Three sentences:
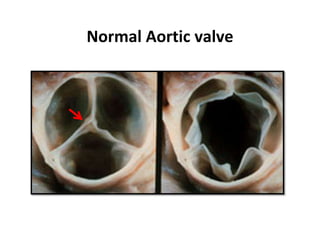
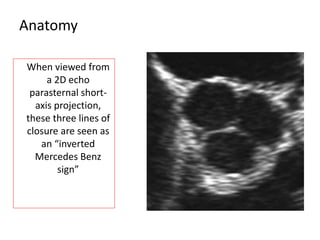
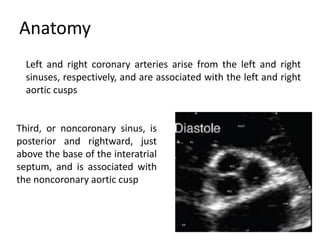
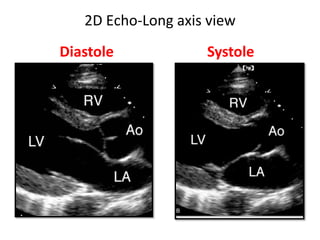
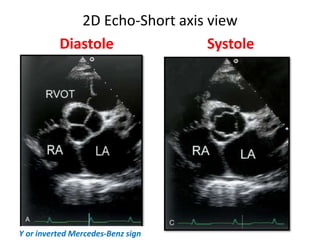
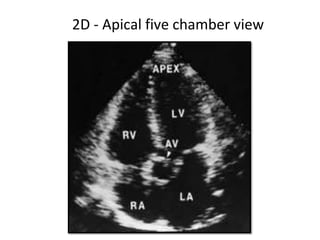
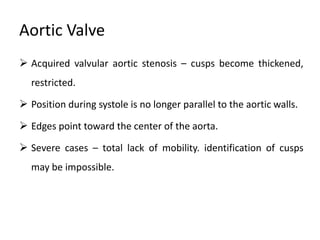
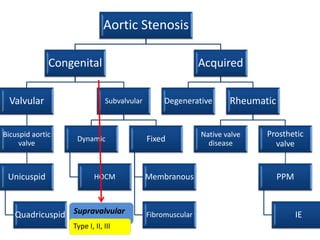
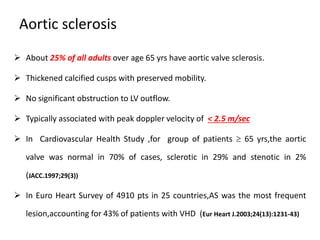
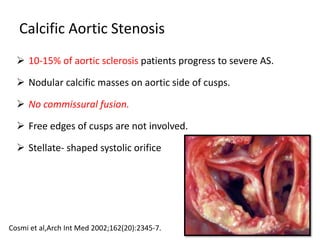
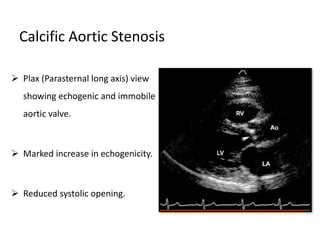
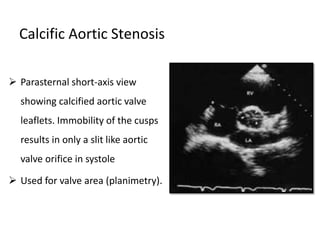
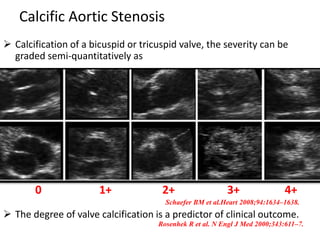
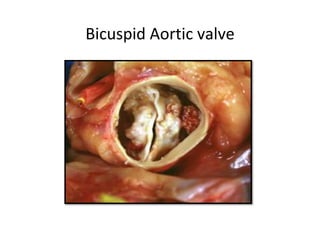
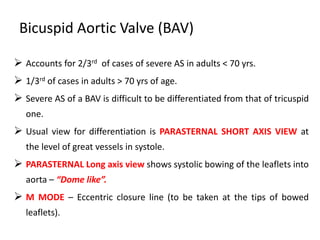
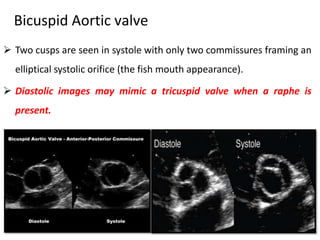
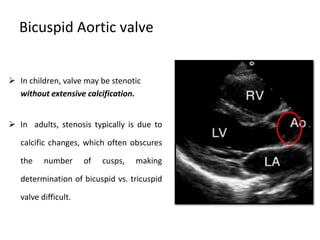
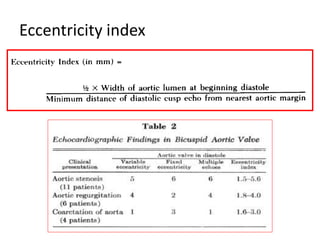
