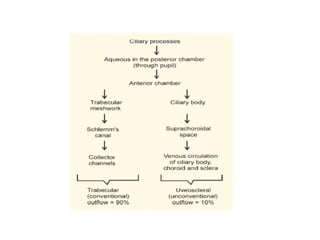
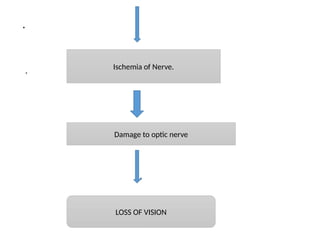
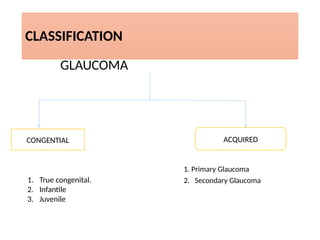
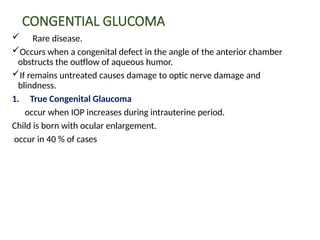
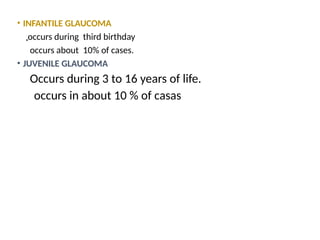
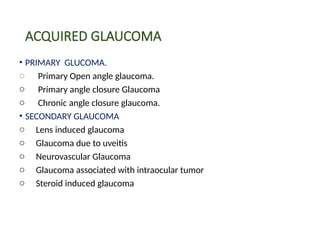
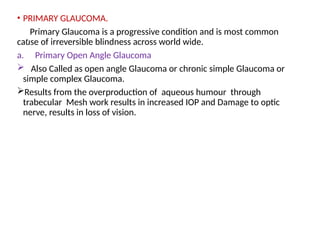
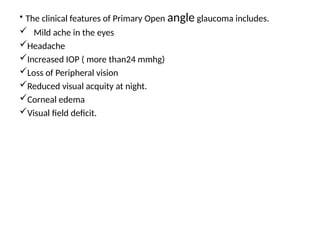
Glaucoma is a group of ocular conditions characterized by optic nerve damage due to increased intraocular pressure, which if untreated can lead to permanent loss of eyesight. It mainly affects individuals over 40 and can be classified into primary and secondary types, with various risk factors including genetics and eye trauma. Management includes medical and surgical interventions aimed at reducing intraocular pressure and preventing optic nerve damage.