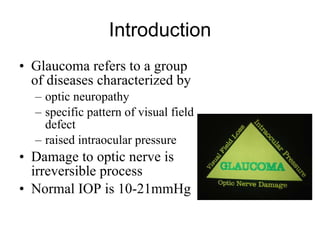
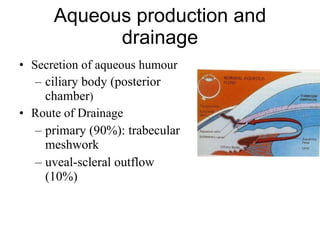
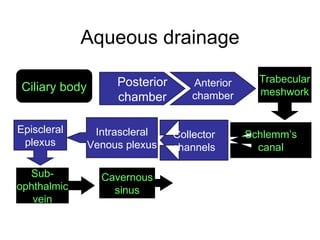
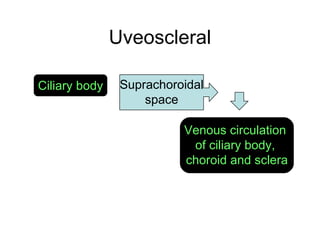
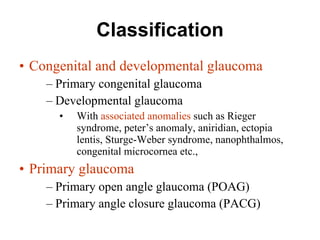
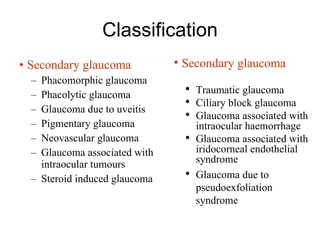
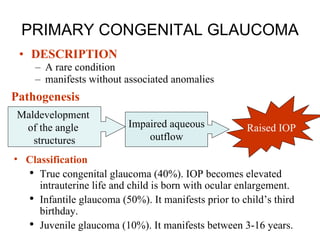
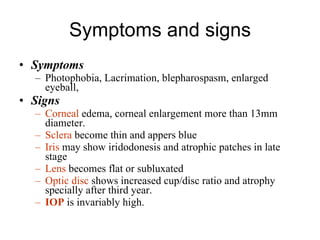
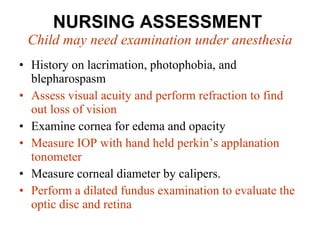
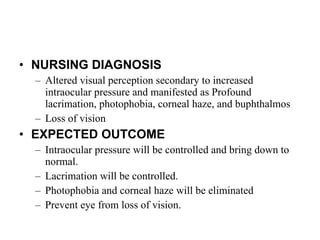
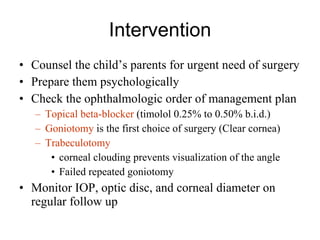
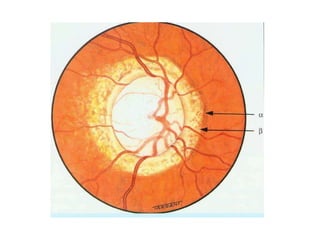
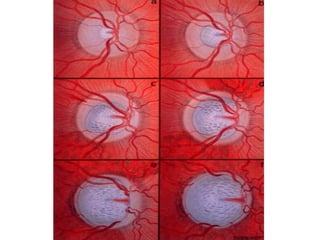
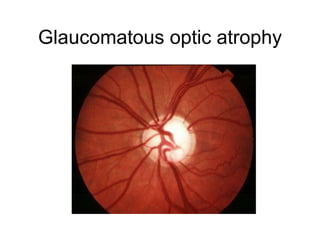
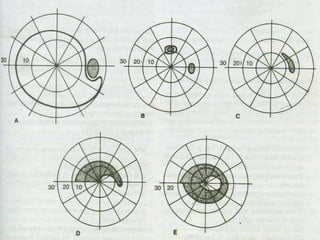
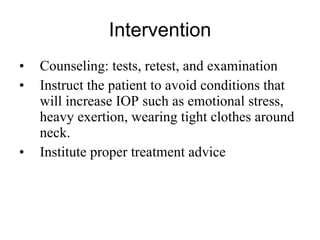
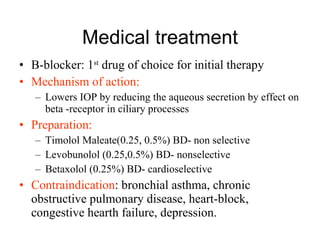
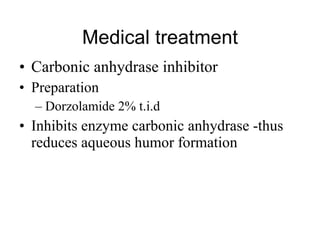
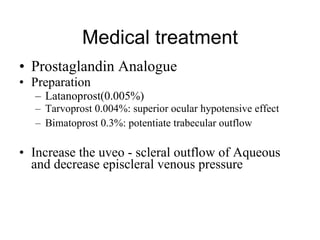