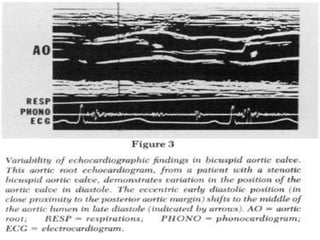
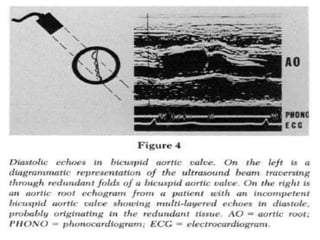
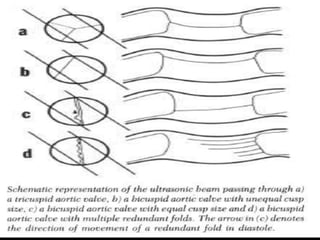
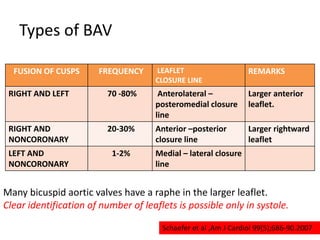
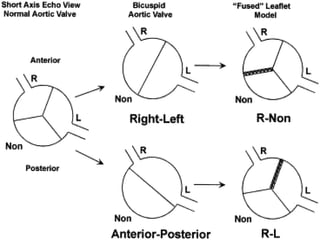
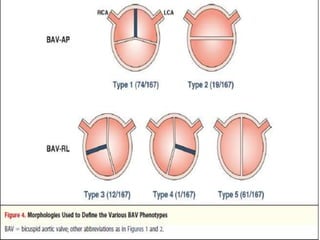
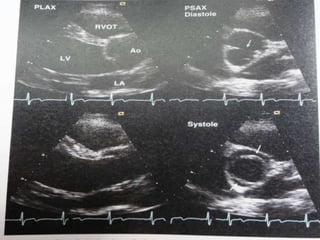
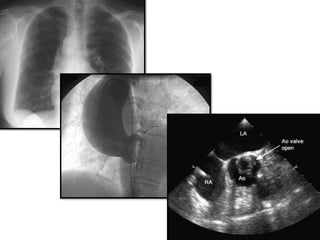
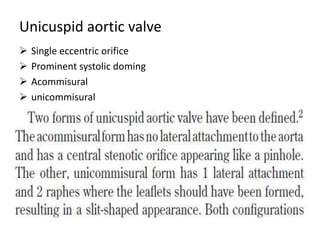
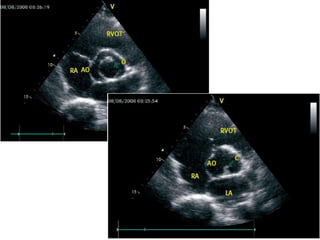
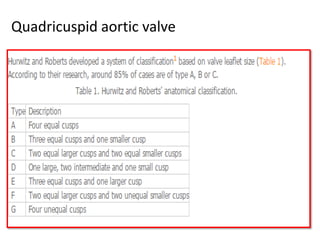
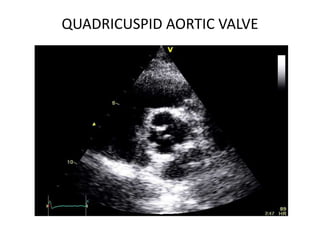
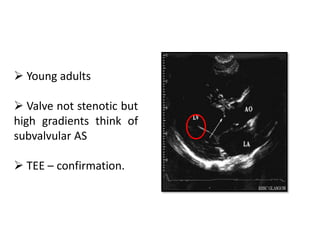
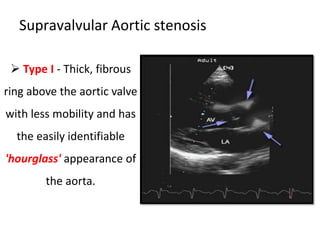
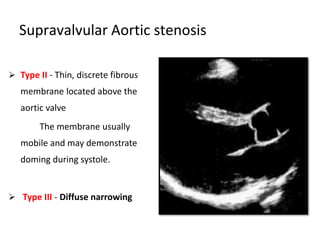
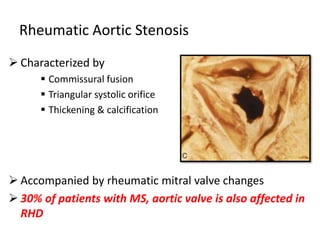
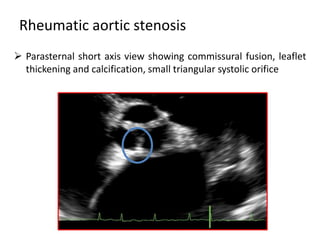
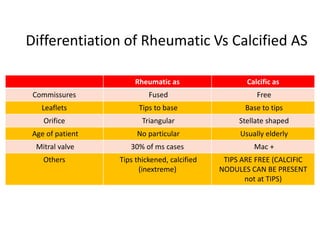
