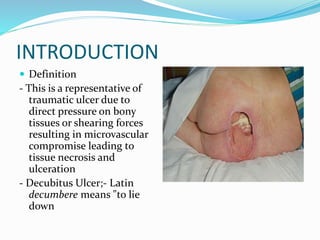
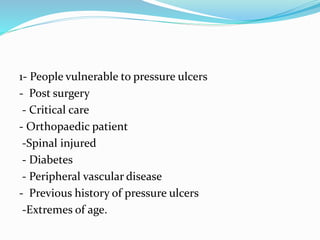
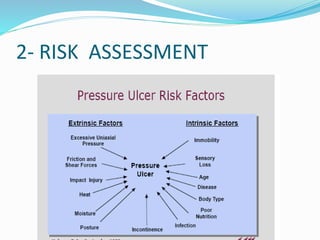
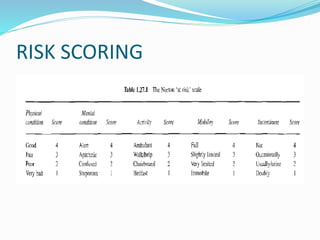
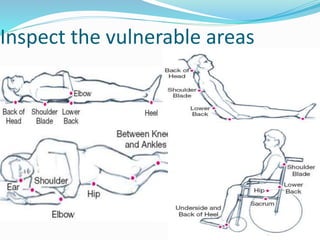
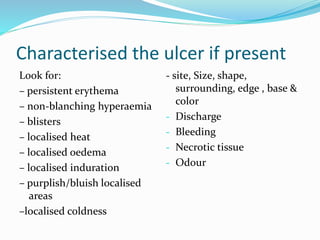
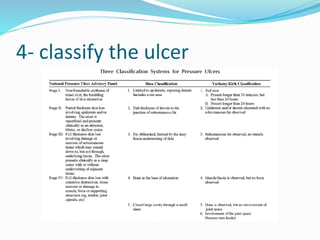
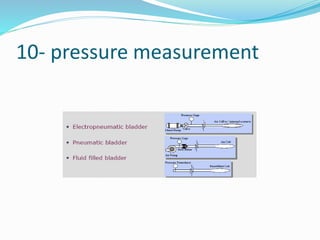
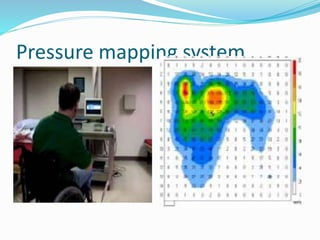
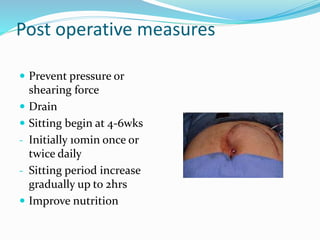
The document provides a comprehensive overview of pressure ulcers, including their definition, epidemiology, diagnosis, and management strategies. It emphasizes the importance of prevention, early mobilization, and multidisciplinary care in treating vulnerable patients and outlines both non-operative and operative treatment options. The conclusion stresses that effective pressure ulcer management is crucial due to its associated morbidity, mortality, and economic impact.