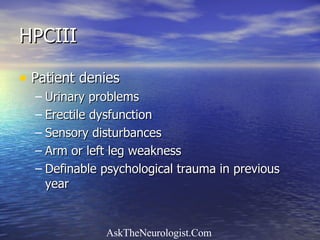
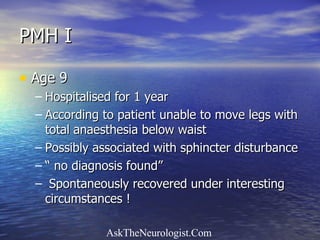
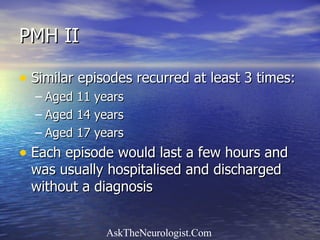
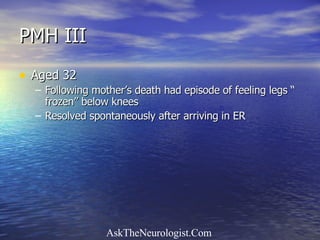
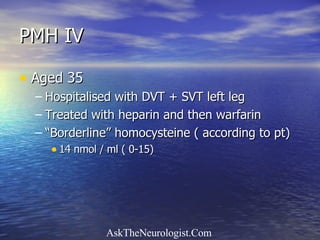
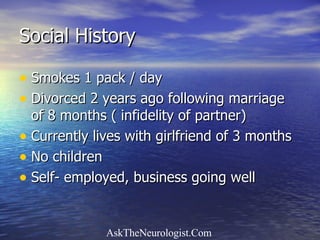
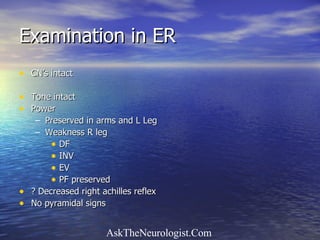
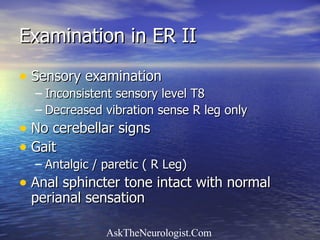
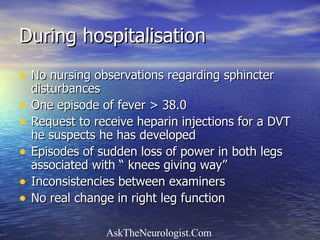
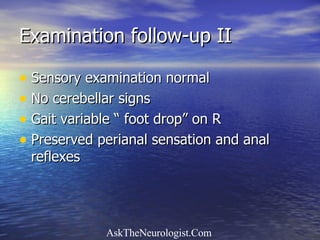
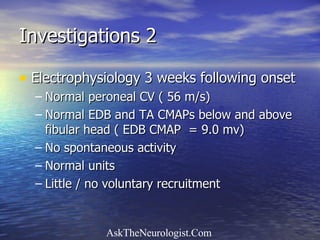
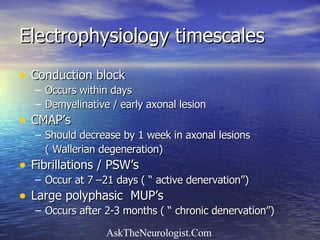
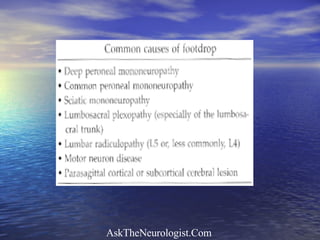
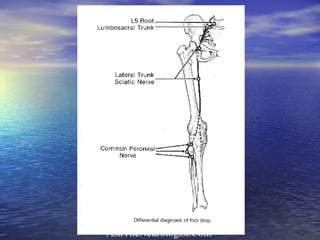
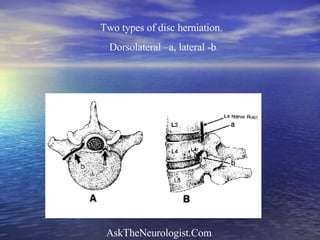
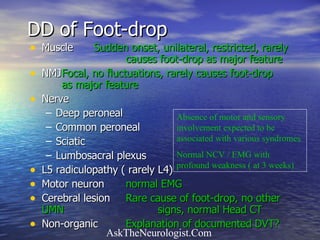
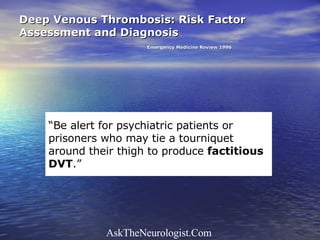
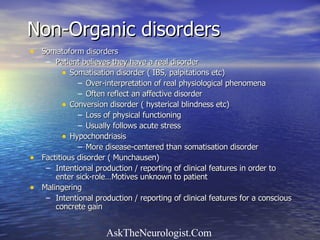
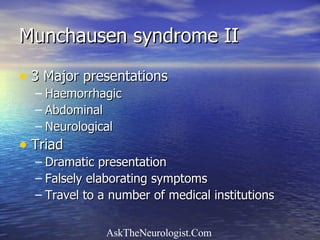
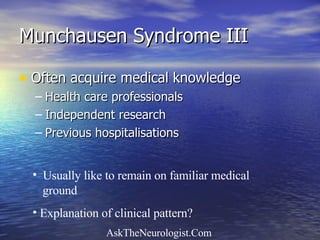
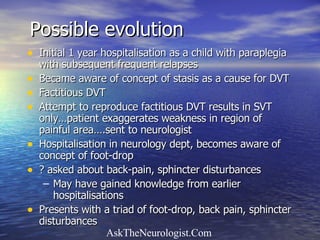
The document describes the case of a 40-year-old man presenting with right foot drop and difficulty walking. His medical history includes several episodes as a child and young adult of temporary leg paralysis without clear cause. Electrophysiology testing showed normal results inconsistent with his symptoms. His symptoms and history were inconsistent and suggestive of a non-organic or factitious disorder.