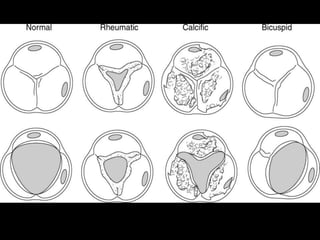
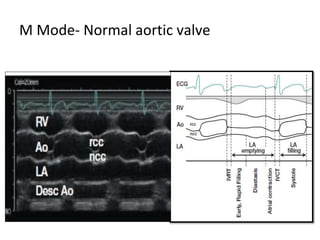
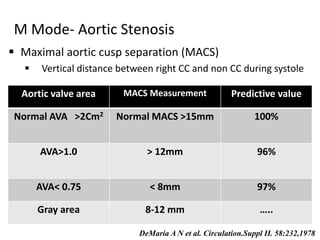
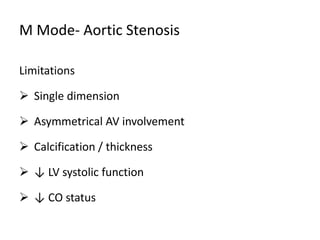
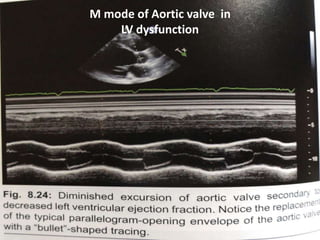
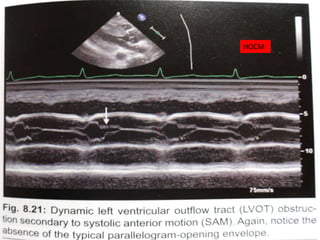
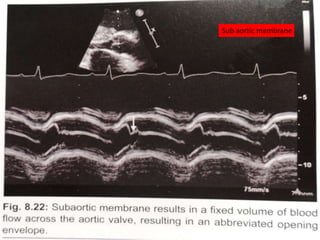
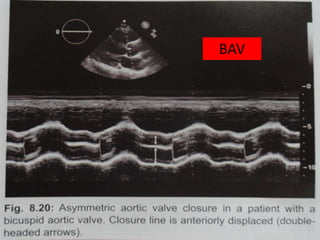
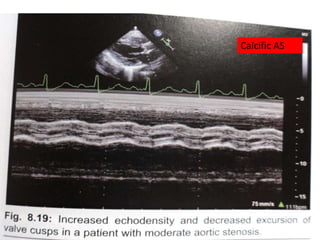
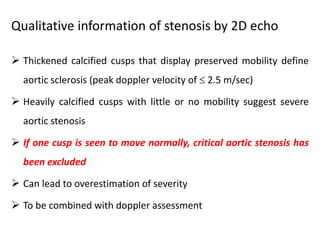
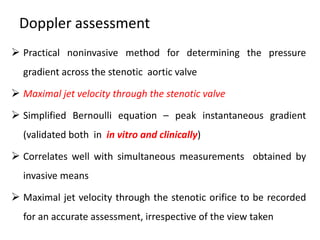
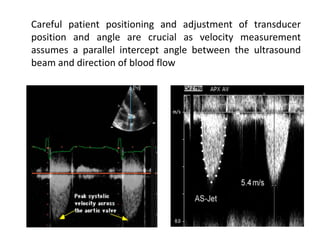
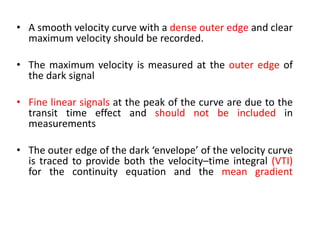
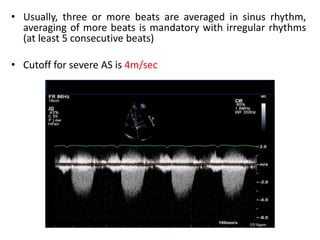
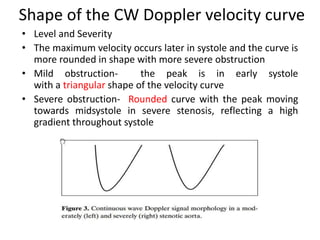
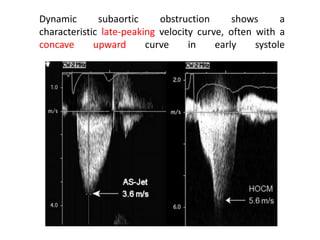
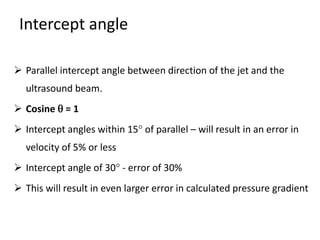
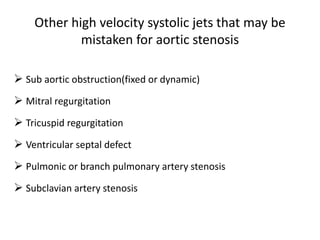
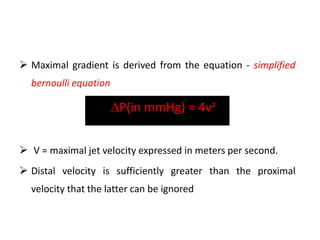