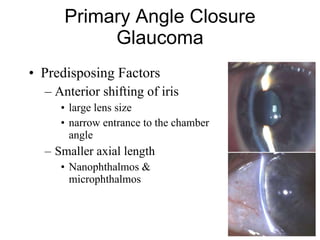
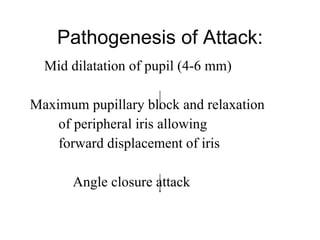
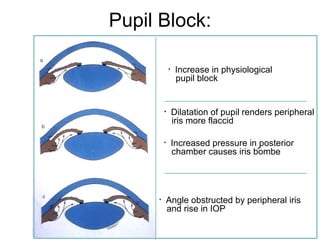
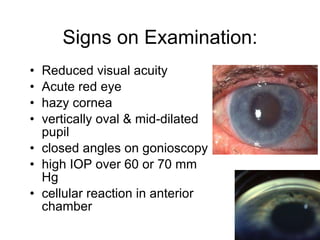
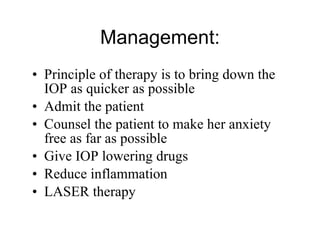
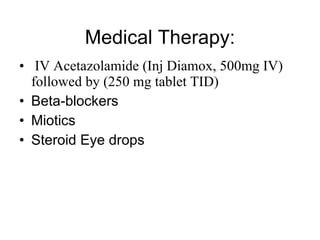
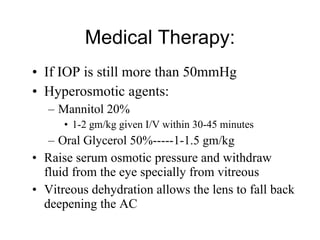
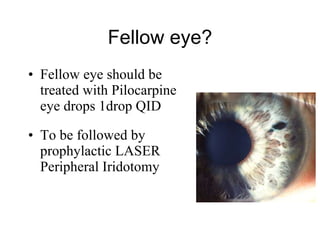
The document discusses glaucoma, its types, classifications, and management strategies. It covers congenital and primary glaucoma, secondary glaucoma, and primary angle closure glaucoma, detailing symptoms, diagnostic approaches, and treatment options including medications and surgical interventions. The document emphasizes the importance of controlling intraocular pressure to prevent vision loss and outlines nursing assessments and patient care related to glaucoma.