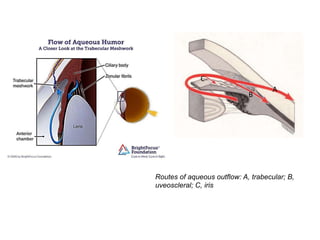
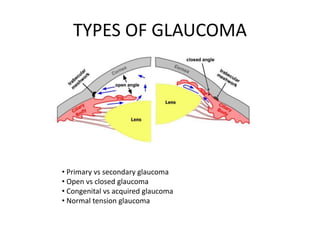
Glaucoma is a group of eye conditions that damage the optic nerve, often caused by an increase in intraocular pressure. The aqueous humour maintains pressure in the eye and normally flows through the anterior chamber, draining out of the eye. In glaucoma, the drainage pathways become blocked, increasing pressure and damaging the optic nerve. There are several types of glaucoma including open-angle glaucoma, the most common type caused by slow drainage blockage, and closed-angle glaucoma caused by physical blockage of drainage canals. Treatment aims to lower pressure through eye drops or surgery and slow progression of vision loss.