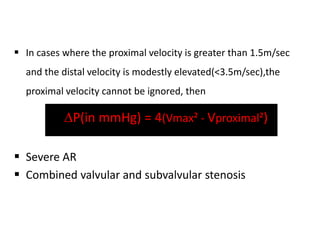
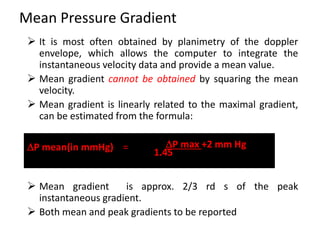
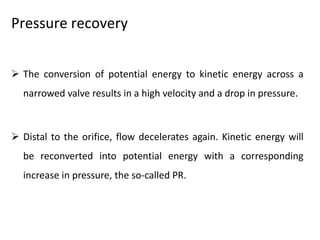
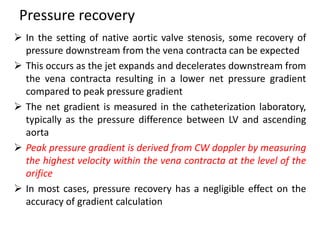
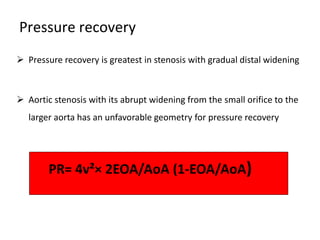
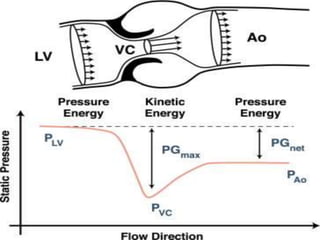
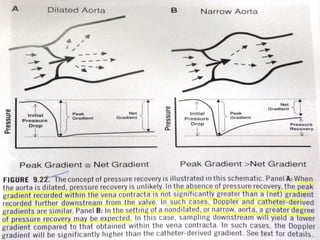
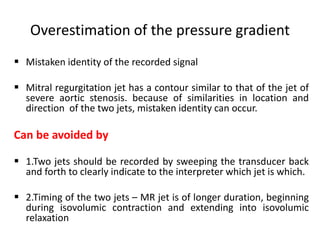
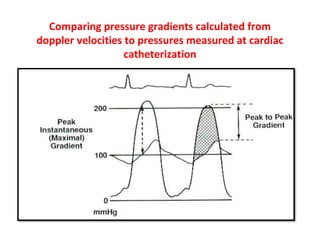
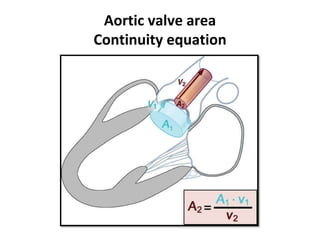
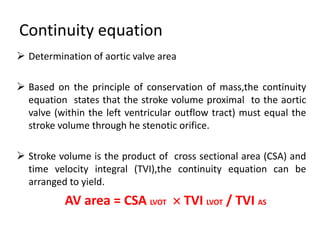
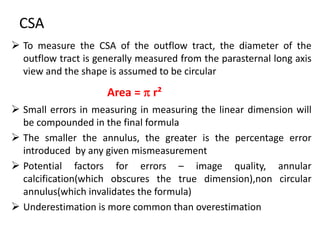
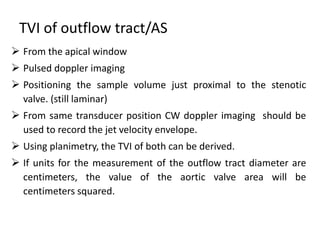
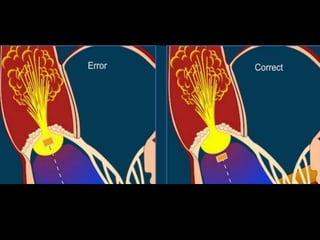
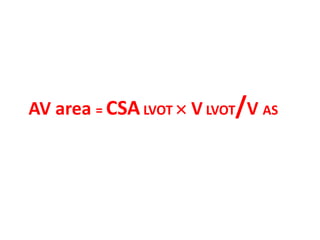
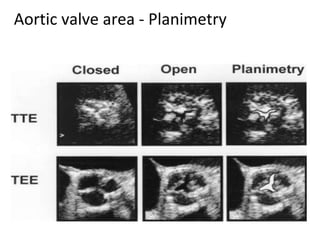
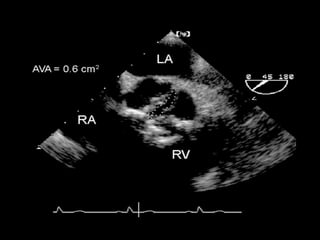
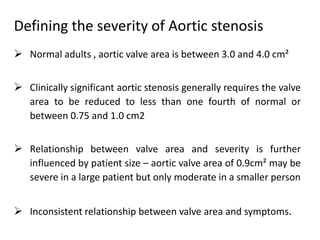
