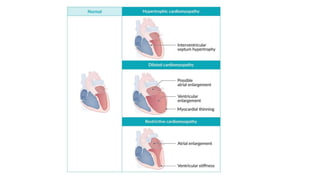
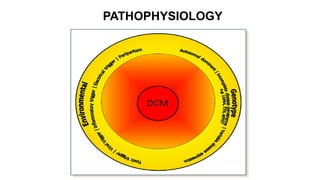
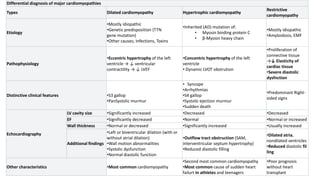
Cardiomyopathies are diseases of the heart muscle that weaken and enlarge the heart. There are three main types: dilated cardiomyopathy where the heart chambers enlarge, hypertrophic cardiomyopathy where the heart muscle thickens, and restrictive cardiomyopathy where the heart muscle stiffens. Dilated cardiomyopathy is the most common type and causes the heart to dilate and weaken over time from various genetic, toxic, or inflammatory causes ultimately leading to heart failure.