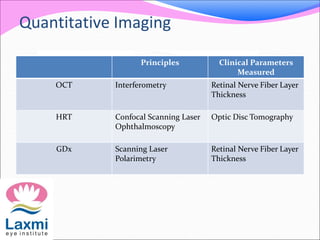
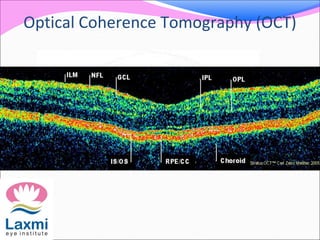
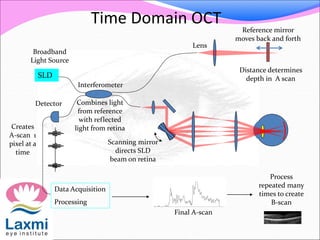
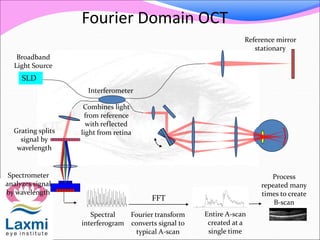
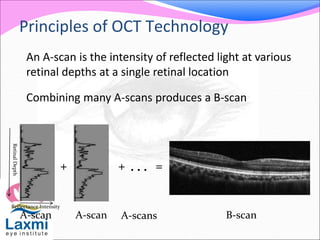
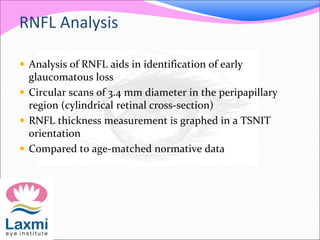
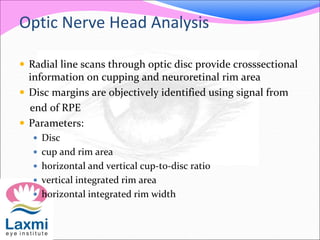
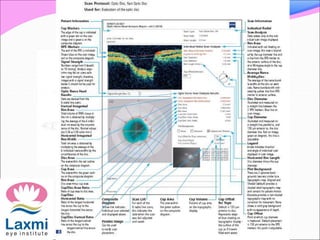
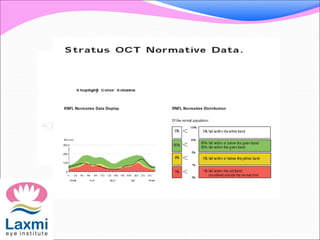
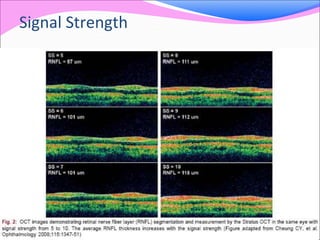
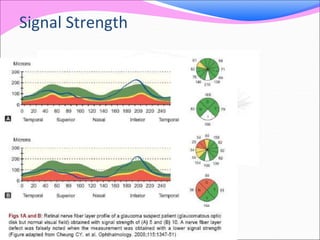
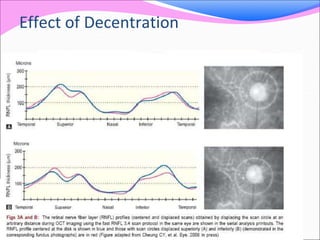
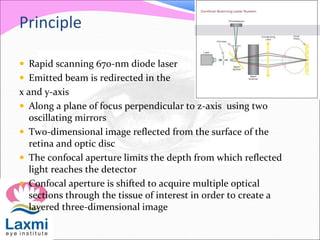
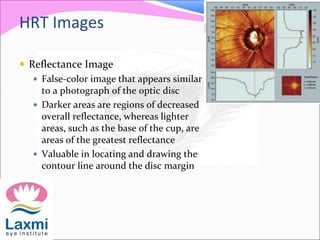
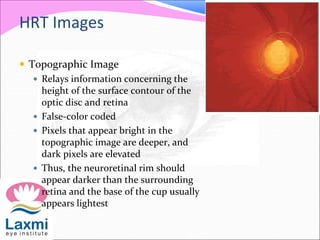
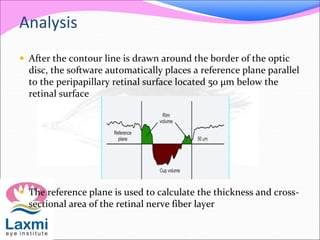
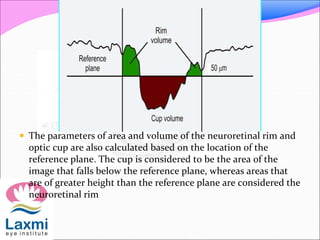
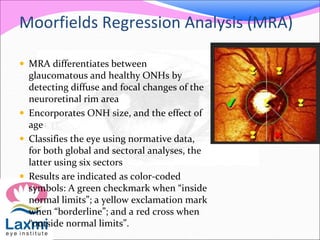
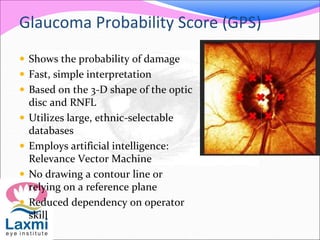
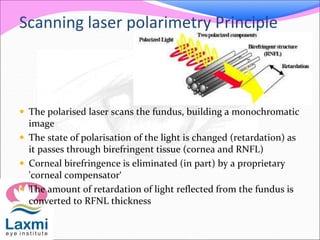
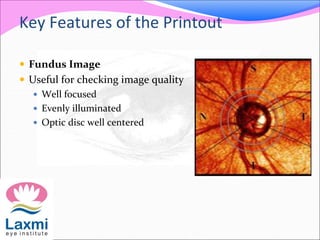
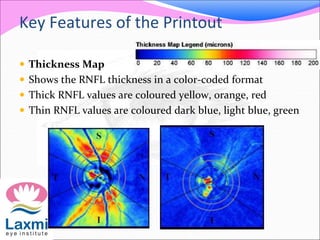
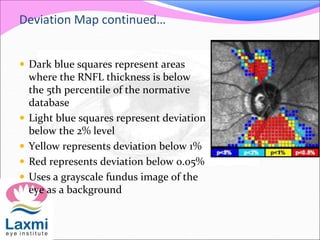
