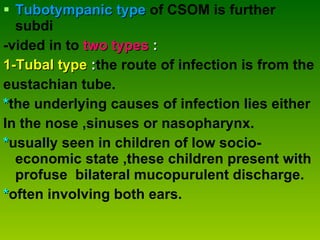
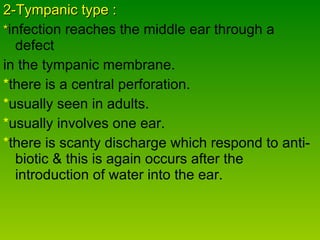
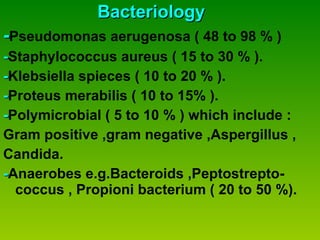
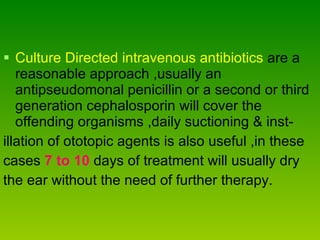
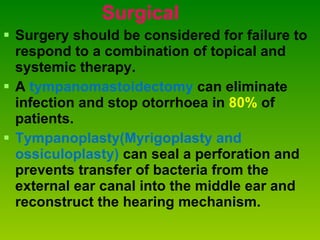
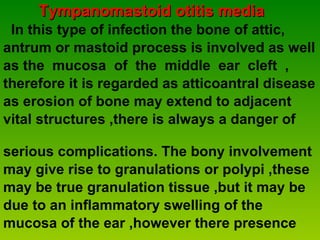
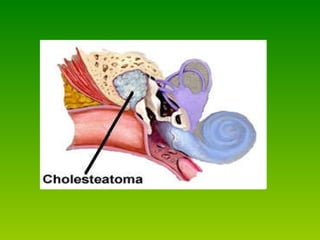
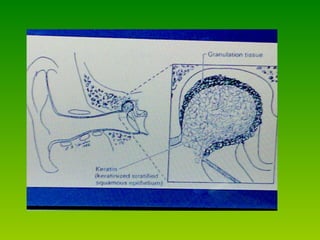
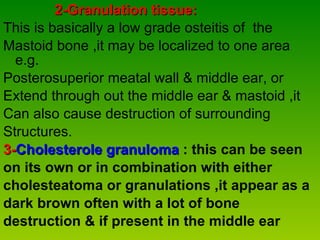
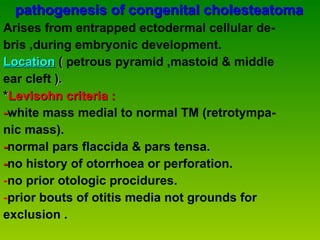
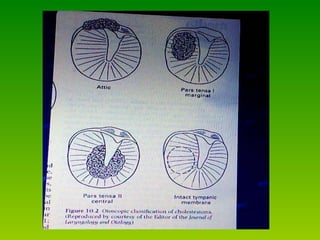
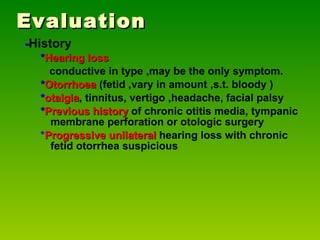
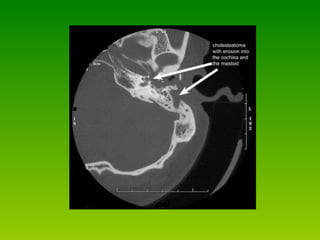
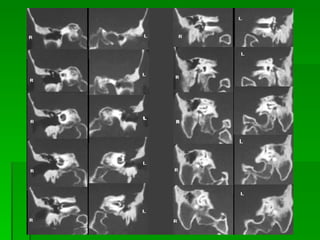
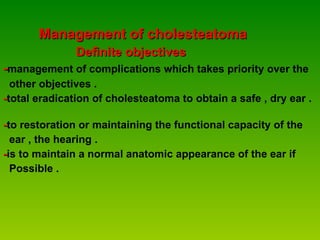
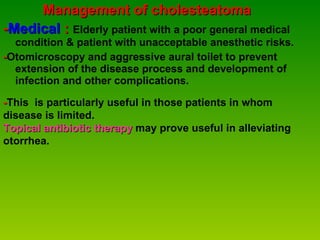
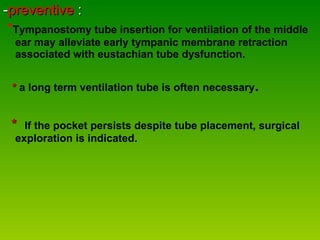
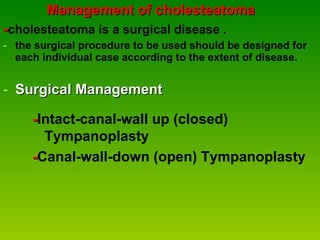
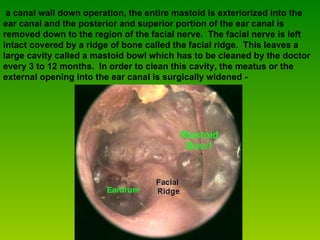
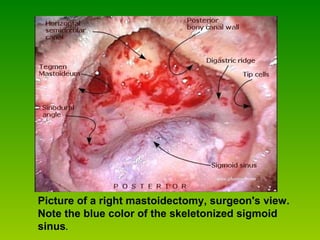
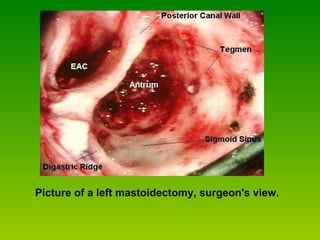
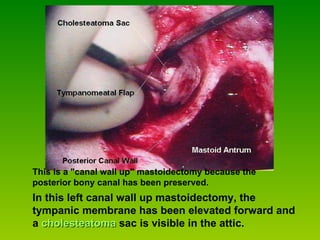
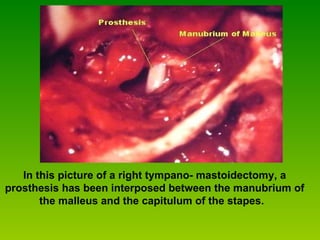
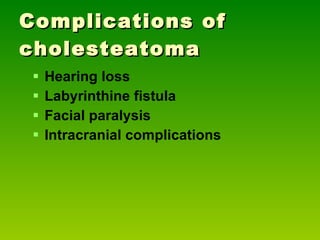
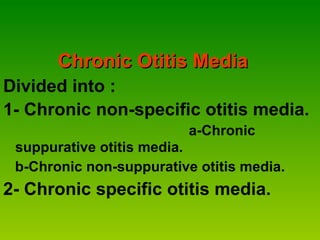
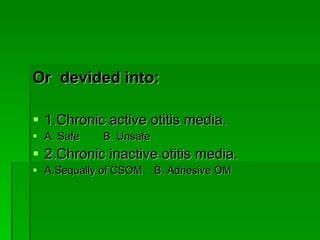
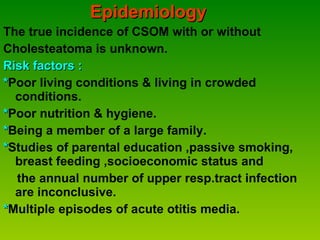
This document provides an overview of chronic otitis media, including its definition, classification, clinical features, treatment, and epidemiology. It is divided into chronic nonspecific otitis media and chronic specific otitis media. Chronic suppurative otitis media is further classified as tubotympanic disease or atticoantral disease, with the latter including cholesteatoma, granulation tissue, or cholesterol granuloma involvement. Treatment involves antibiotics, surgery for refractory cases, and tympanoplasty to repair perforations and reconstruct hearing.

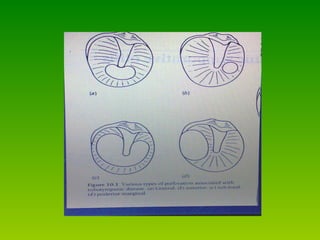
![Tubotympanic disease * Charactrised by a perforation of the pars tensa [ central perforation ] . * adequate atticoantral drainage. * disease confirm to the mucosa of the antero- inferior portion of the middle ear cleft. * risk of serious complication is minimal. * most perforations arise when an acute perforation occurs during an episodes of acute suppurative otitis media.](https://image.slidesharecdn.com/com-111206132312-phpapp01/85/E-N-T-COM-dr-hewa-10-320.jpg)