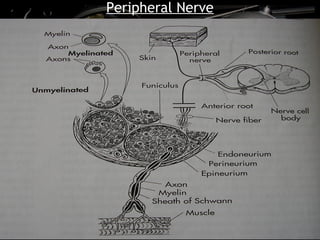
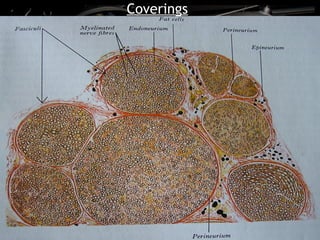
This document discusses peripheral nerve injuries, including:
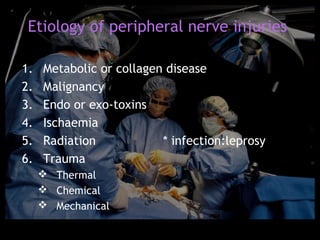
1. It describes the different types and causes of peripheral nerve injuries, including trauma, disease, ischemia, and radiation.
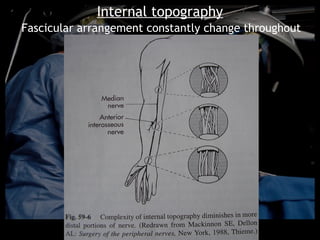
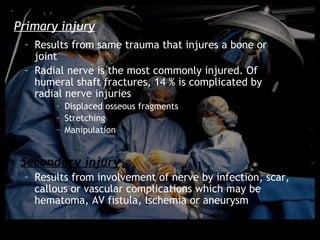
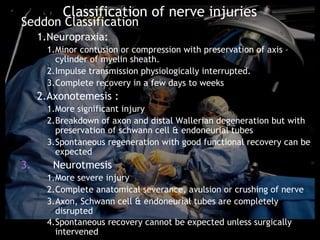
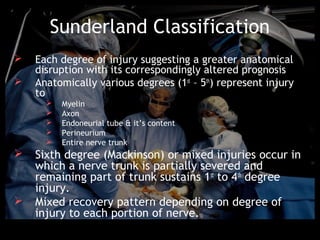
2. It outlines the primary and secondary injury mechanisms and classifies nerve injuries using the Seddon and Sunderland classifications based on the anatomical disruption.
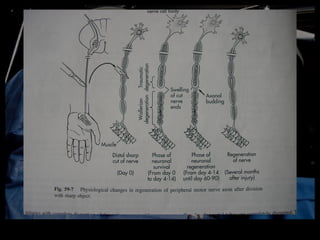
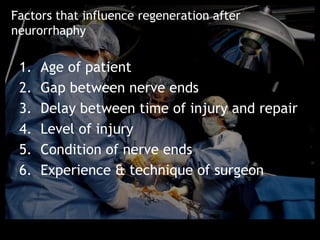
3. It explains the neuronal degeneration and regeneration process after a nerve injury.