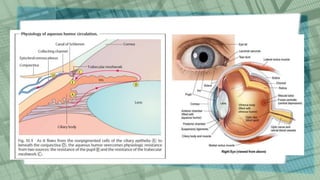
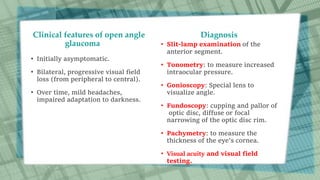
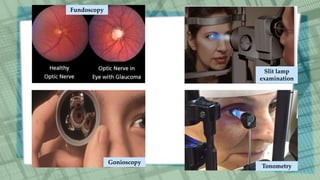
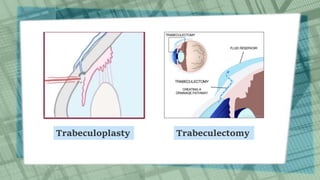
Glaucoma is a group of eye diseases that causes optic nerve damage and vision loss due to increased pressure in the eye (intraocular pressure). The two main types are open-angle glaucoma, which accounts for 90% of cases, and angle-closure glaucoma. Treatment options aim to lower intraocular pressure and prevent further vision loss through eye drop medications, laser treatments, or surgery. Glaucoma can also be caused secondary to other conditions like diabetes or inflammation and may be present from birth in rare cases of congenital glaucoma.