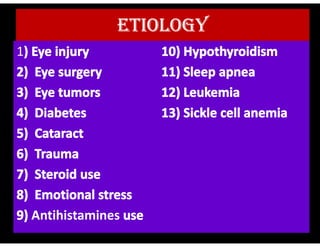
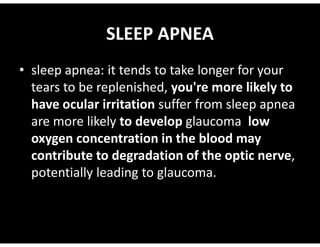
1. Glaucoma is a group of eye conditions characterized by optic nerve damage and vision loss due to increased pressure in the eye. The increased pressure damages the optic nerve, leading to blindness if not treated.
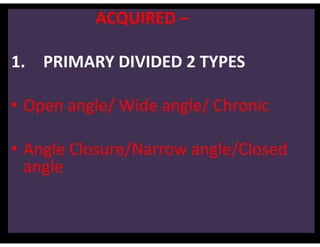
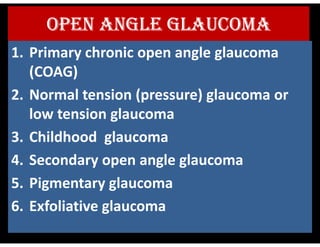
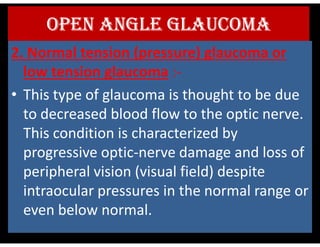
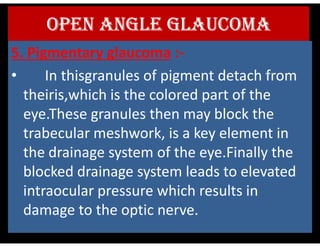
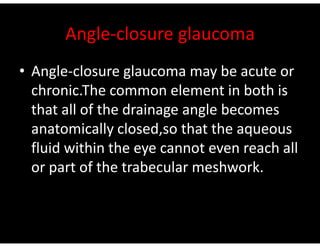
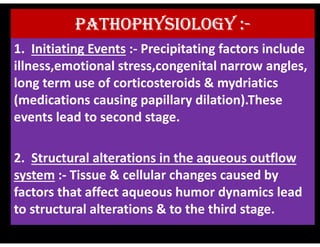
2. There are several types of glaucoma including open-angle glaucoma, which is the most common type, as well as angle-closure, normal tension, and congenital glaucoma.
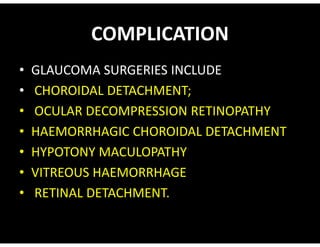
3. Glaucoma is diagnosed through tests such as tonometry, ophthalmoscopy, visual field tests, and imaging of the optic nerve. Treatment options include eye drop medications to lower pressure, laser treatments, and surgeries like trabeculectomy to drain fluid from the eye