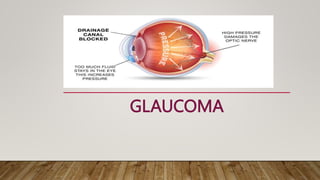
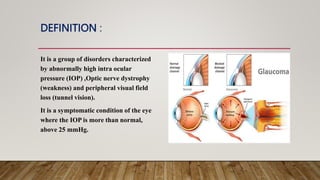
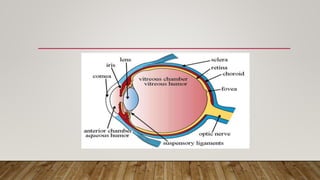
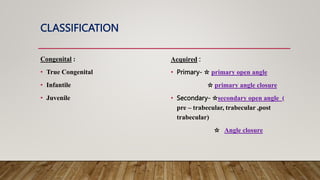
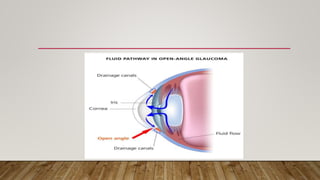
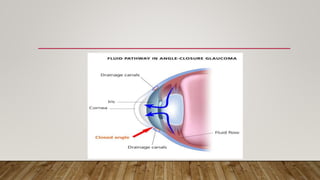
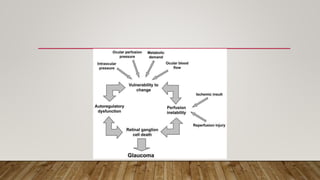
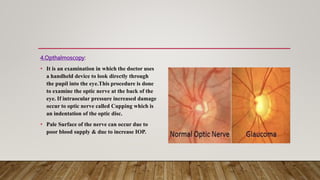
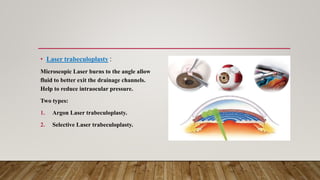
This document provides an overview of glaucoma, including its definition, causes, risk factors, symptoms, diagnostic tests, treatment options, and post-operative complications. Glaucoma is an eye disease where damage to the optic nerve leads to vision loss. It is often caused by abnormally high pressure within the eye. Diagnostic tests include visual field testing, tonometry, ophthalmoscopy and gonioscopy. Treatment may involve eye drops, oral medication, laser procedures or surgery to improve fluid drainage from the eye. Surgical options include trabeculectomy, laser treatments, and the use of aqueous shunt devices. Post-operative risks include infection, shallow anterior chamber and over or under filtration of fluid from the eye