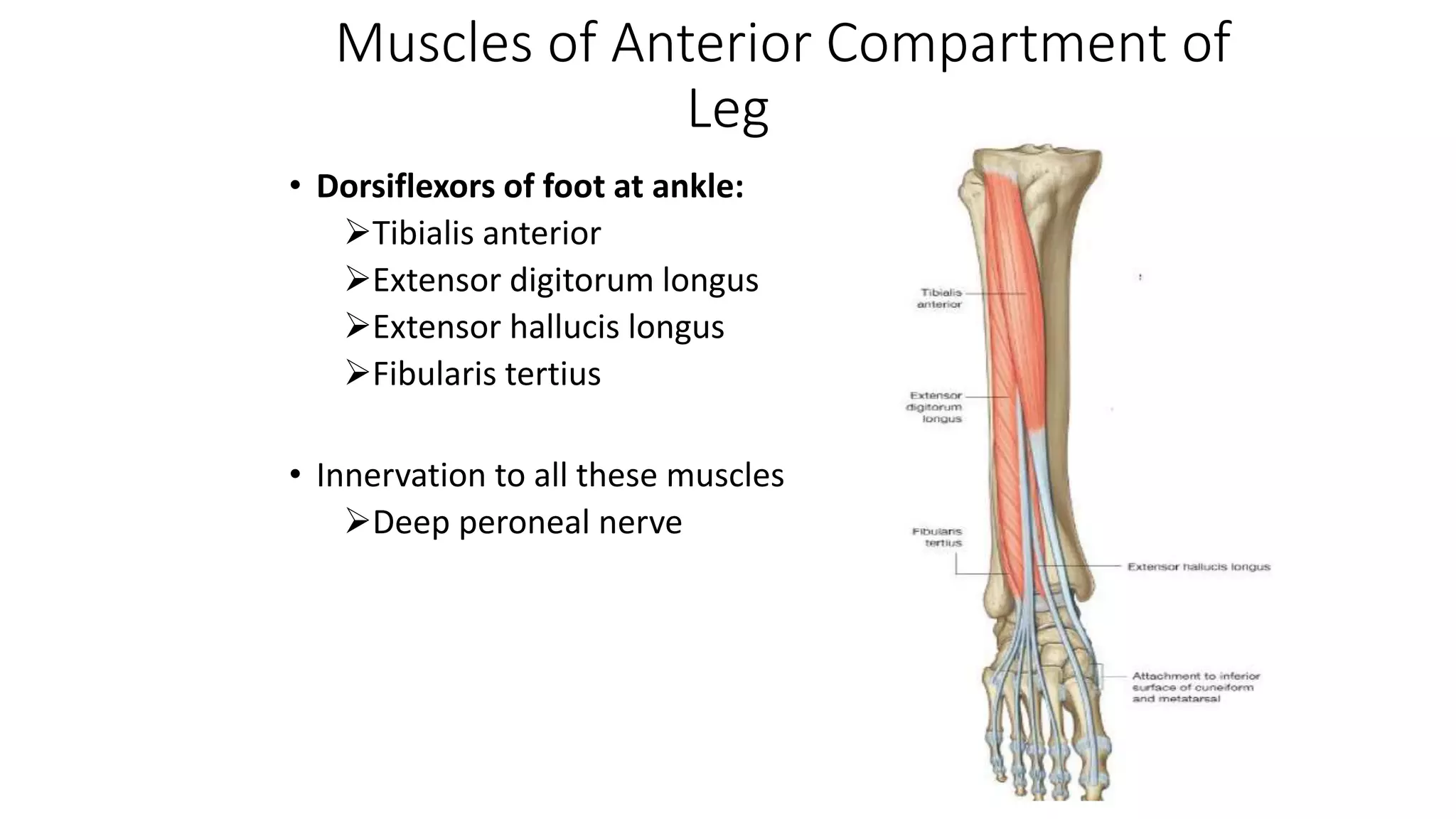
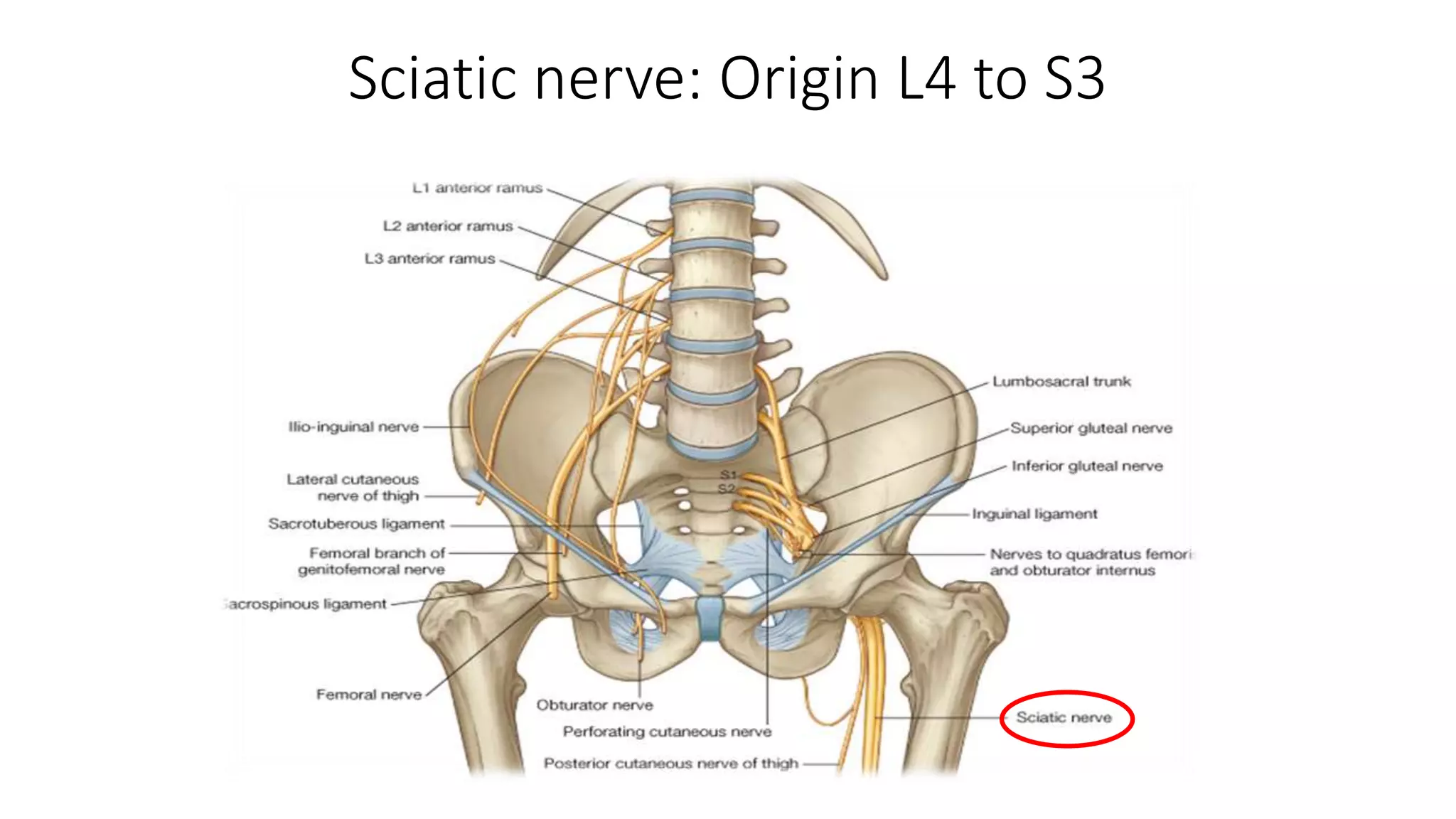
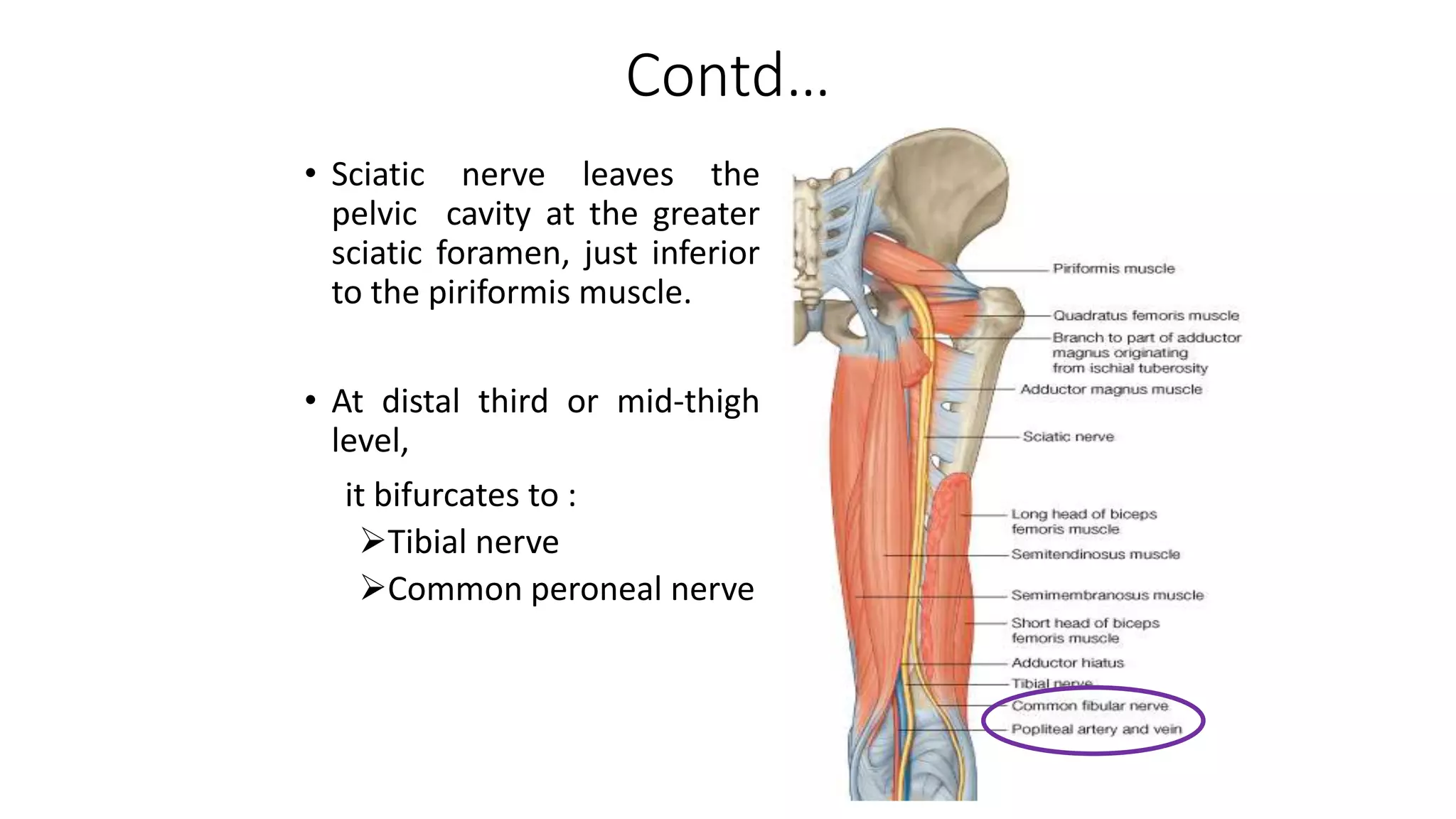
