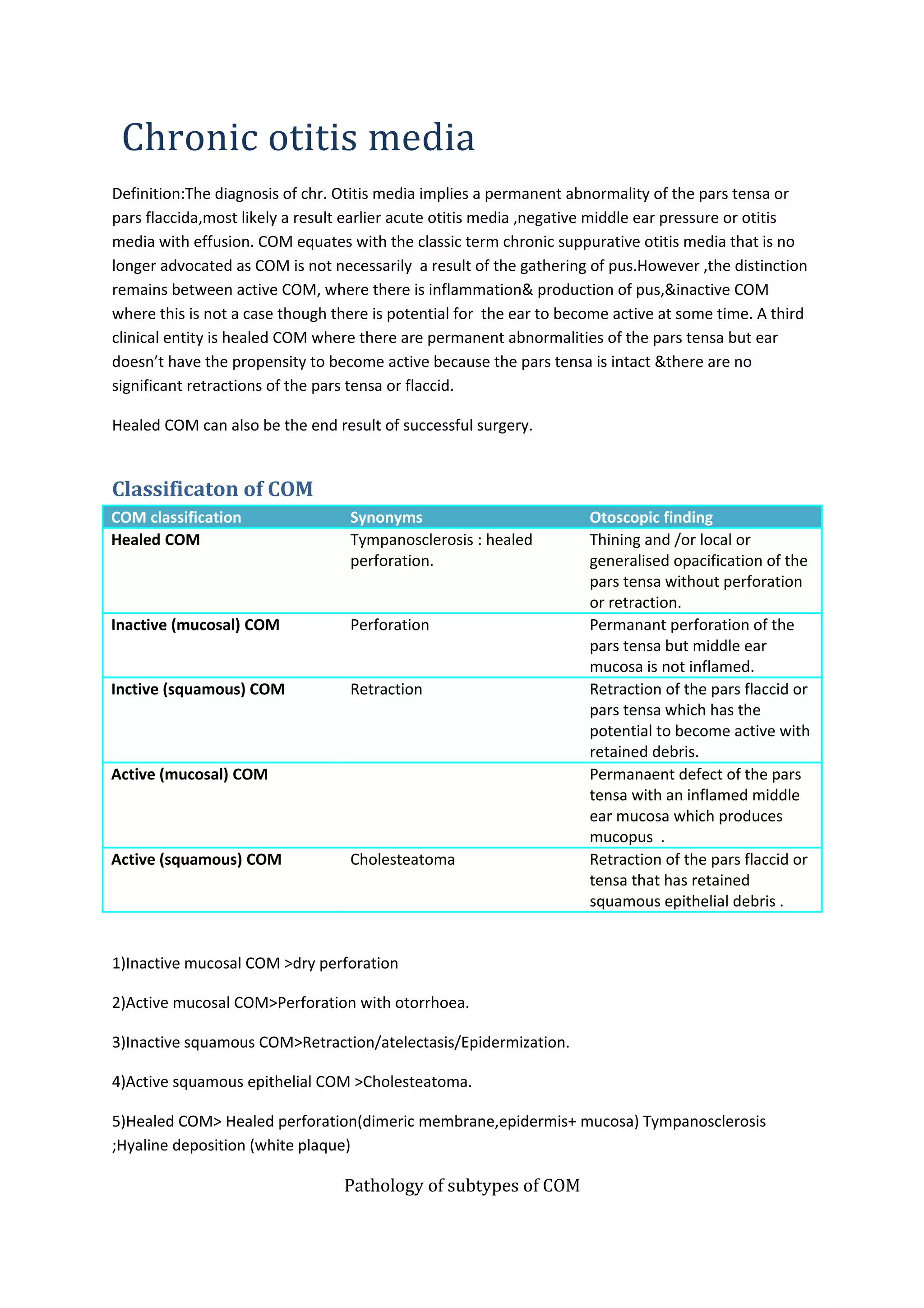
1) Chronic otitis media (COM) refers to permanent abnormalities of the eardrum or middle ear bones caused by previous ear infections. It is classified into several subtypes based on symptoms and examination findings.
2) Inactive mucosal COM involves a dry perforation of the eardrum, while active mucosal COM shows inflammation and discharge through a perforation. Inactive squamous COM includes retraction pockets without debris, while active squamous COM features cholesteatoma with retained skin and potential to destroy local bones.
3) Complications of COM can arise from the spread of infection through direct bone erosion, preformed pathways, or blood vessels. This may lead to labyrinth