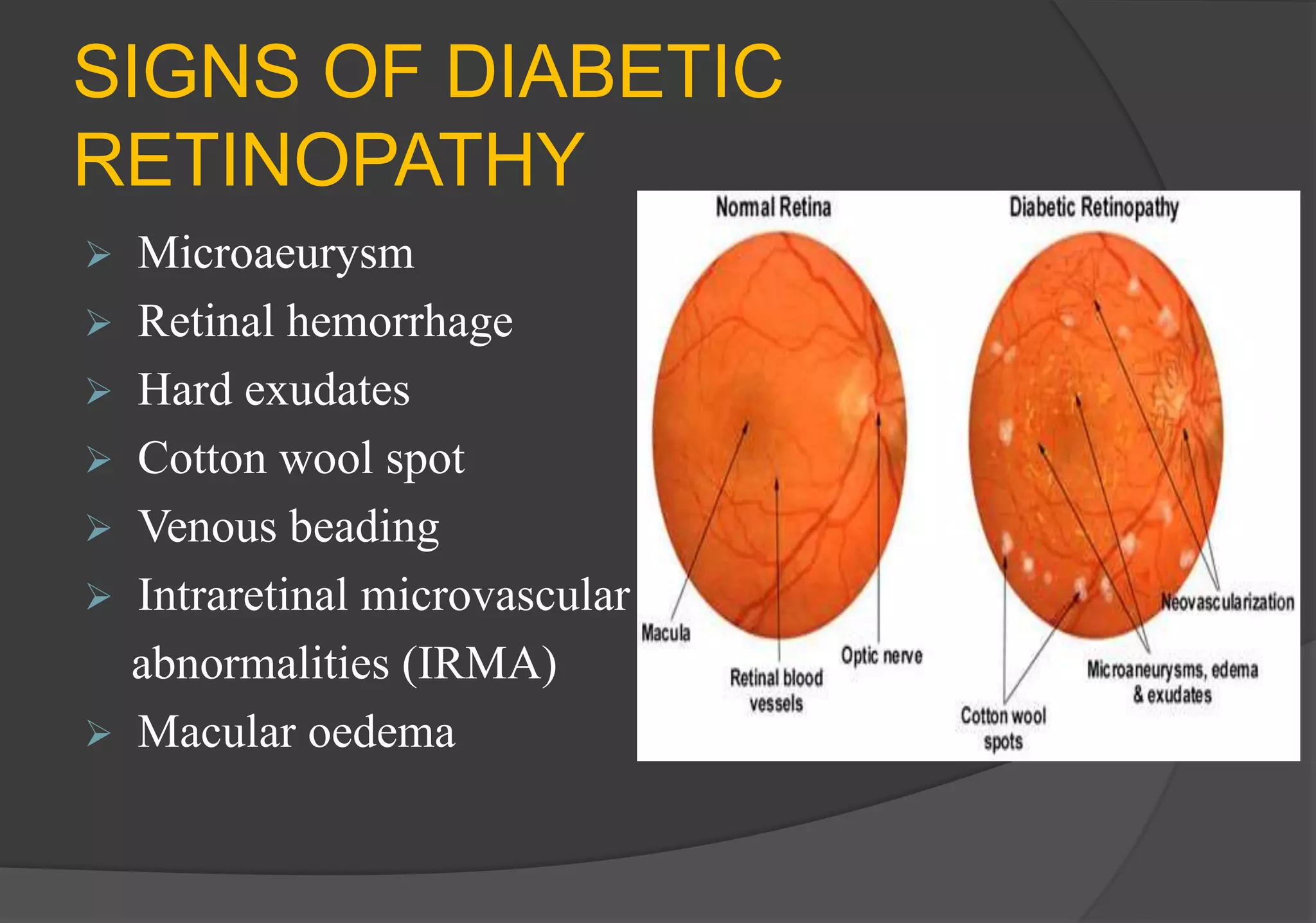
Diabetic retinopathy is a complication of diabetes that affects the eyes. It is caused by changes in the blood vessels of the light-sensitive tissue (retina). Prolonged high blood sugar can damage the tiny blood vessels inside the retina. This document discusses the risk factors, signs and symptoms, classifications, screening, diagnosis, and management of diabetic retinopathy. Laser therapy, anti-VEGF injections, and vitrectomy are common treatments used to prevent vision loss from this condition. Strict control of blood sugar, blood pressure, and lipids is important to reduce the risk and progression of diabetic retinopathy.