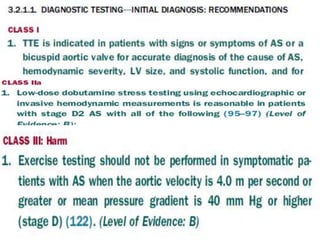
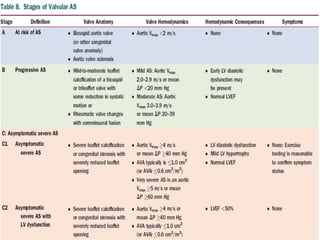
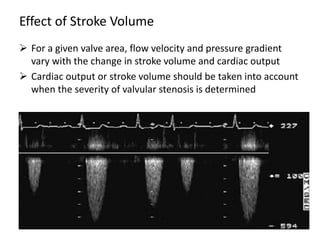
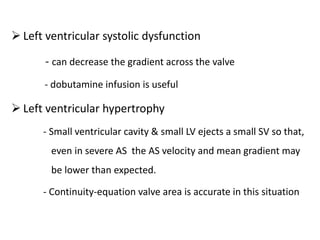
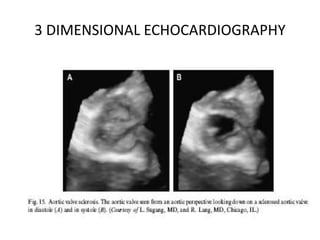
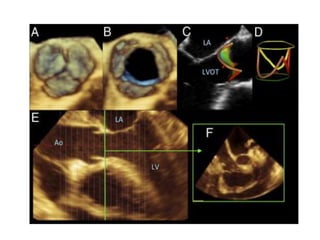
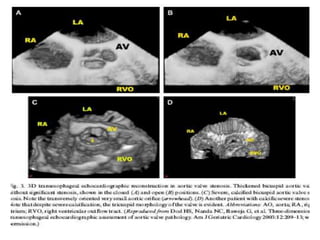
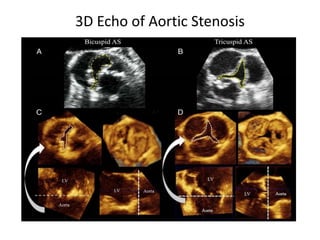
The document provides details on the anatomy and evaluation of aortic stenosis using echocardiography. It describes the normal aortic valve anatomy and how various types of aortic stenosis like calcific, rheumatic, bicuspid and subvalvular present on echo. Quantitative assessment of aortic stenosis severity is done using Doppler ultrasound to measure the maximum jet velocity and calculate the pressure gradient across the stenotic valve.