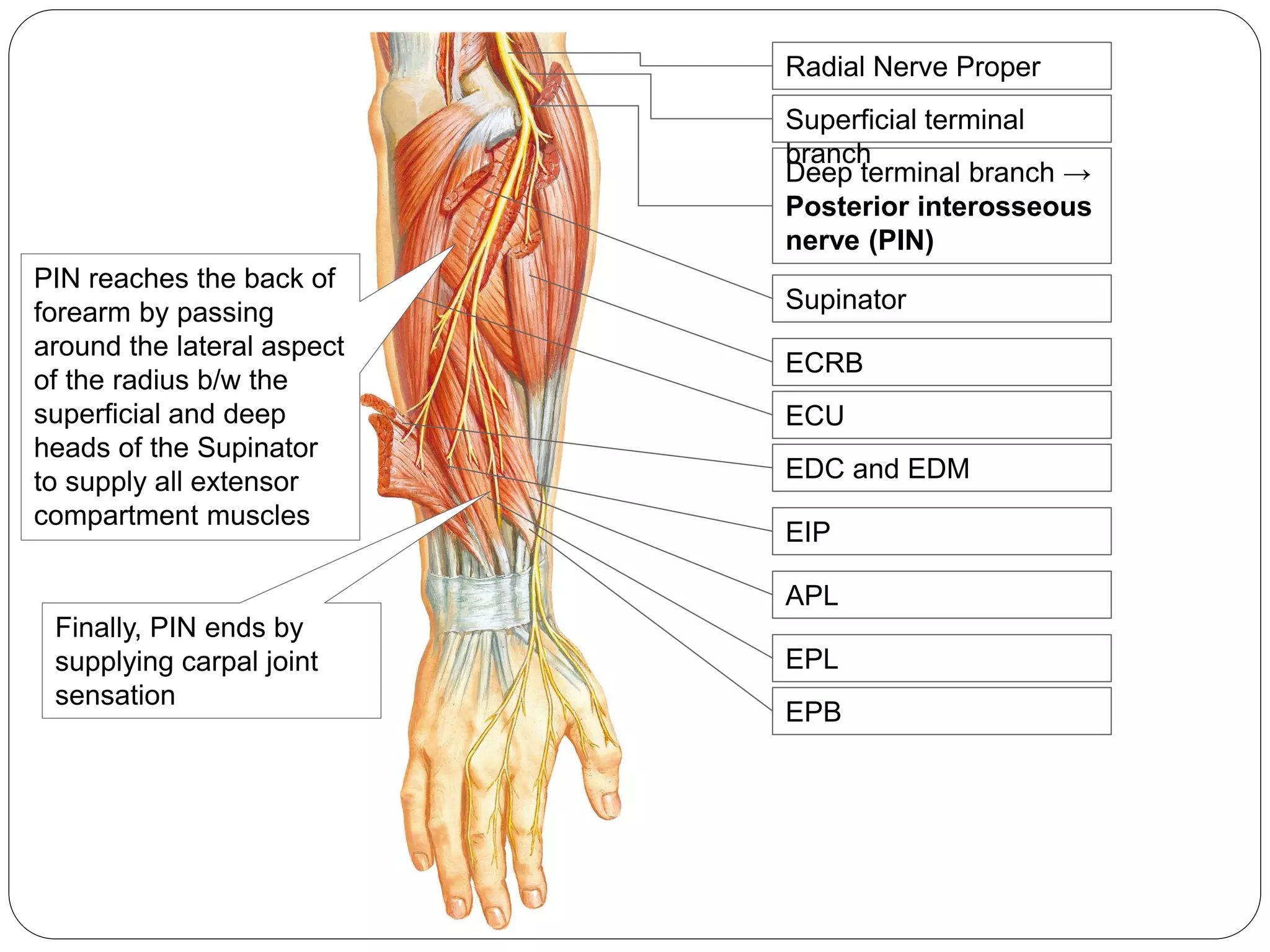
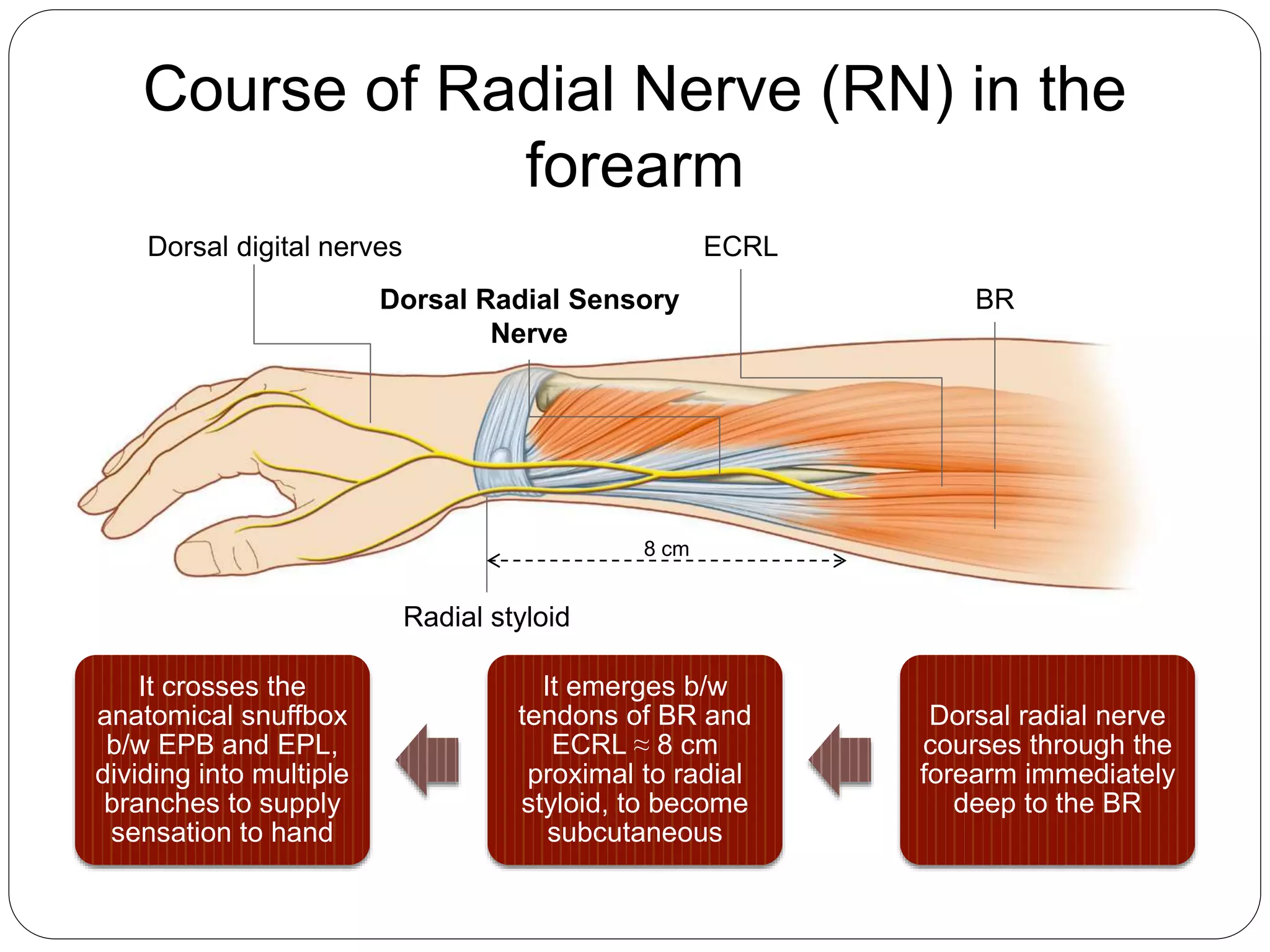
The document provides information about the radial nerve including its anatomy, course, branches and clinical presentations of radial nerve palsies. It discusses the radial nerve's origin from the brachial plexus and branches in the arm and forearm. Common causes of radial nerve palsy include fractures and entrapment in the radial tunnel. Clinical features, investigations, treatment including splinting and tendon transfers, and postoperative management are outlined. Surgical techniques for nerve repair and reconstructive procedures are also described.














