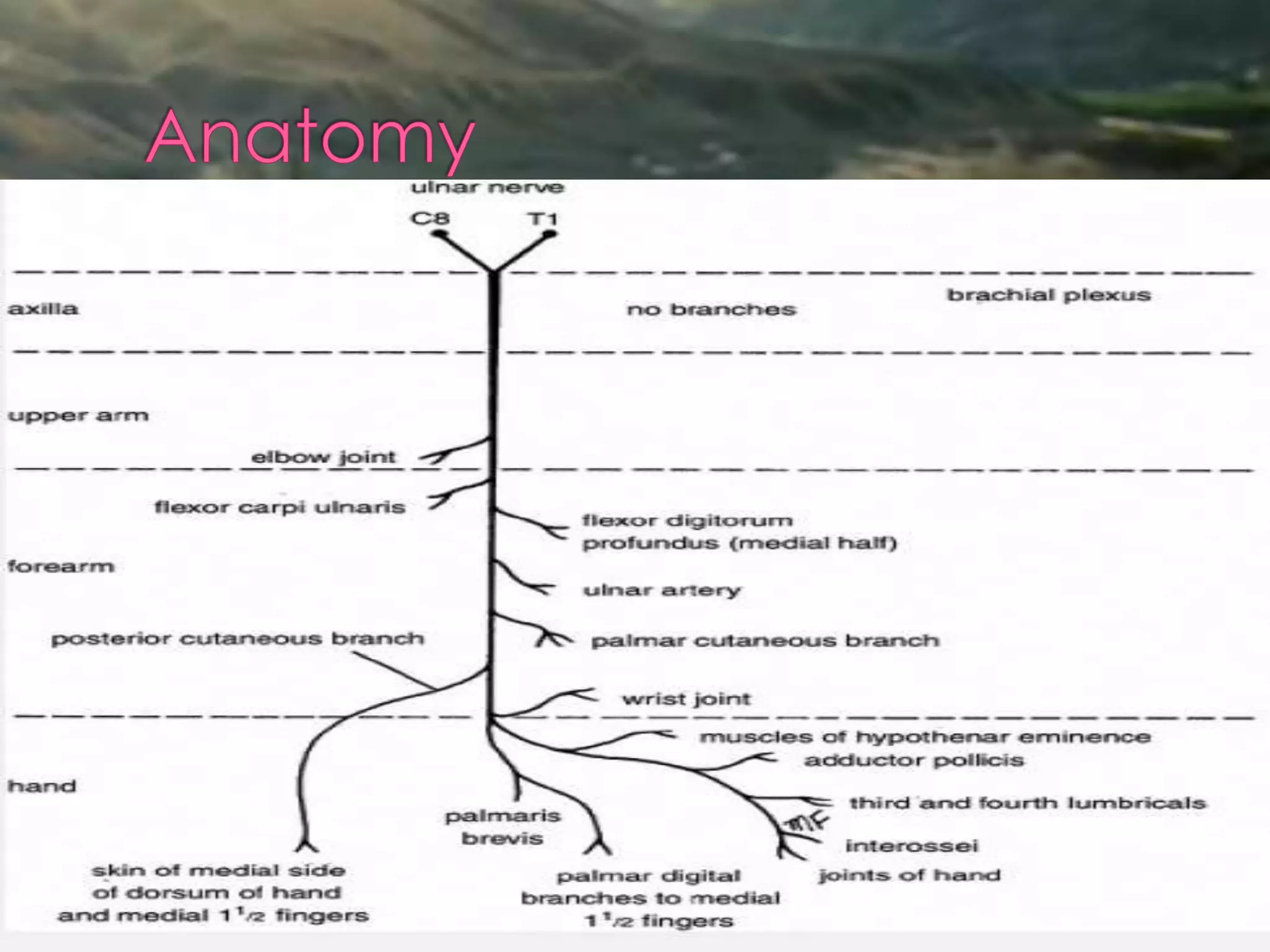
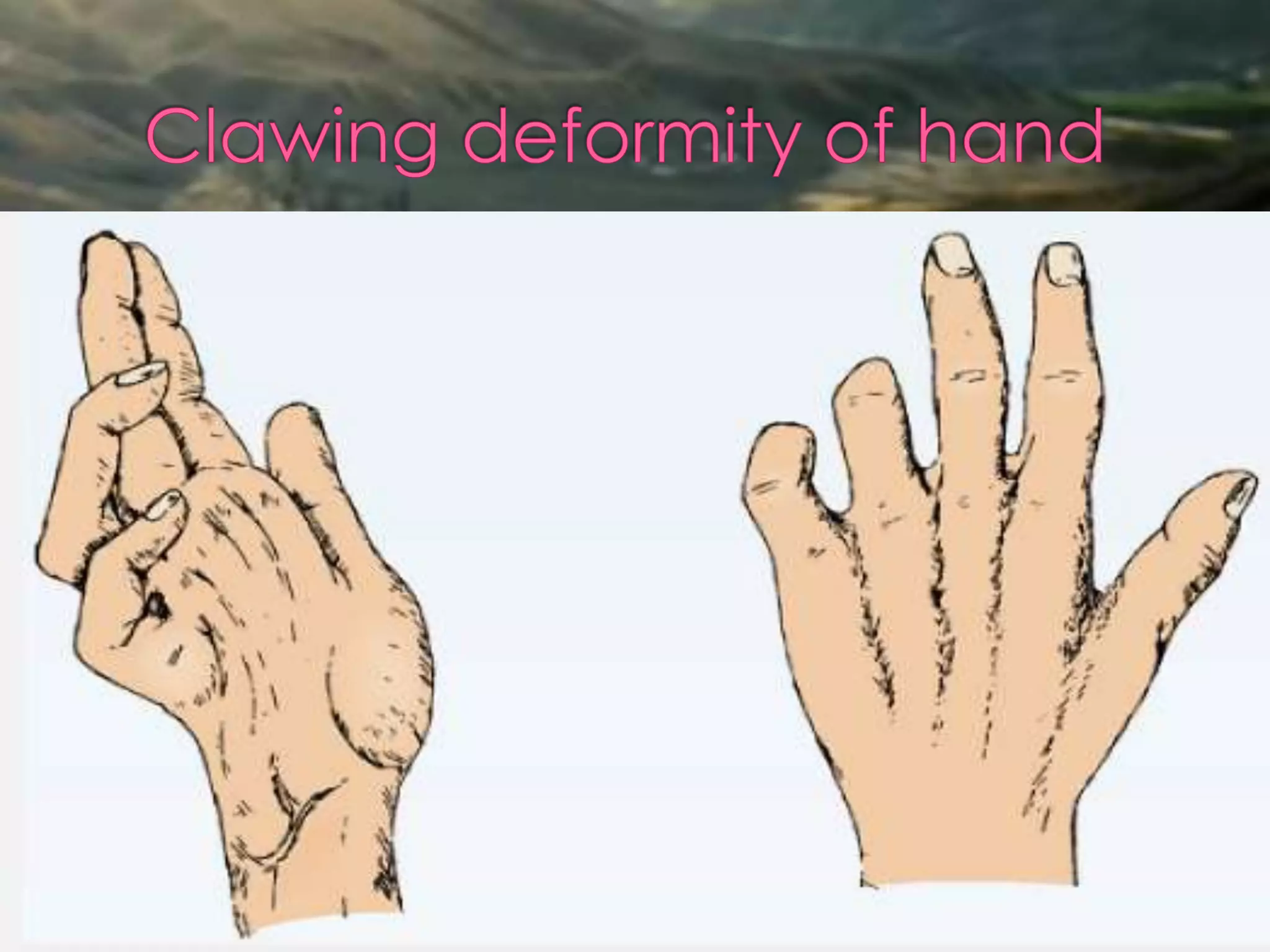
The ulnar nerve arises from the brachial plexus and supplies sensation to the palmar side of the hand and medial 1.5 fingers as well as muscles in the forearm and hand. It is most commonly injured at the elbow or wrist, which can cause sensory loss, muscle weakness or wasting, and deformities like claw hand. Surgical exploration and repair or nerve transposition are often used to treat ulnar nerve injuries.