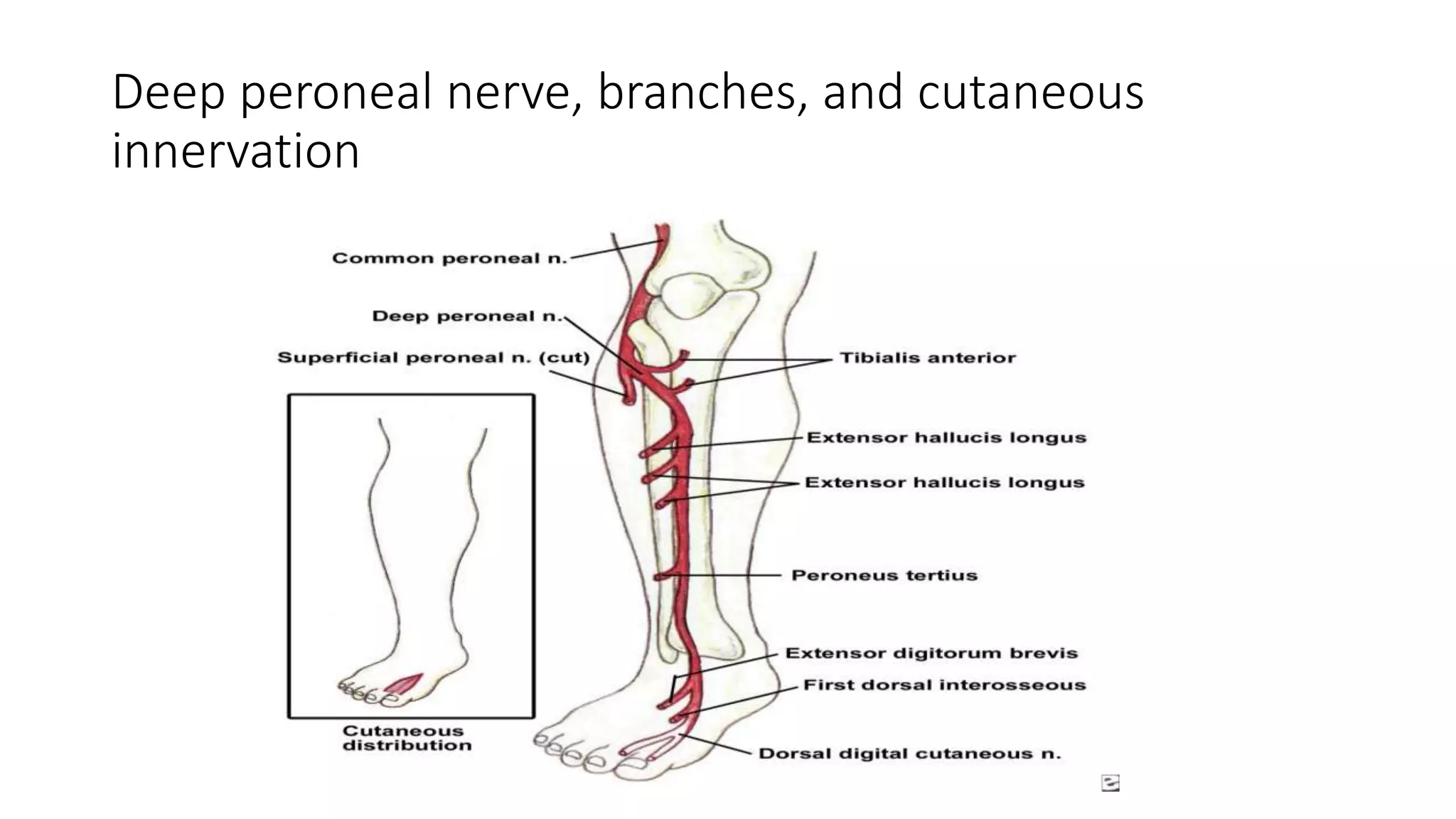
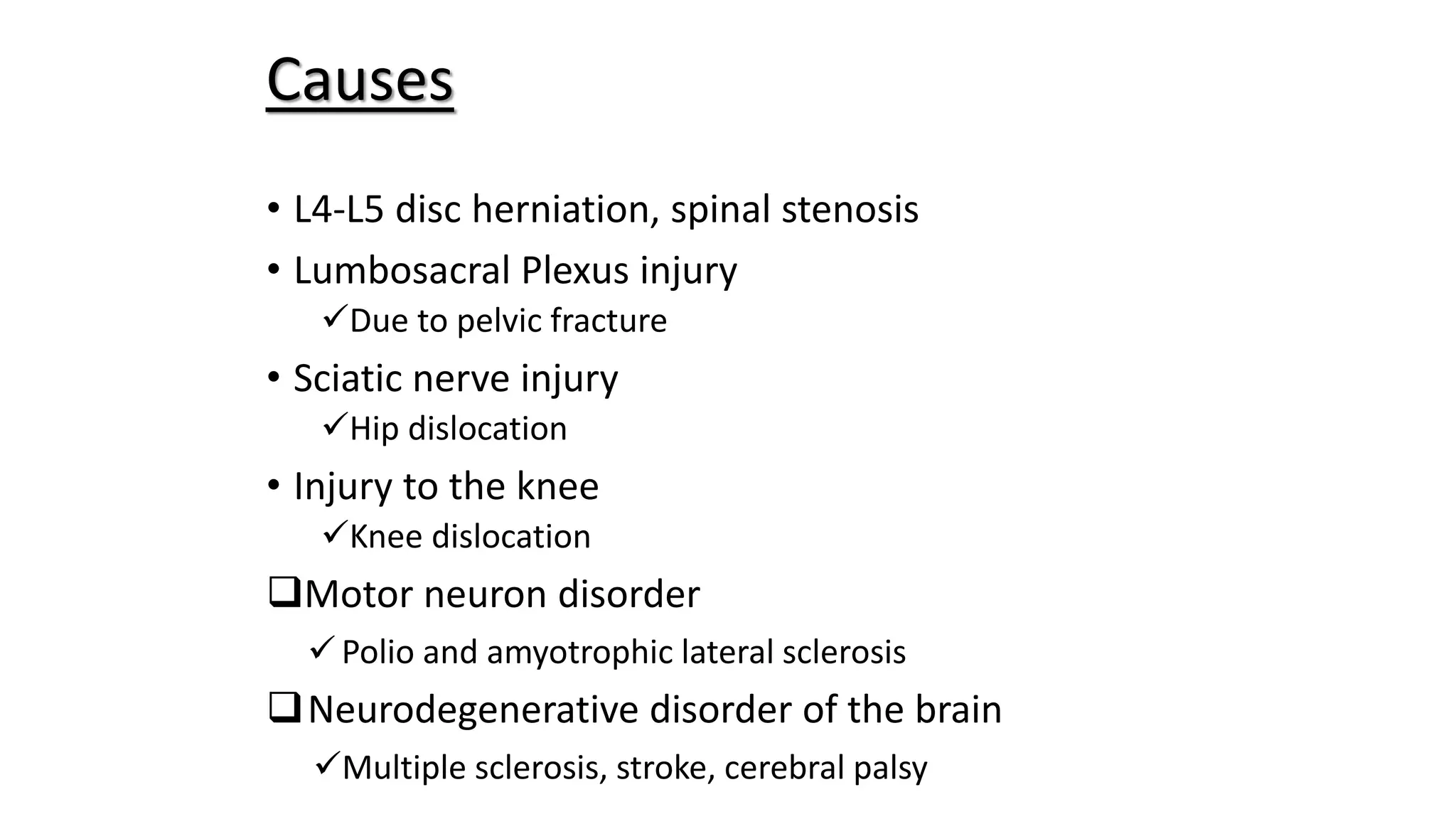
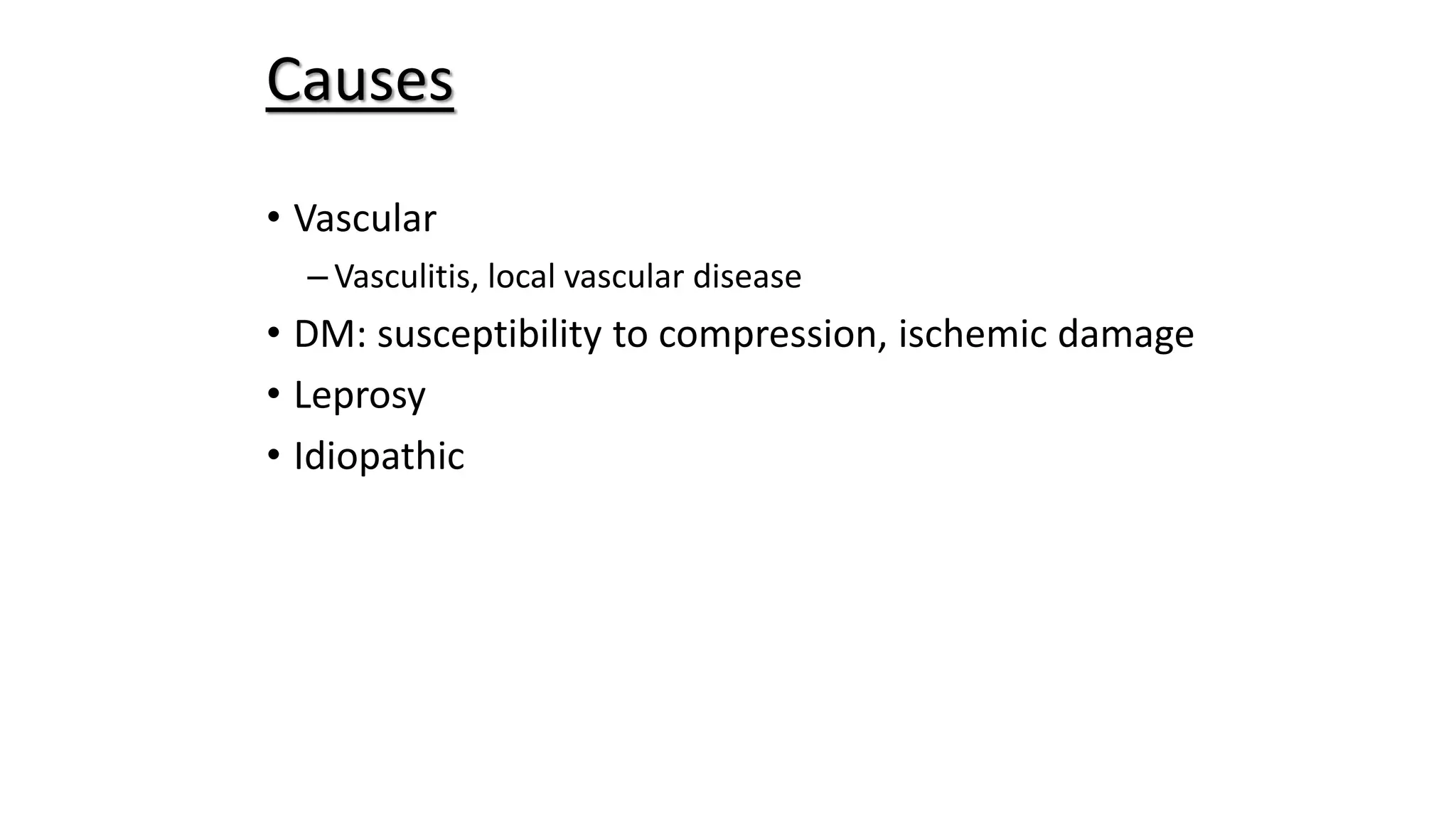
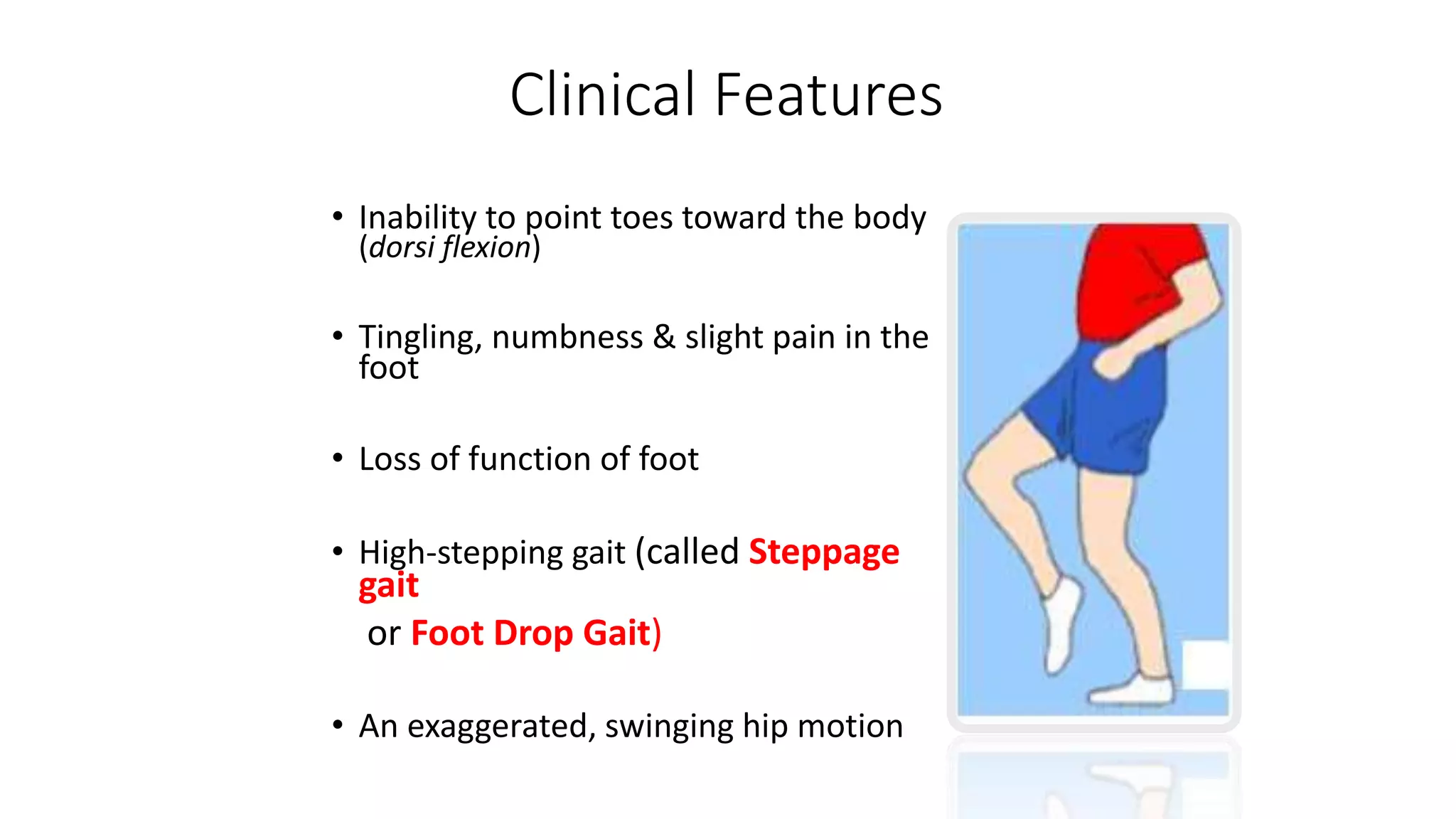
Foot drop is a condition characterized by an inability to lift the front part of the foot, which can result from injury or damage to the muscles and nerves responsible for dorsiflexion. The deep peroneal nerve is responsible for innervating the muscles that lift the foot. Causes of foot drop include issues with the lumbosacral plexus, sciatic nerve, common peroneal nerve, or the muscles themselves due to conditions such as multiple sclerosis, disc prolapse, or trauma. Symptoms include an inability to point the toes up, tingling/numbness in the foot, and an exaggerated swinging gait known as steppage gait. Treatment options include orthotics, physical therapy, nerve