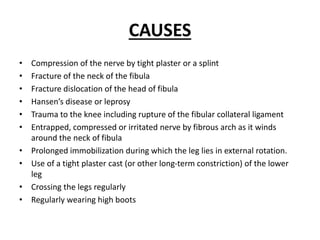
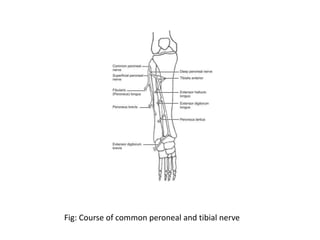
The common peroneal nerve is a crucial nerve in the lower leg that provides sensation and motor function to various muscles, particularly affecting the dorsiflexion of the foot. Common peroneal nerve palsy can result from various causes including trauma, compression, or systemic illnesses, leading to symptoms such as foot drop, weakness, and loss of sensation. Diagnosis involves electromyography and imaging techniques, while treatment options range from conservative management to surgical interventions like nerve repair and tendon transfer.