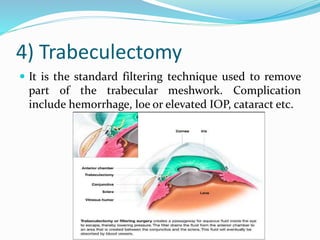
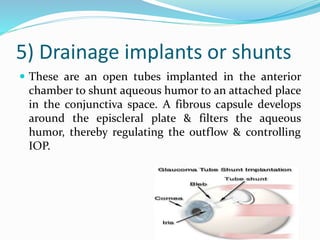
This document discusses glaucoma, defining it as an eye disease characterized by loss of retinal ganglion cells and their axons caused by increased intraocular pressure. It is the leading cause of irreversible blindness. There are two main types - open angle glaucoma, the most common type, and angle closure glaucoma. Diagnosis involves measuring intraocular pressure and examining the optic nerve and visual field. Treatment options include eye drop medications, laser treatments, and surgeries like trabeculectomy to improve fluid drainage from the eye. Nursing care focuses on managing pain, allaying fears, and educating patients.