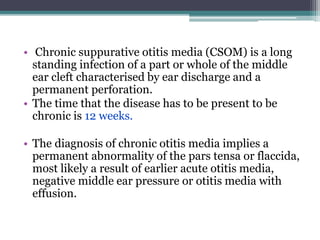
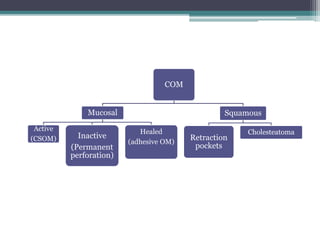
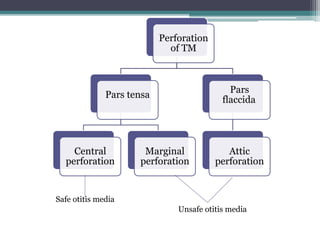
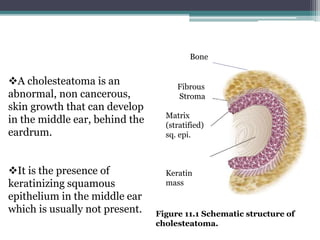
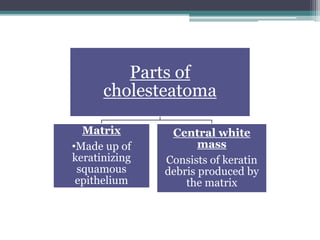
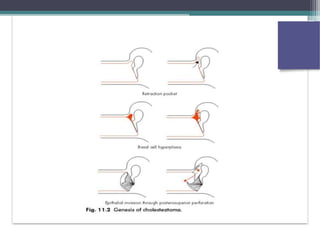
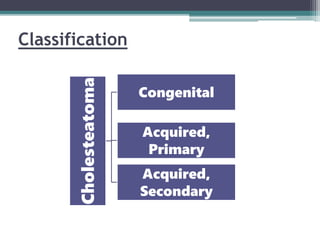
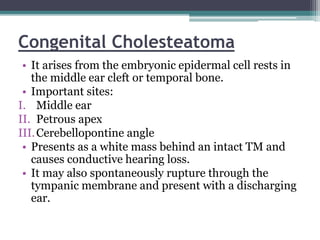
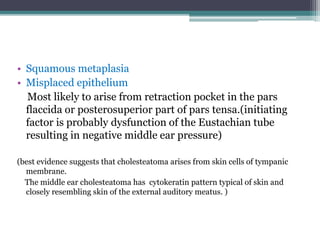
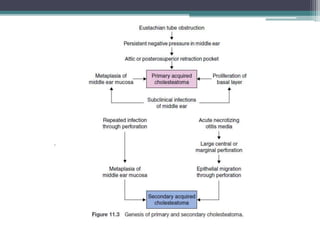
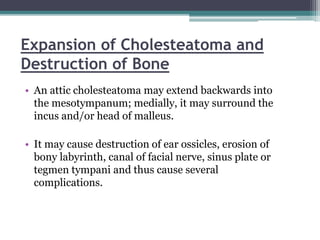
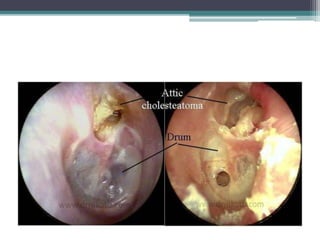
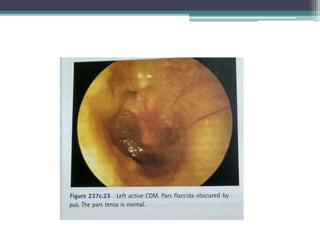
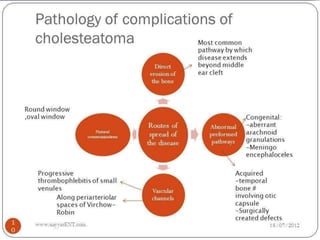
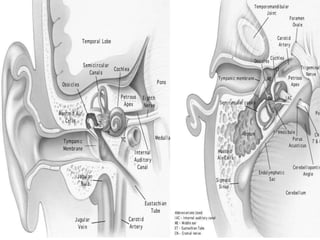
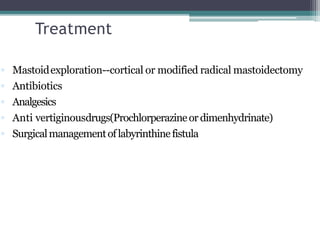
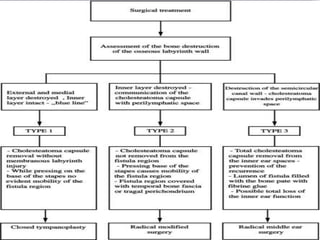
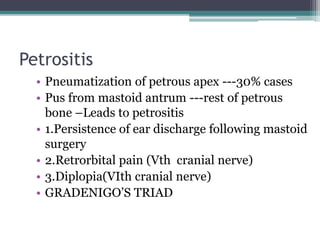
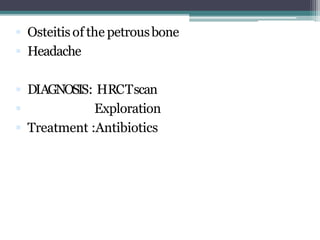
Chronic suppurative otitis media (CSOM) is a long-standing ear infection characterized by ear discharge and permanent ear drum perforation. It can lead to complications like cholesteatoma, a non-cancerous skin growth in the middle ear that causes bone destruction. Cholesteatoma is classified as congenital, primary acquired, or secondary acquired based on its origin. It expands over time and can erode bones in the middle ear. Treatment involves surgical removal of the cholesteatoma and reconstruction of the ear structures.