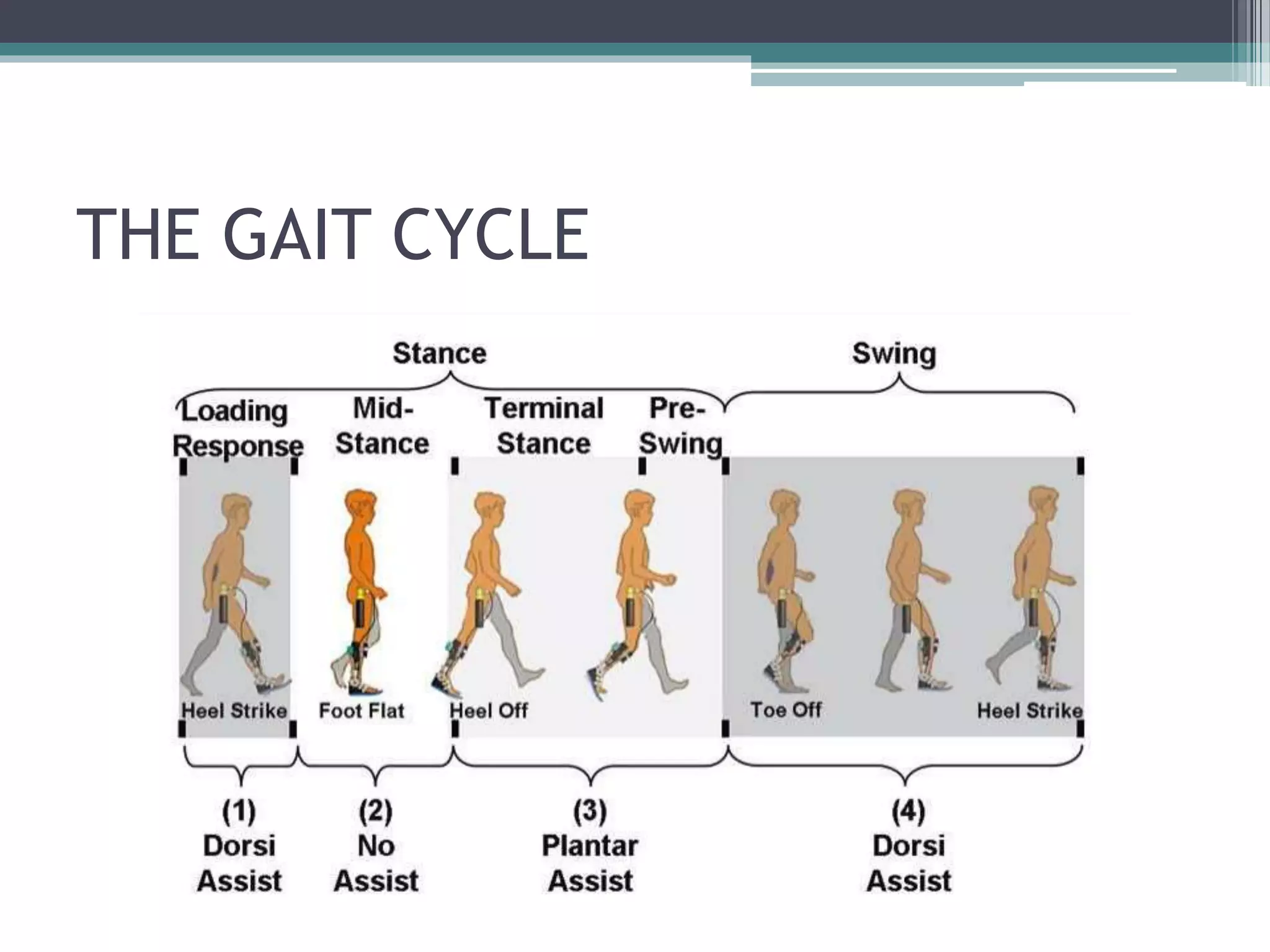
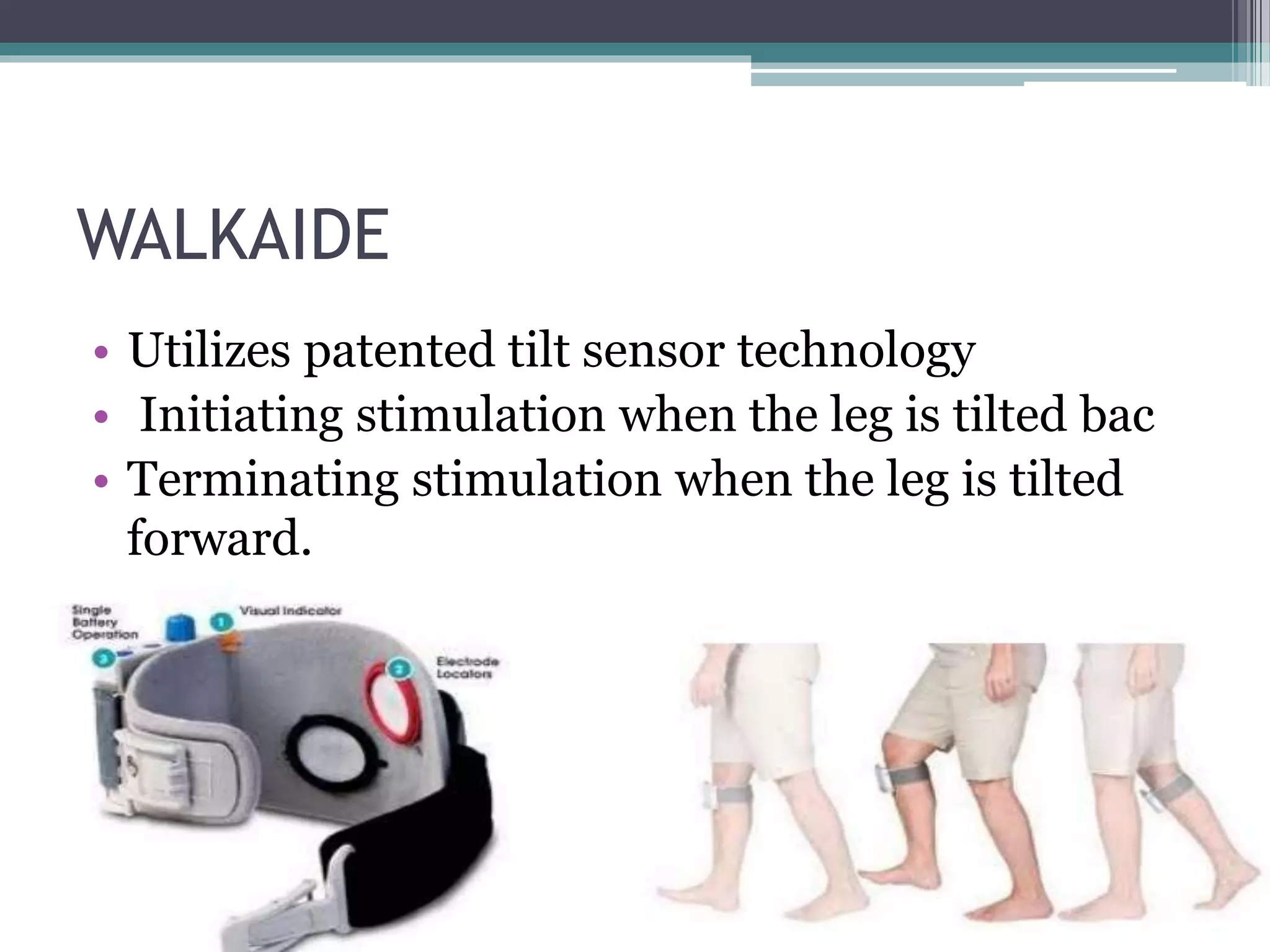
Foot drop is a symptom characterized by the inability to lift the front part of the foot, often due to nerve injury, neurological conditions, or muscle disorders. It leads to steppage gait, requiring individuals to lift their legs higher while walking, and is associated with various medical conditions such as multiple sclerosis and peroneal nerve injury. Treatment options include physical therapy, ankle foot orthotics, electrical stimulation, and, in some cases, surgery to restore a regular gait cycle.
![INTRODUCTION
• Steppage gait (High stepping, Neuropathic
gait) is a form of gait abnormality characterised
by foot drop due to loss of dorsiflexion.[1] The foot
hangs with the toes pointing down, causing the toes
to scrape the ground while walking, requiring
someone to lift the leg higher than normal when
walking.
• It can be caused by damage to the deep peroneal
nerve.
• Characterize by excessive flexion of hip and knee in
swing phase,](https://image.slidesharecdn.com/myopathicgait-200427151615/75/neuropathic-gait-and-foot-drop-2-2048.jpg)