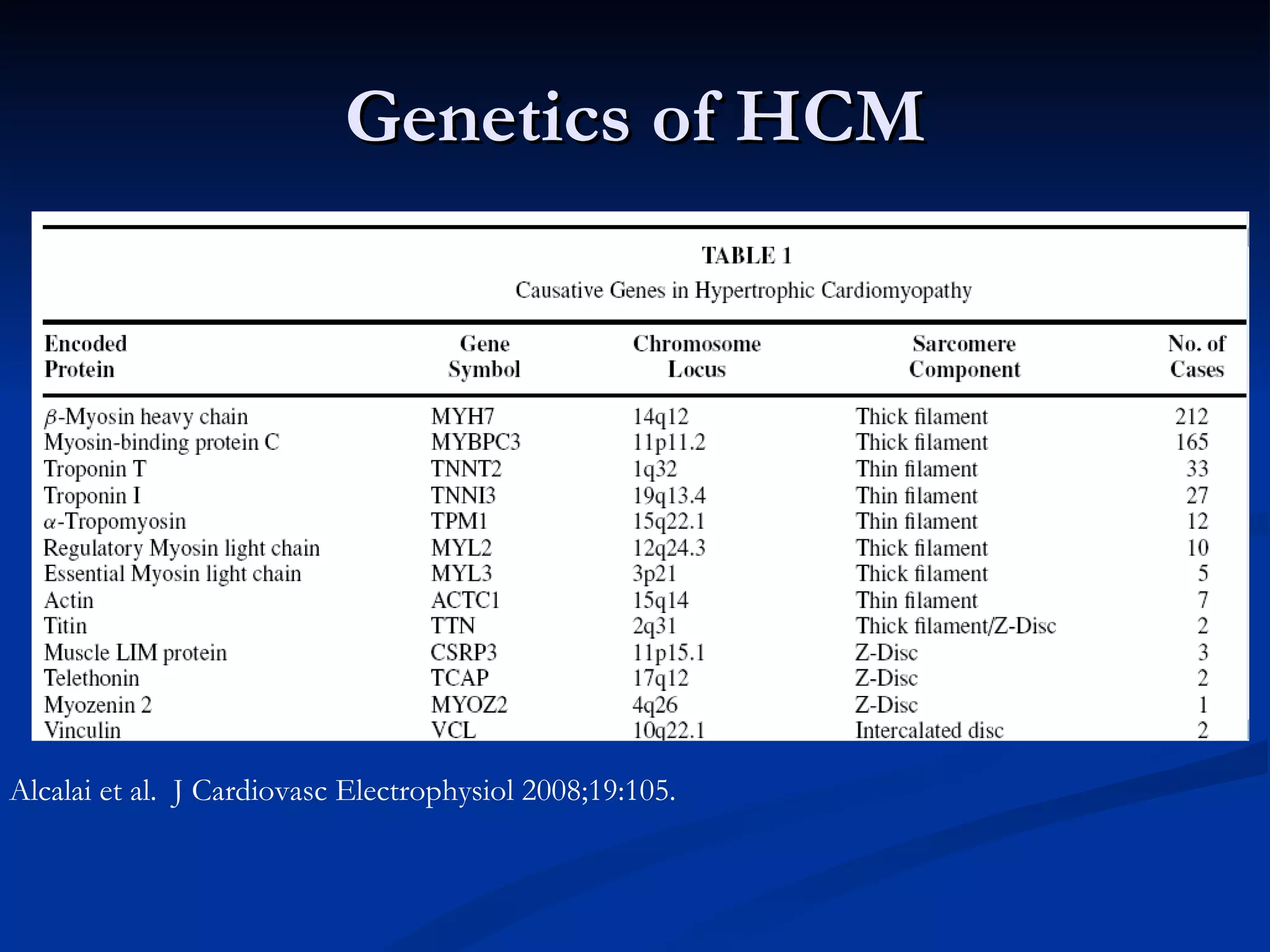
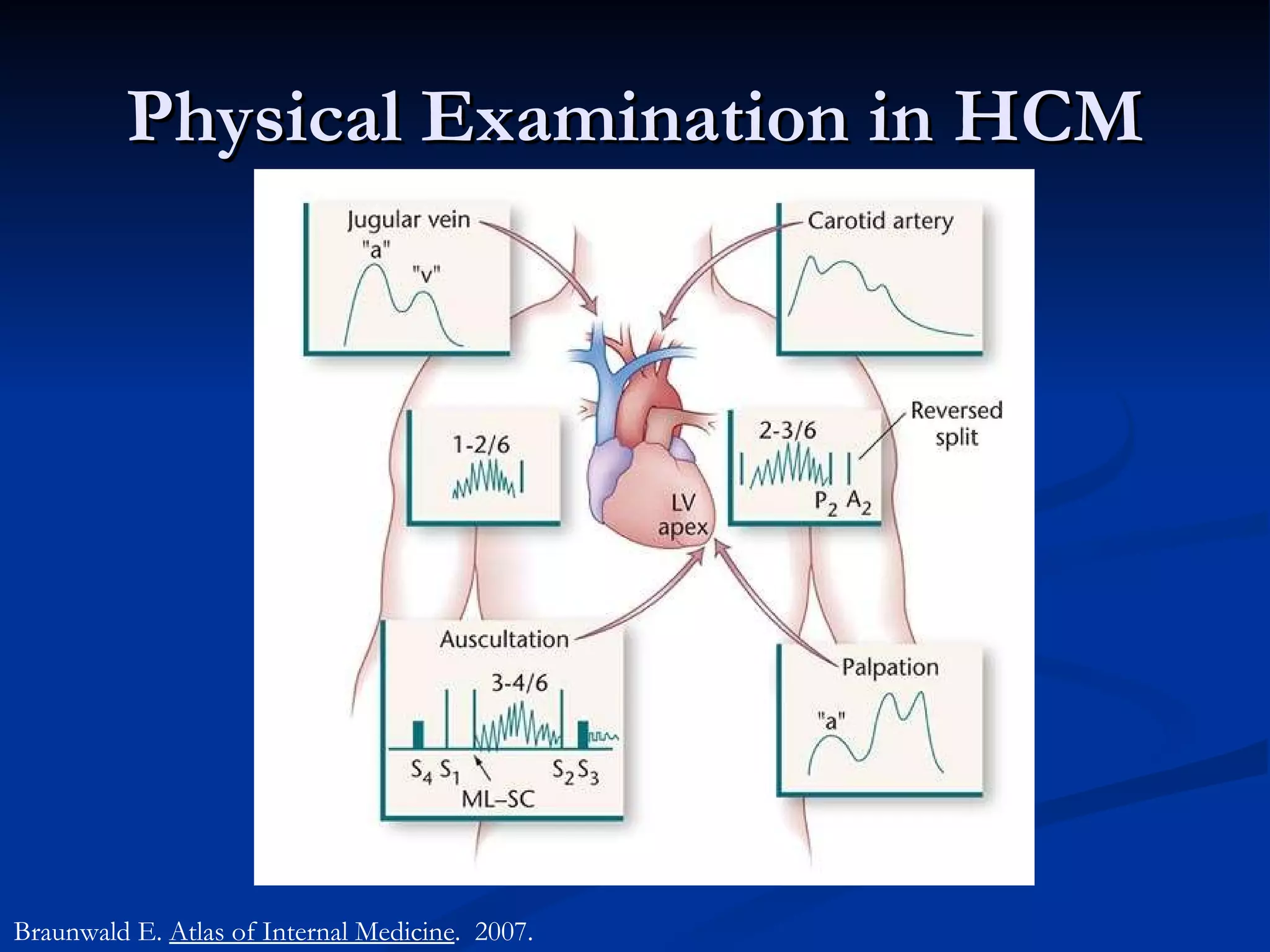
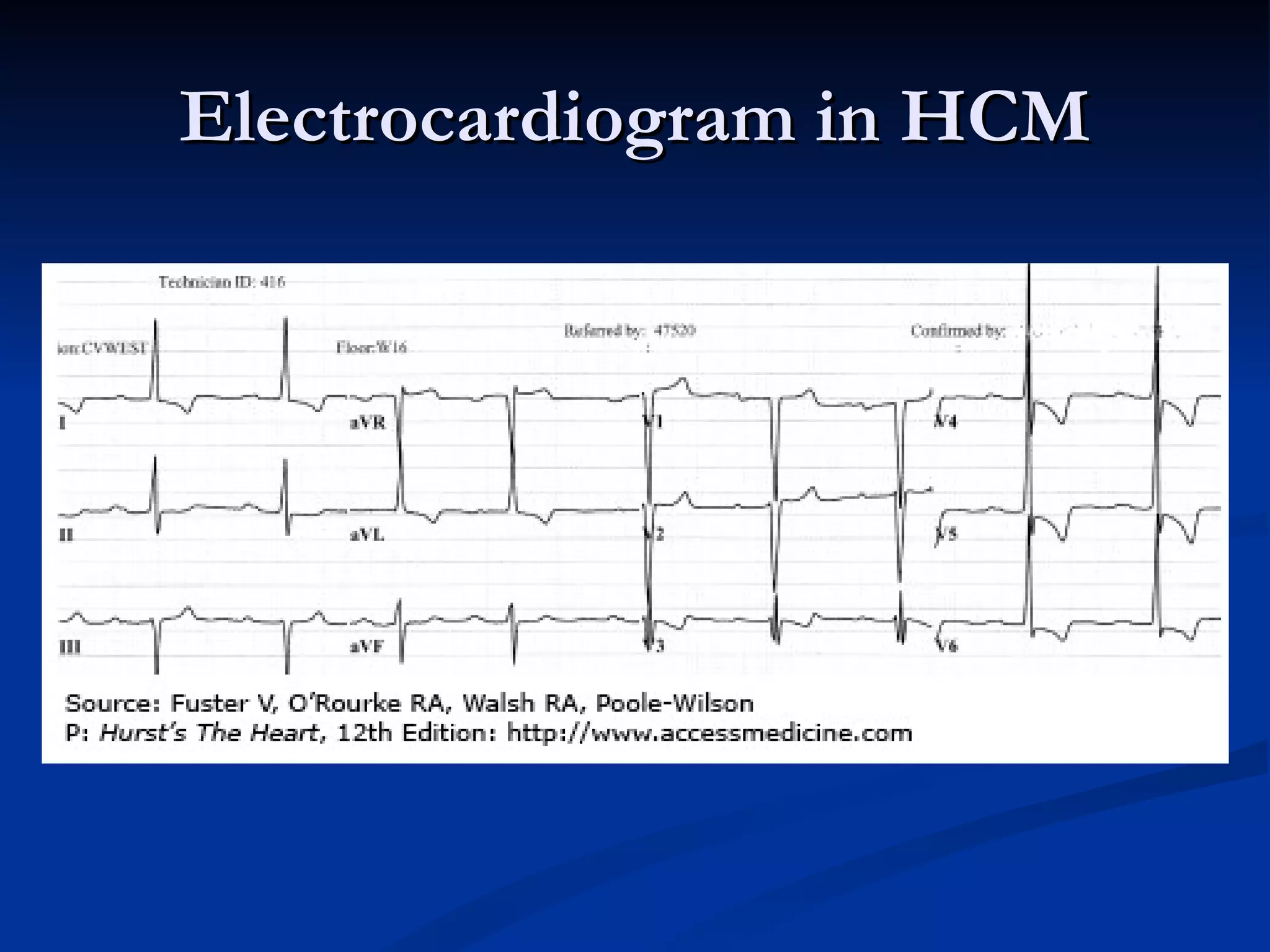
