This document provides information about glaucoma, including:
- Glaucoma is characterized by loss of vision due to damage to the optic nerve, usually caused by elevated intraocular pressure. Vision loss from glaucoma is irreversible.
- While elevated IOP is a major risk factor, not all glaucoma involves high pressure, and many people with elevated pressure never develop glaucoma.
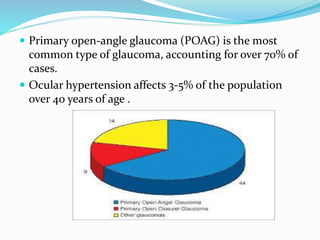
- There are several types of glaucoma including open-angle glaucoma (POAG), angle-closure glaucoma (PACG), and secondary glaucomas caused by underlying conditions.
- Treatment depends on the type but may involve medications, laser treatment, or surgery to lower