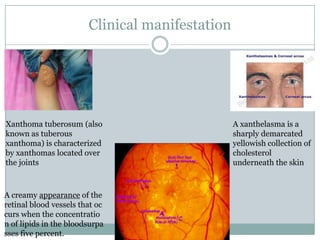
Hyperlipidemia is a condition marked by abnormally high levels of lipids in the blood. It can be caused by primary genetic disorders affecting lipid metabolism or secondary factors like hypothyroidism, obesity, and certain medications. Clinical manifestations include fatty deposits in the skin called xanthomas and cholesterol deposits in the eyes seen on fundoscopy. Long-term complications arise from atherosclerosis driven by chronically elevated cholesterol, increasing risks of heart attack, stroke, and peripheral vascular disease. Diagnosis involves lipid profile blood tests to classify lipid abnormalities and their underlying causes.




![Lipid Metabolism
Endogenous = Liver {De Novo Synthesis}
(VLDL→IDL→LDL) [Apo B 100]
Exogenous= Intestine {From Diet}
(Chylomicron→Chylomicron Remnants) [Apo B 48]
HDL
[Apo C II ’Activate
Lipoproten Lipase’
, Apo E ’Liver
Recognition’ ]](https://image.slidesharecdn.com/hyperlipidimea-140415052734-phpapp02/85/Hyperlipidimea-5-320.jpg)





















![ Palmar xanthoma is clinically characterized by
yellowish plaques that involve the palms and
flexural surfaces of the fingers.[1]:531 Plane
xanthomas are characterised by yellowish to
orange, flat macules or slightly elevated
plaques, often with a central white area which may
be localised or generalised. They often arise in the
skin folds, especially the palmar creases. They
occur in hyperlipoproteinaemia type III and type
IIA, and in association with biliary cirrhosis. The
presence of palmar xanthomata, like the presence
of tendinous xanthomata, is indicative of
hypercholesterolaemia.
Eruptive xanthoma is
clinically characterized by
small, yellowish-orange to
reddish-brown papules
that appear all over the
body.It tends to be
associated with elevated
triglycerides](https://image.slidesharecdn.com/hyperlipidimea-140415052734-phpapp02/85/Hyperlipidimea-28-320.jpg)