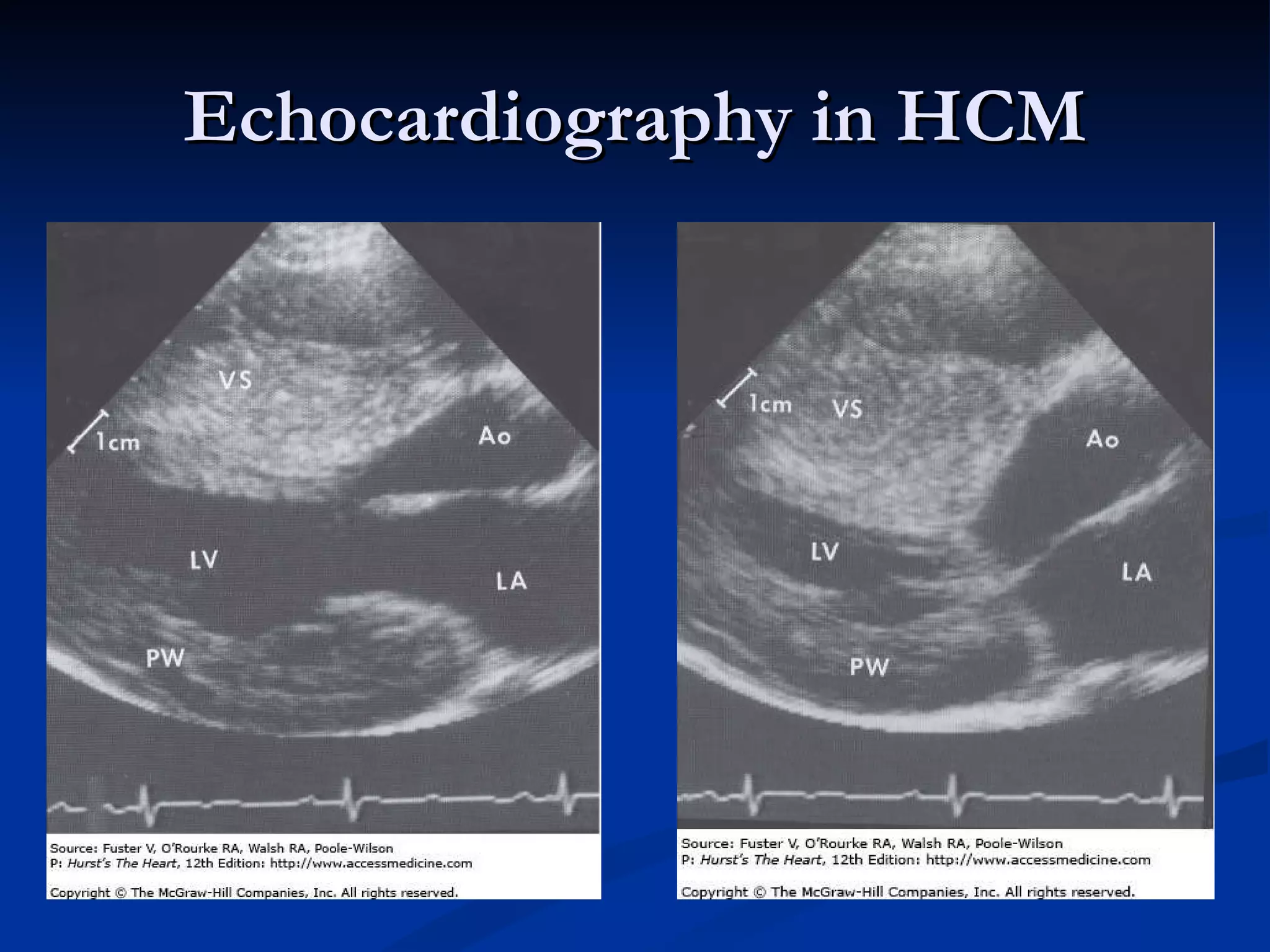
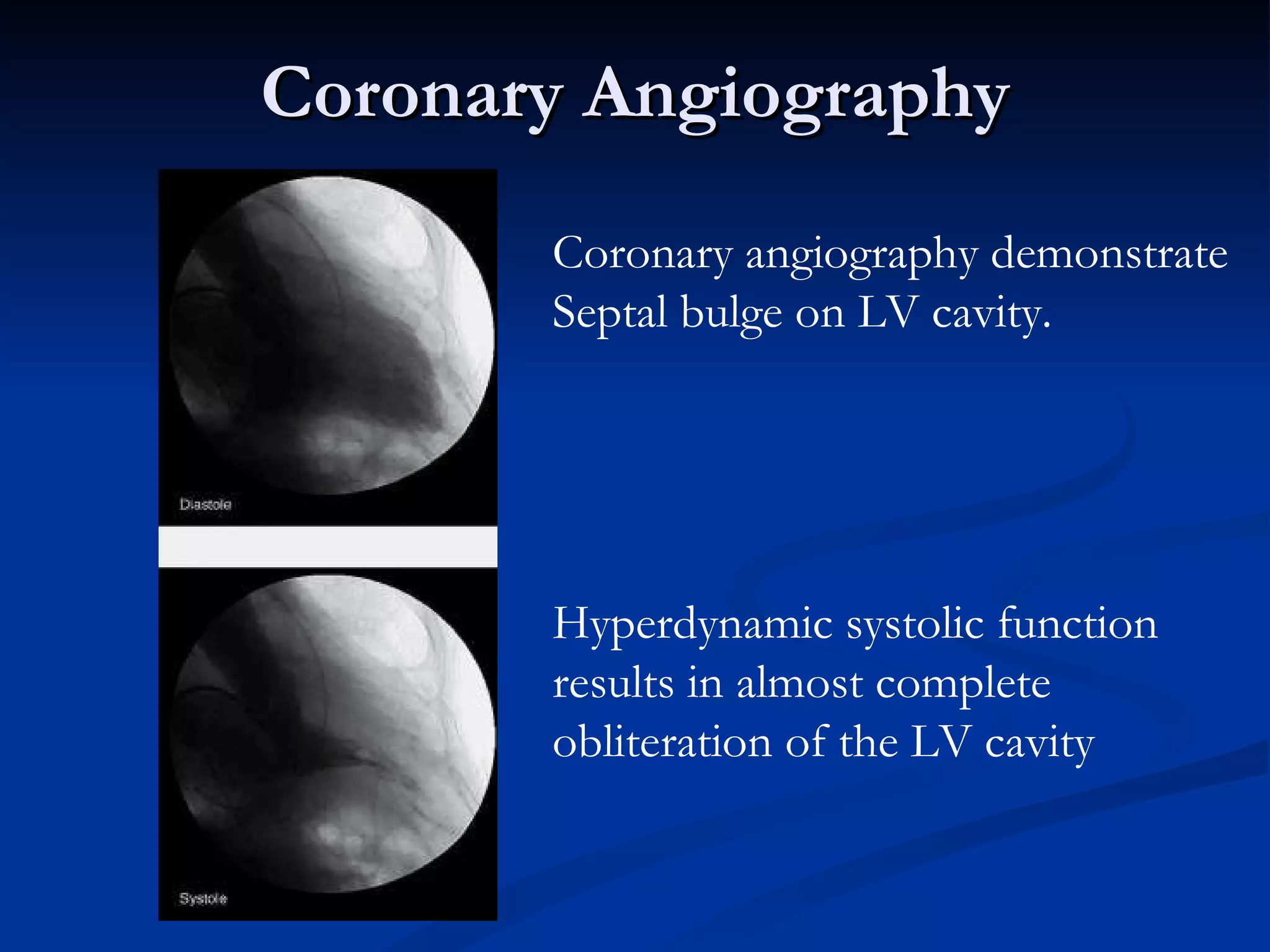
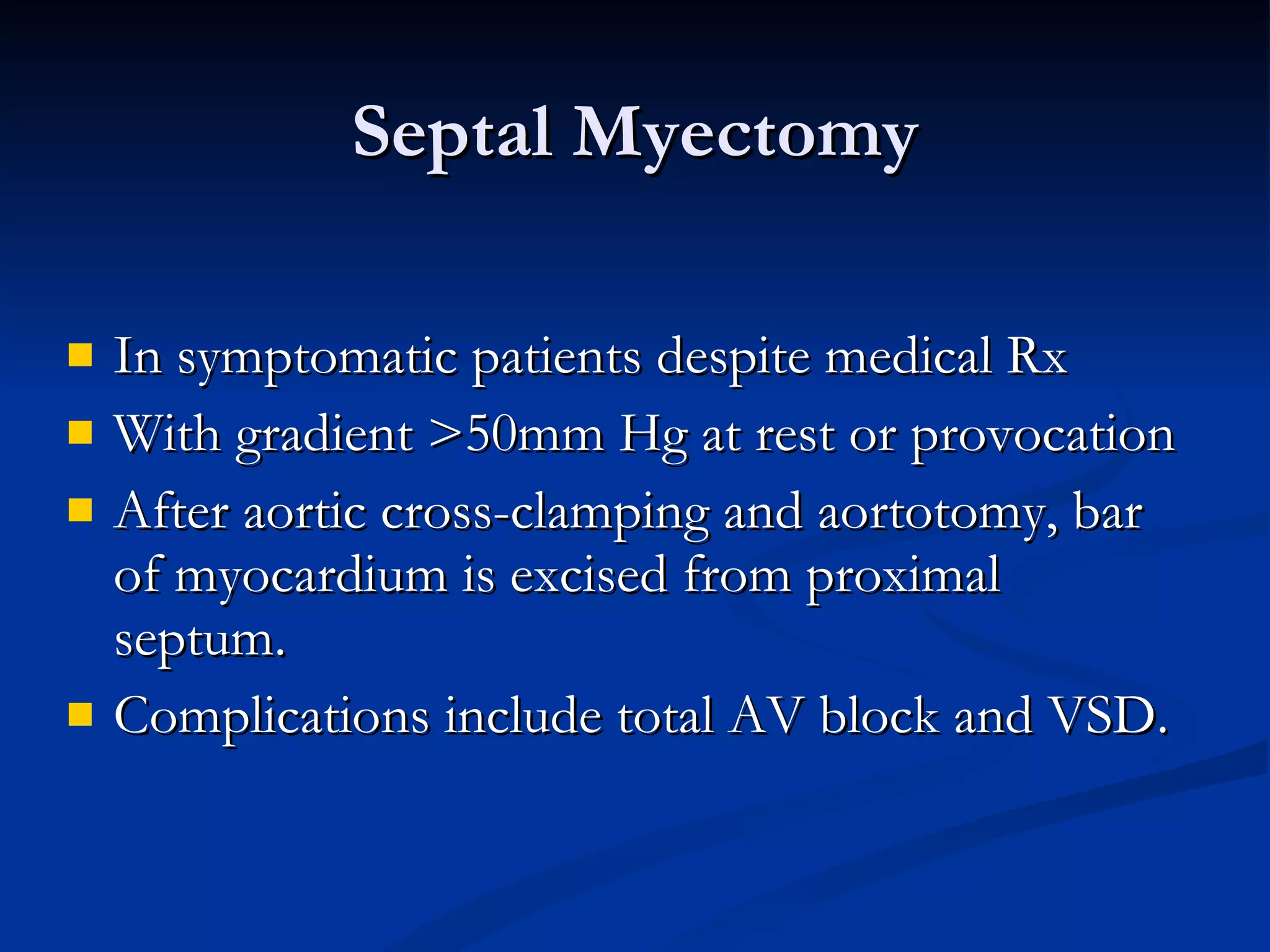
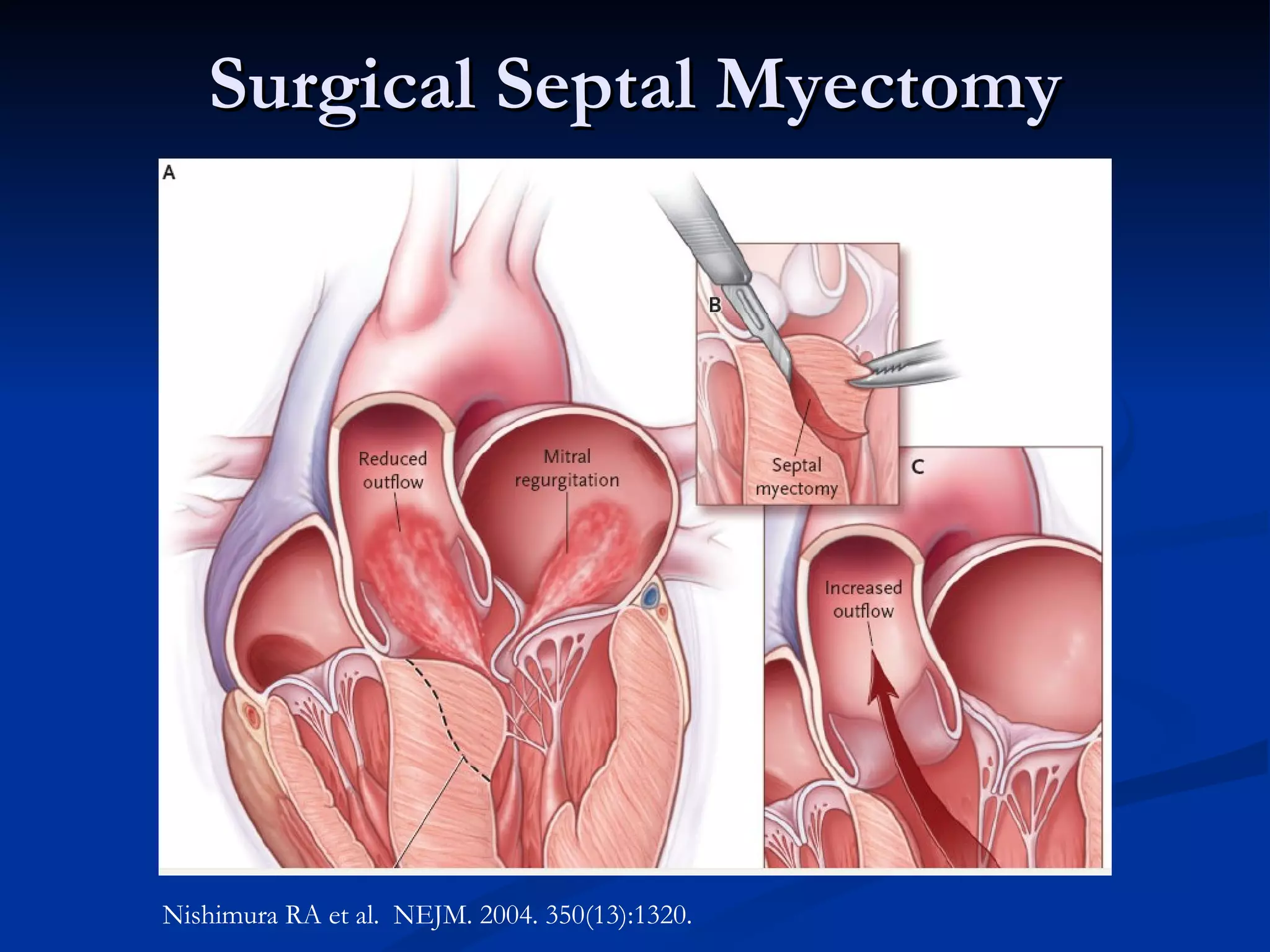
Hypertrophic cardiomyopathy (HCM) is a genetic heart condition characterized by excessive thickening of the heart muscle. It was initially described in the 1950s and causes significant morbidity and mortality due to heart failure, arrhythmias, and sudden cardiac death. The pathophysiology involves left ventricular outflow tract obstruction, diastolic dysfunction, myocardial ischemia, and mitral regurgitation. Treatment involves medications, septal reduction procedures like myectomy or alcohol ablation, and implantable cardioverter-defibrillators in high-risk patients. Prognosis depends on symptom severity and risk factors for sudden cardiac death.