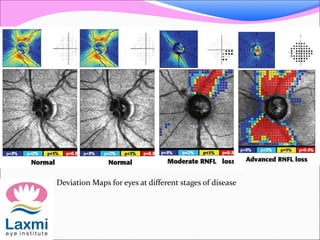
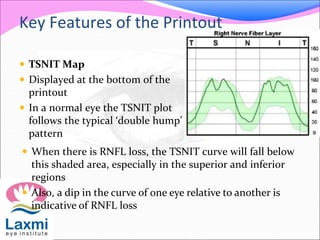
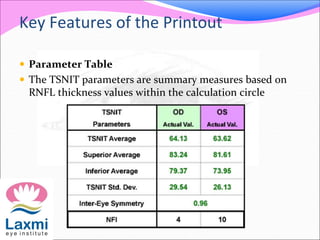
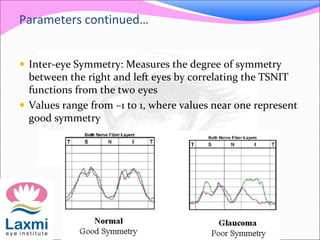
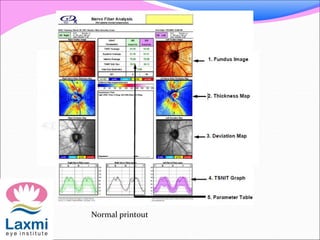
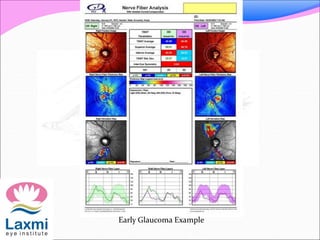
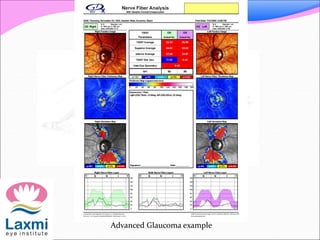
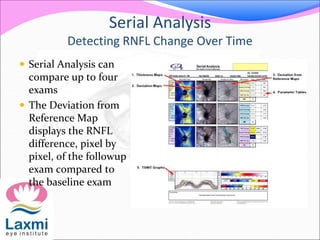
This document discusses various imaging techniques used to evaluate glaucoma, including OCT, HRT, and GDx. OCT uses interferometry to measure retinal nerve fiber layer thickness. HRT uses confocal laser scanning to create 3D images of the optic nerve and measure disc parameters. GDx uses scanning laser polarimetry to measure retinal nerve fiber layer thickness and detect glaucomatous damage through thickness maps, deviation maps, and TSNIT plots compared to normative data. Together these quantitative imaging techniques provide objective assessment to aid in glaucoma diagnosis and detection of progression.