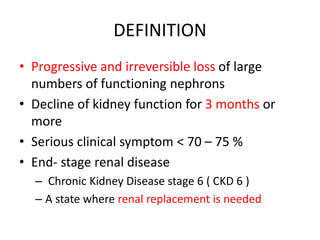
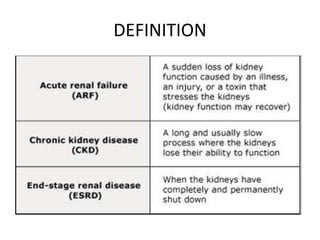
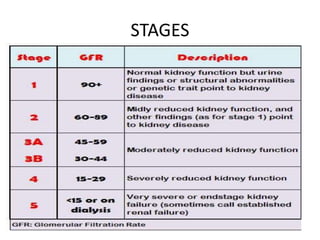
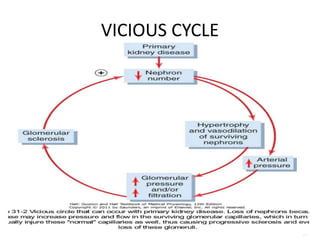
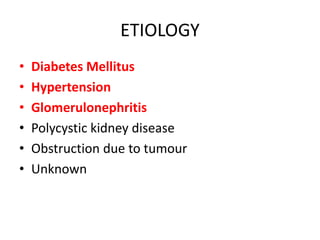
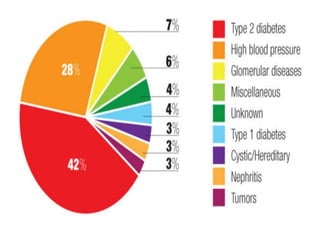
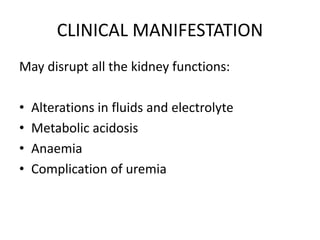
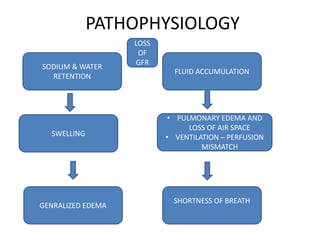
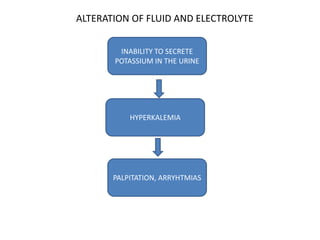
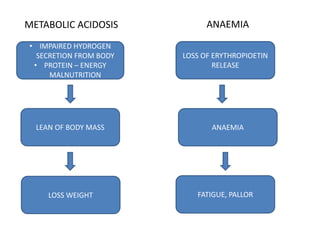
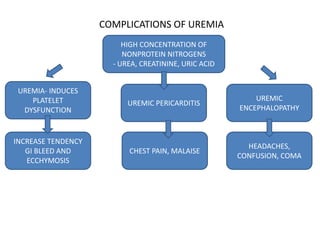
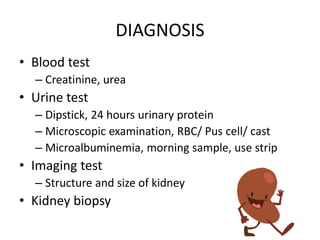
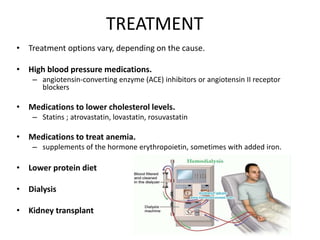
Chronic renal failure is the progressive loss of kidney function over months or years. It is defined as a decline in glomerular filtration rate below 70-75% and is generally irreversible. It progresses through stages and is caused by conditions like diabetes, hypertension, and glomerulonephritis. Symptoms result from kidney's inability to regulate fluids, electrolytes, and waste and include edema, shortness of breath, fatigue, and neurological changes. Treatment focuses on slowing progression through blood pressure control, cholesterol medications, treating anemia, and dialysis or transplant for end-stage disease.