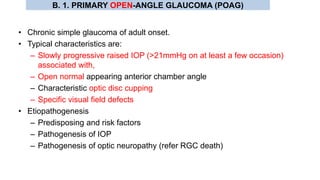
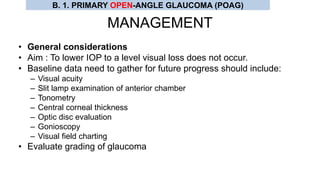
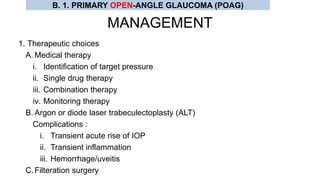
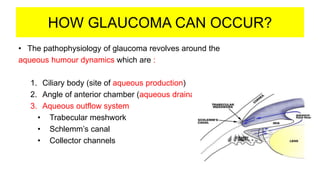
Glaucoma is a group of eye disorders characterized by optic nerve damage and visual field loss. Primary open-angle glaucoma (POAG) is the most common type of glaucoma. It is caused by a gradual increase in eye pressure due to impaired outflow of fluid from the eye. Risk factors include older age, family history, race, and high eye pressure. Patients may be asymptomatic initially, but can experience vision loss over time without treatment to lower eye pressure and prevent further optic nerve damage. Diagnosis involves examining the optic disc for cupping, visual field testing, and measuring intraocular pressure. Early treatment can help prevent vision loss from POAG.

![1. PRIMARY CONGENITAL / DEVELOPMENTAL GLAUCOMA
• Depending upon the age of onset the developmental glaucoma are termed as:
1. Newborn glaucoma (true congenital glaucoma)[40% of cases]
• When IOP raised during intrauterine life and child is born with ocular enlargement.
2. Infantile glaucoma [55% of cases]
• When the disease manifests prior to the child’s third birthday
3. Juvenile glaucoma (Juvenile open-angle glaucoma/POAG)[5%]
• Develop pressure rise after 3 years but before adulthood.
Bupthalmos (bull-like eyes) = The eyeball enlarges prior to age of 3 years
due to retention of aqueous humour; thus ‘hydropthalmos’ suggested
A. CONGENITAL AND DEVELOPMENTAL GLAUCOMA](https://image.slidesharecdn.com/glaucoma036-191110151413/85/Glaucoma-20-320.jpg)
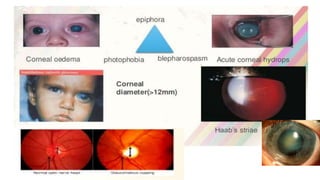
![CLINICAL FEATURES
1. Lacrimation, photophobia and blepharospasm
– Classic triad of congenital glaucoma
2. Corneal signs
I. Corneal edema
II. Corneal enlargement [>13mm confirms enlargement]
III. Tears and breaks in Descemet’s membranes (Haab’s striae) [appears as lines with
double contour]
3. Sclera : Thin and appears blue due to underlying uveal tissue.
4. Anterior chamber : Becomes deep
5. Iris : Iridodonesis and atrophic patches in late stage.
6. Lens : Flat due to stretching of zonules and subluxate backward.
7. Optic disc : Variable cupping and atrophy especially after third year.
8. IOP : Raised which is neither marked nor acute.
9. Axial myopia : Increase in axial length leading to anisometropic amblyopia.
A. CONGENITAL AND DEVELOPMENTAL GLAUCOMA](https://image.slidesharecdn.com/glaucoma036-191110151413/85/Glaucoma-22-320.jpg)
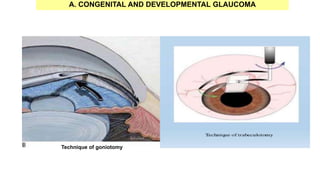
![TREATMENT
• Medical treatment (acetazolamide, beta blocker)
• Surgical procedures
1. Incisional angle surgery
• Internal approach (goniotomy)[85% success rate]
– Barkan’s goniotomy knife (approximately 75o)
• External approach (trabeculectomy)
– Harm’s trabeculotome
2. Filteration surgery
• Trabeculectomy with antimetabolites gives good results.
• Combined trabeculectomy and trabeculectomy with antimetabolites
3. Glaucoma drainage devices (GDD)
• Required in incalcitrant cases.
A. CONGENITAL AND DEVELOPMENTAL GLAUCOMA](https://image.slidesharecdn.com/glaucoma036-191110151413/85/Glaucoma-26-320.jpg)