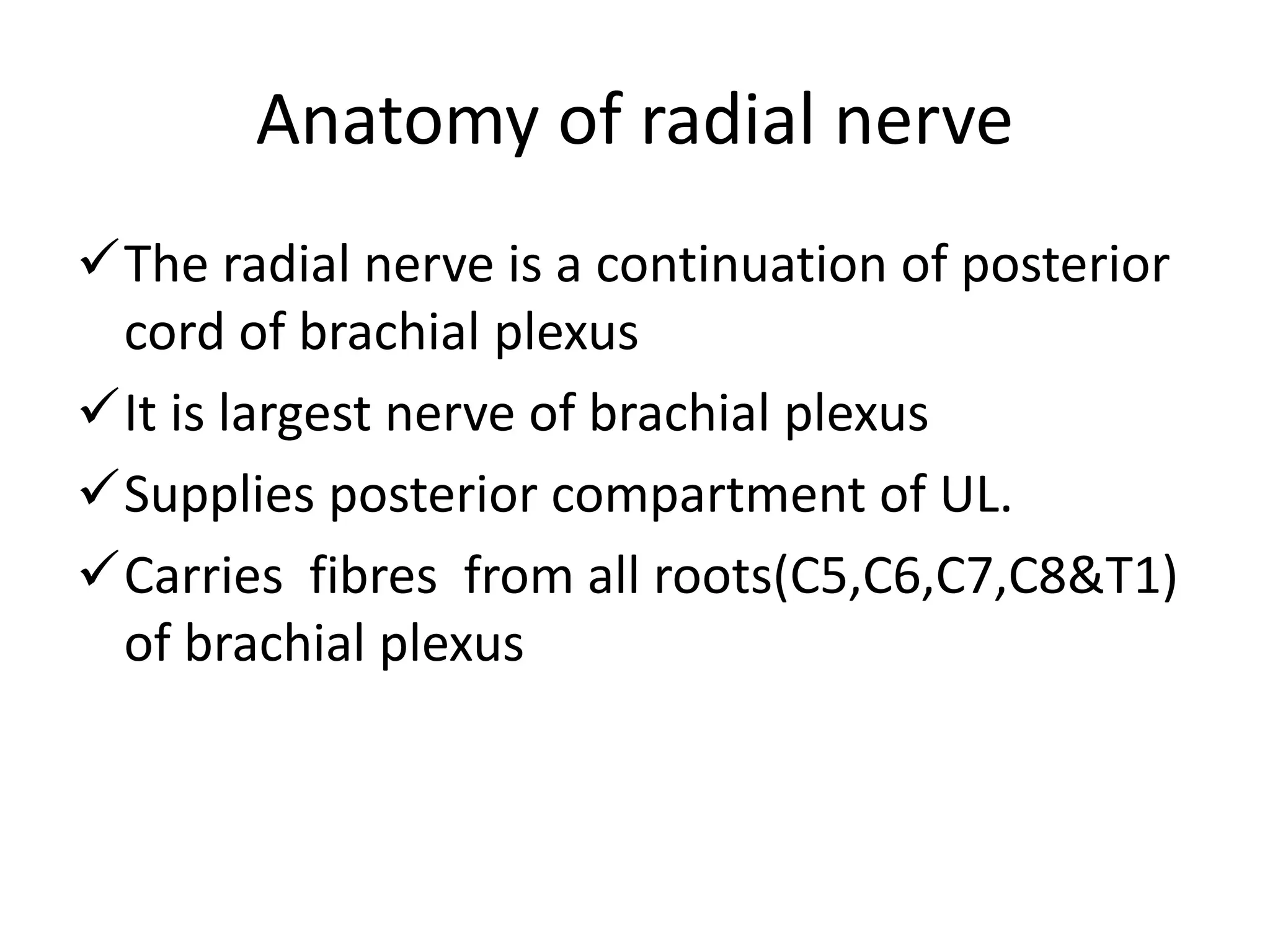
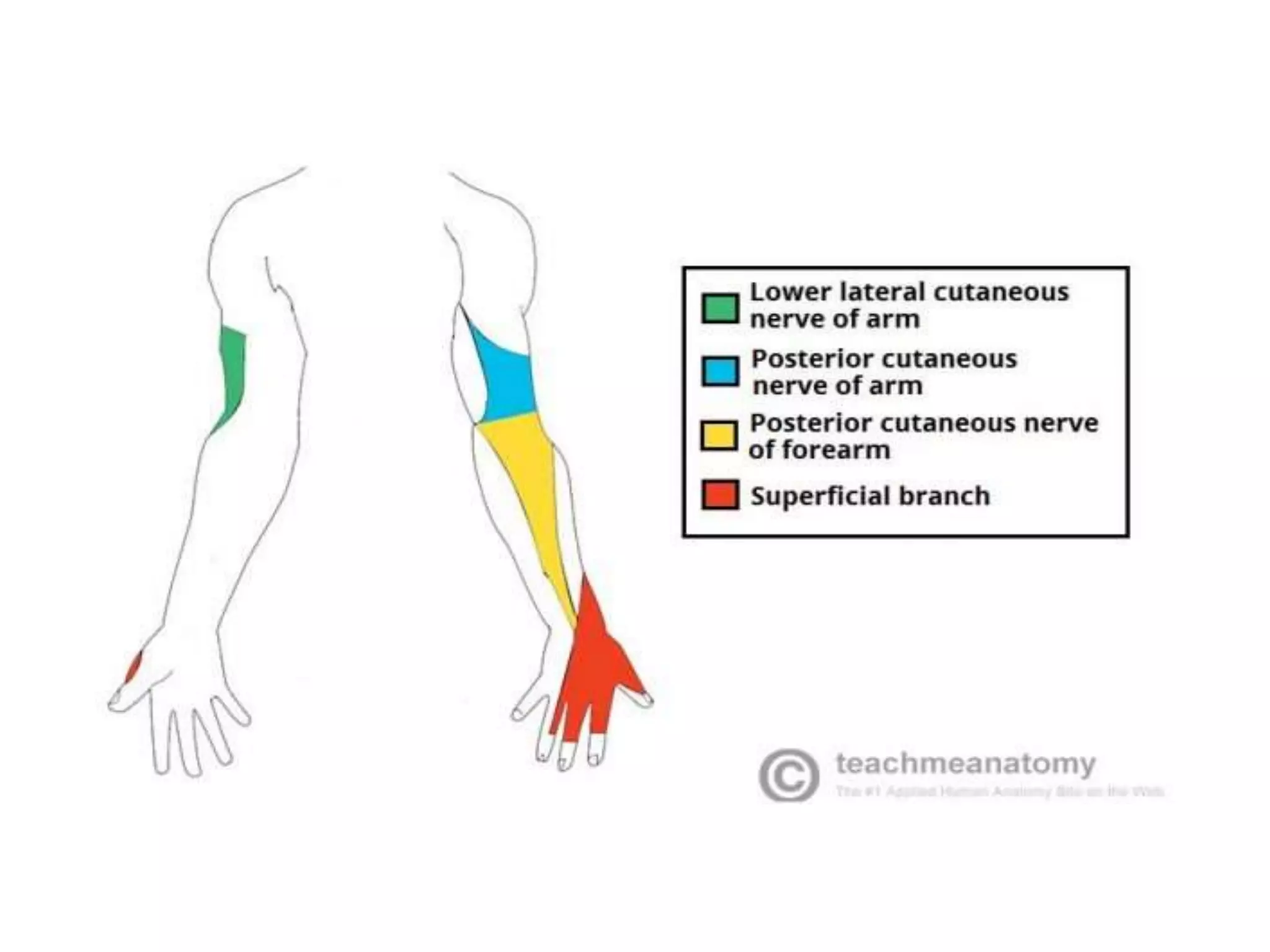
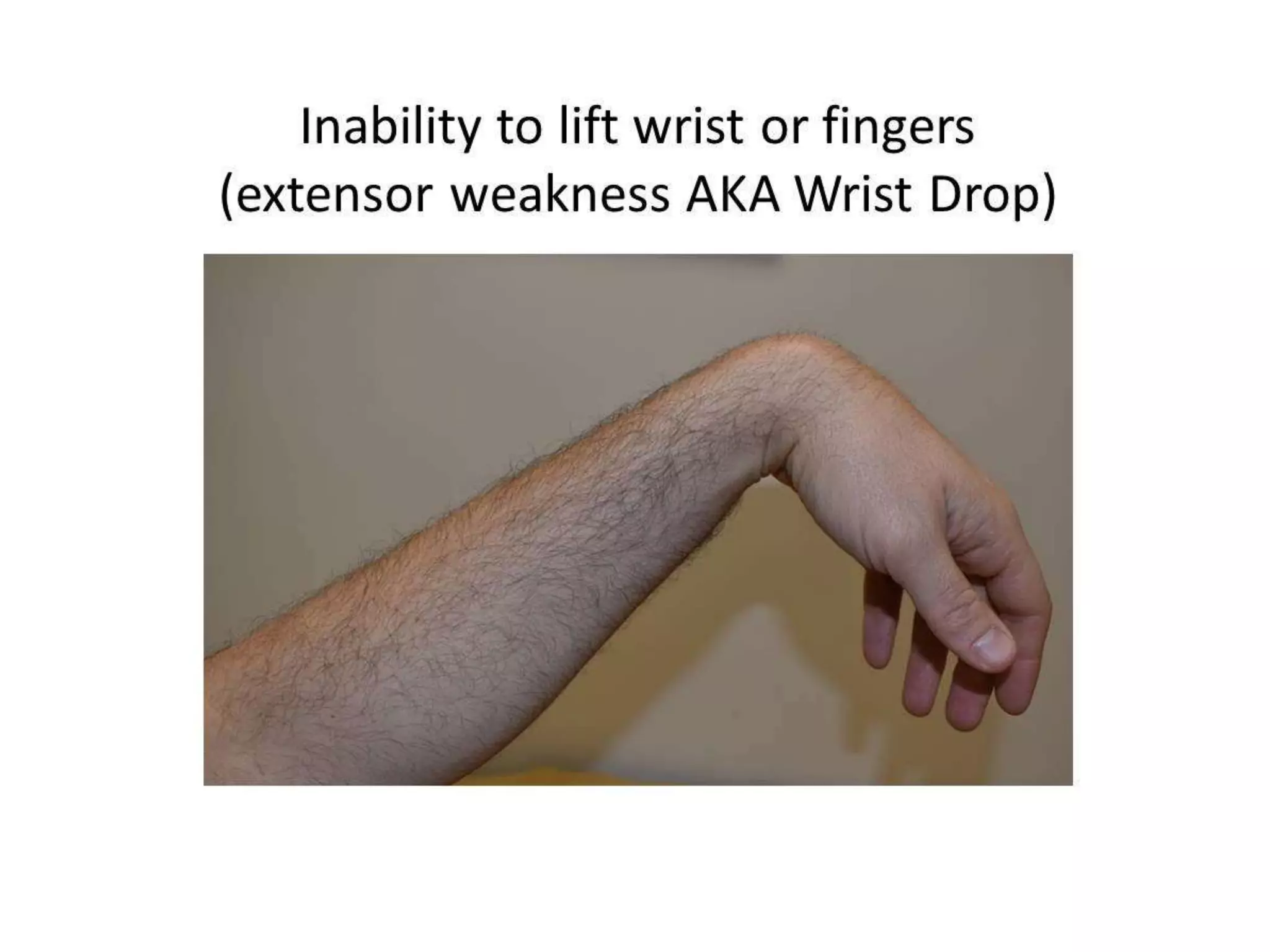
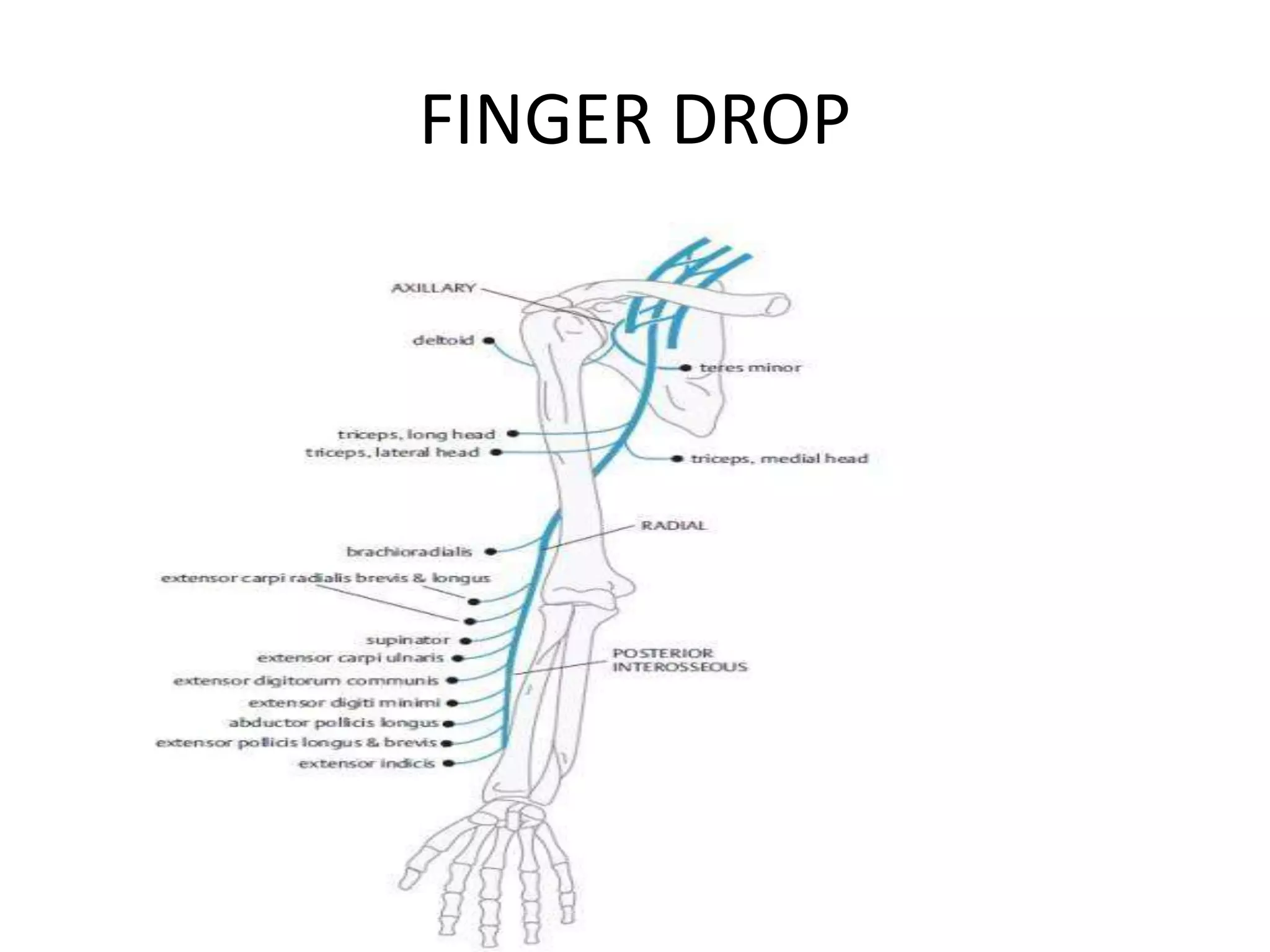
