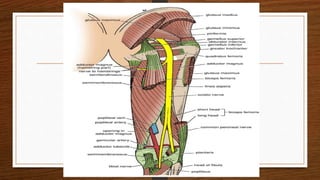
Uncle Willie woke up with weakness and difficulty lifting his left foot, a condition known as foot drop. Foot drop is caused by damage to the deep peroneal nerve and results in inability to dorsiflex the ankle. The physiotherapist examined Uncle Willie and observed these symptoms, suggesting nerve damage as the cause. Foot drop can be tested for using EMG, MRI and other tests and treated with physiotherapy, orthotics, or occasionally surgery. Physiotherapy focuses on exercises to strengthen dorsiflexors while occupational therapy provides adaptive devices.