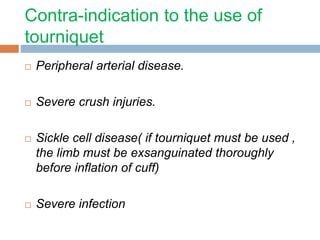
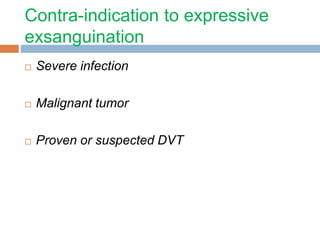
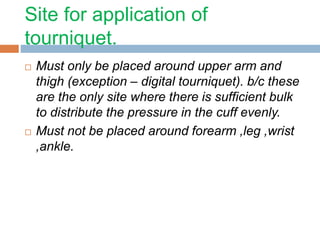
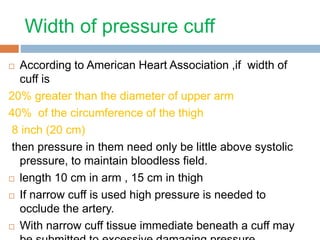
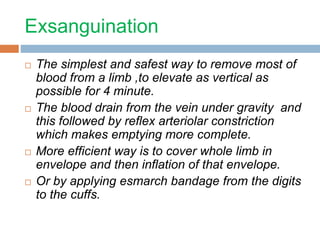
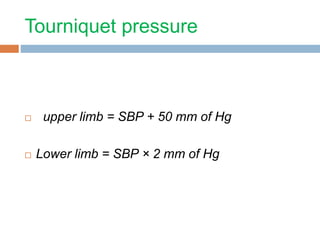
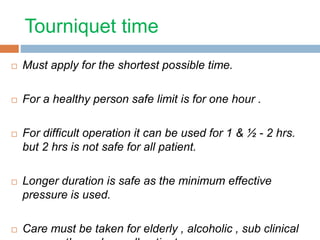
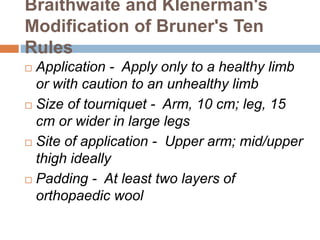
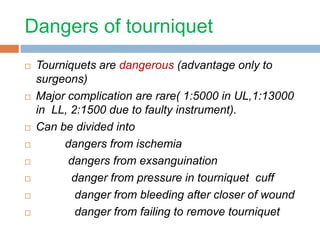
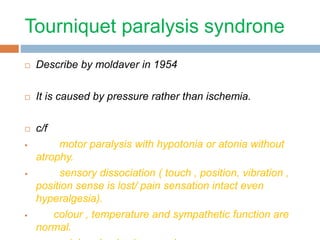
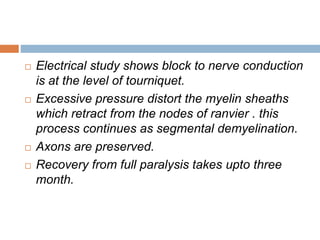
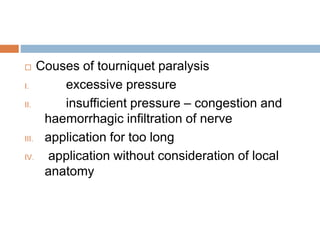
This document discusses the application of tourniquets in orthopaedics. It provides a history of tourniquet development and describes the types of tourniquets. Pneumatic tourniquets are now most commonly used and can be non-automated or automated. Guidelines are presented for the safe use of tourniquets, including appropriate application sites, padding, pressures, and time limits. Potential complications from ischemia, pressure in the cuff, and failure to remove the tourniquet are outlined. Proper exsanguination techniques using an Esmarch bandage are also described.