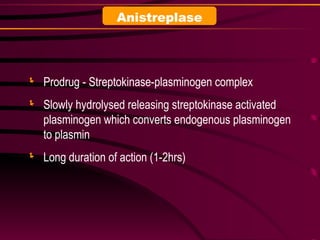
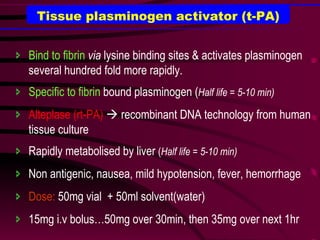
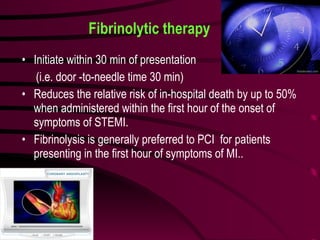
Fibrinolytics, also known as thrombolytics, work to dissolve blood clots and are used to treat conditions like heart attacks, deep vein thrombosis, and pulmonary embolism. The main fibrinolytic agents discussed are streptokinase, tissue plasminogen activator (t-PA), and its variants reteplase and tenecteplase. These work by activating plasminogen and converting it to plasmin to break down fibrin clots. Their use comes with risks of hemorrhage, so antifibrinolytic drugs like tranexamic acid and aminocaproic acid are used to reduce bleeding when fibrinolytics are given.
![FIBRINOLYTICS [THROMBOLYTICS] DR.SOMASHEKARA.S.C DEPARTMENT OF PHARMACOLOGY SVS MEDICAL COLLEGE](https://image.slidesharecdn.com/fibrinolyticagents-101009115626-phpapp02/85/Fibrinolytic-agents-1-320.jpg)