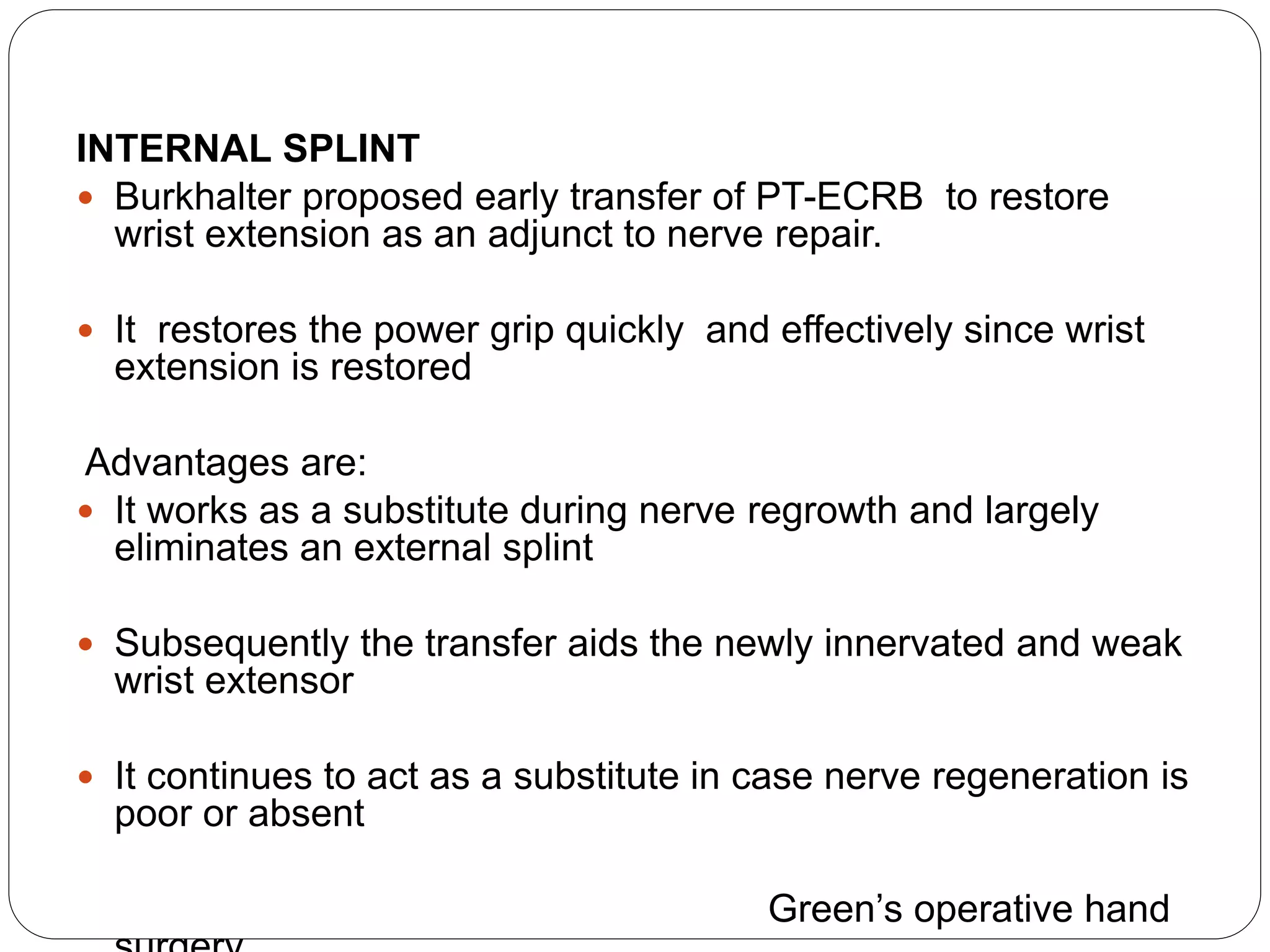








![ A patient with irreparable radial nerve palsy
needs to be provided with
(1) wrist extension.
(2) finger (metacarpophalangeal [MP] joint)
extension.
(3) a combination of thumb extension and
abduction.
Requirements in a Patient with Radial Nerve
Palsy](https://image.slidesharecdn.com/radialnervepalsy-160706134024/75/Radial-nerve-palsy-30-2048.jpg)