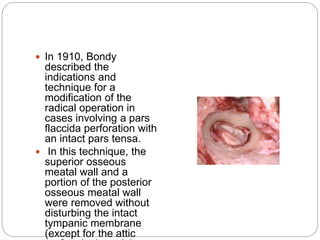
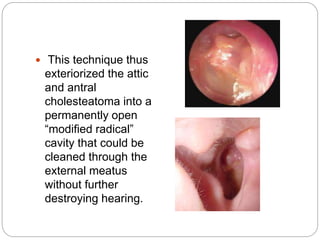
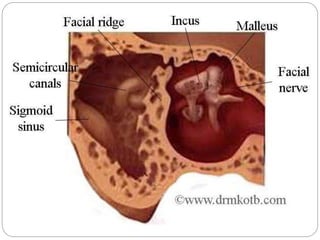
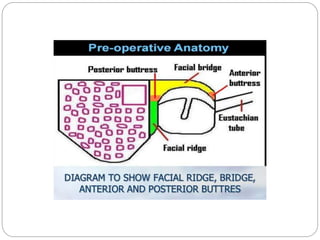
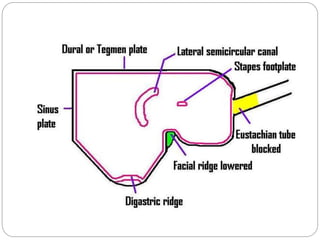
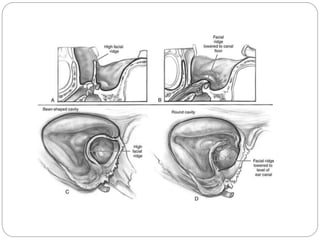
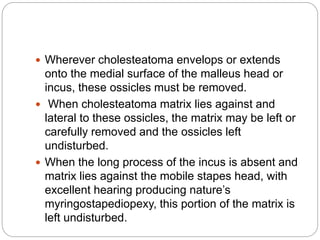
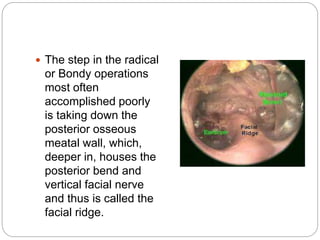
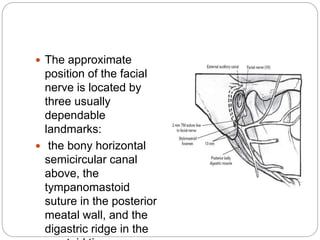
This document discusses open cavity mastoid operations, including their history, indications, techniques, and complications. Open cavity procedures involve removing the posterior wall of the external auditory canal to exteriorize the mastoid cavity. They allow for monitoring of recurrent cholesteatoma and drainage for unresectable infections. The radical and modified radical mastoidectomies developed historically to fully remove bone-invading disease while preserving hearing when possible. Key steps involve identifying and preserving the facial nerve while removing disease-affected areas. Postoperative care focuses on re-epithelialization of the cavity and monitoring for complications like infection, nerve injury, and recurrent cholesteatoma.