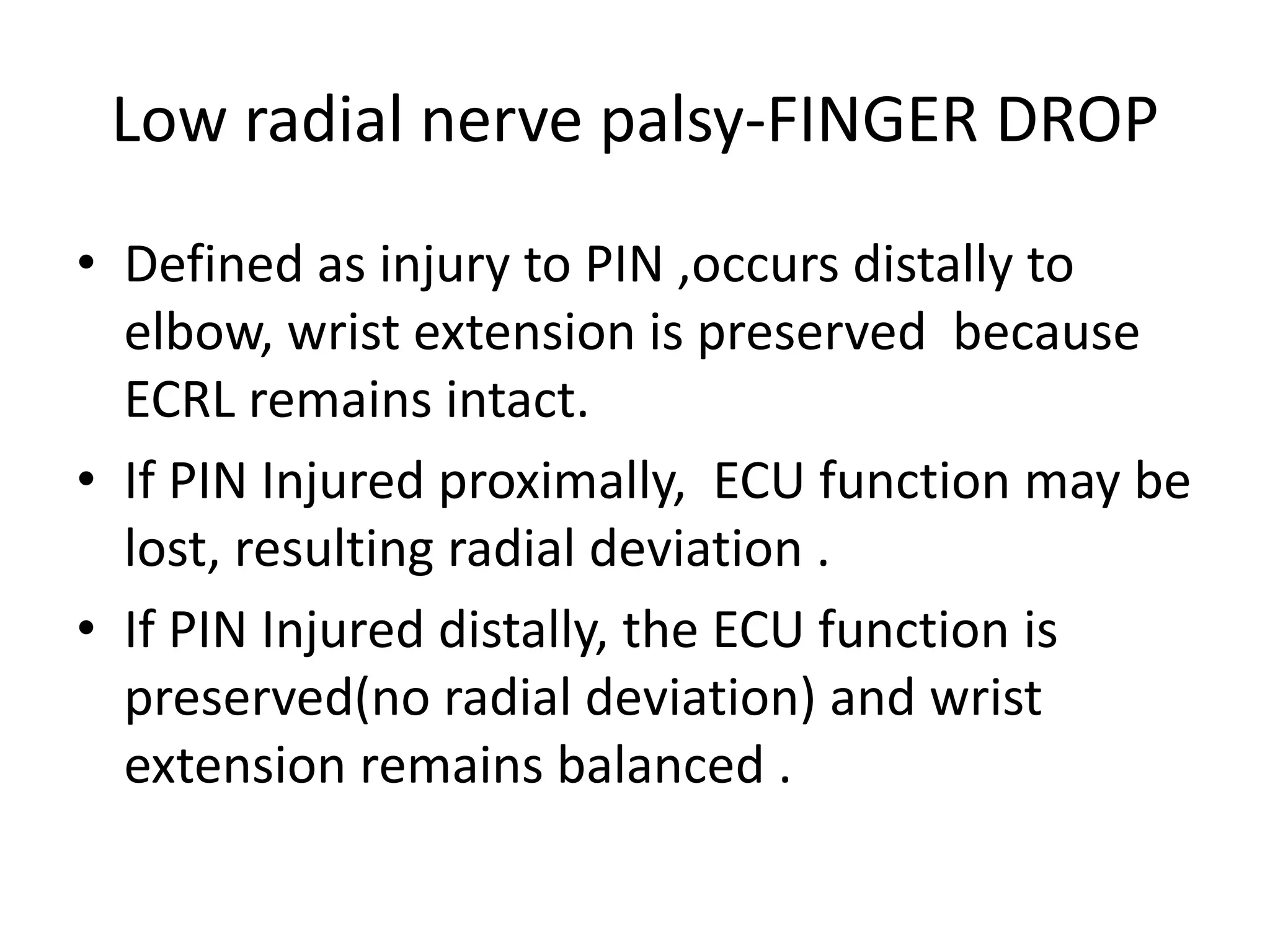
This document discusses wrist drop, finger drop, and foot drop caused by radial nerve palsy. It provides details on the anatomy of the radial nerve and explains how injuries at different points can cause wrist drop or finger drop. For foot drop, it describes the anatomy of the leg and discusses how peroneal nerve injuries or issues with the sciatic nerve or L5 root can cause weakness of the dorsiflexors. It outlines the clinical features, diagnostic process, and treatment options including conservative care, physical therapy, splinting, and in some cases surgery.