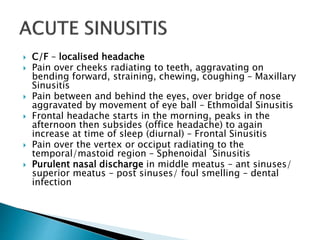
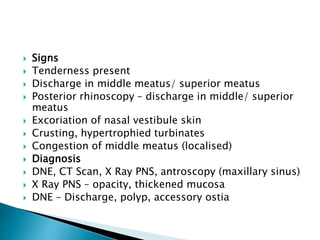
This document discusses sinusitis, including definitions of types of sinusitis, causes, symptoms, signs, investigations, treatments, and complications. It defines acute, subacute and chronic sinusitis. Maxillary sinusitis is the most common type. Causes include viral and bacterial infections, mechanical obstruction, allergic rhinitis, and trauma. Symptoms vary depending on the affected sinus. Investigations include endoscopy, x-ray, and CT scan. Treatment involves antibiotics, nasal irrigation, and sometimes surgery. Complications can include orbital cellulitis if the infection spreads.