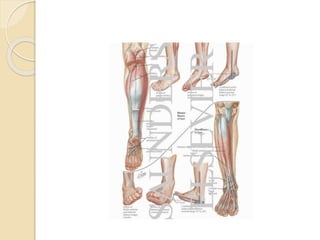
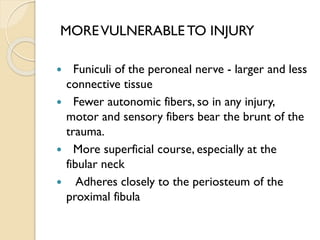
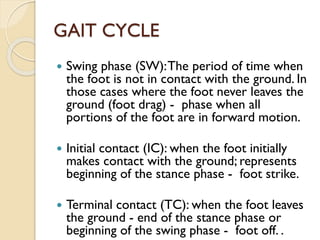
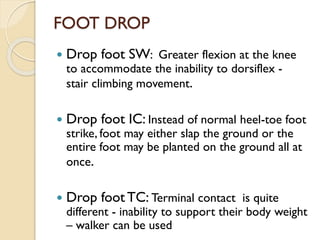
Foot drop is caused by weakness of the muscles that lift the front of the foot due to damage to the common peroneal nerve. This prevents dorsiflexion of the ankle and toes. It can be unilateral or bilateral, and temporary or permanent. Symptoms include difficulty lifting the foot and slapping it down when walking. Treatment depends on the underlying cause but may include braces, physical therapy, nerve stimulation, or tendon transfer surgery if conservative treatments fail.