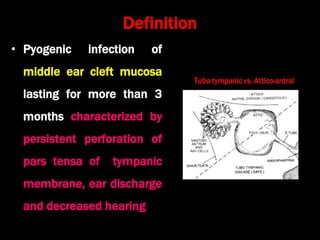
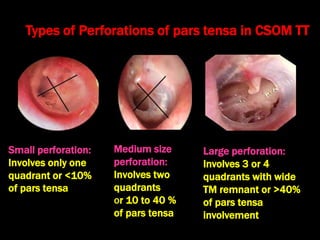
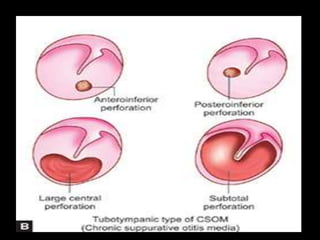
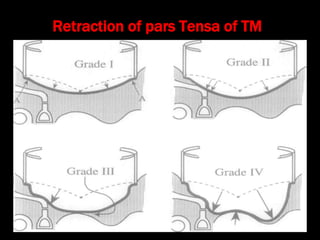
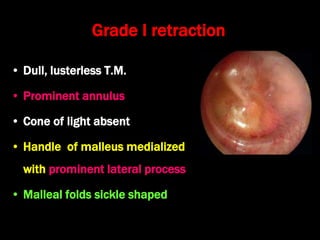
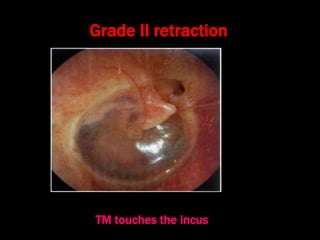
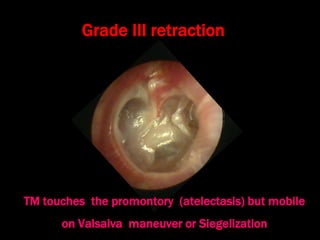
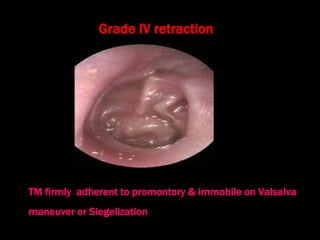
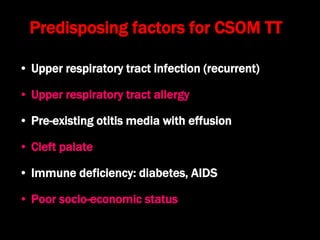
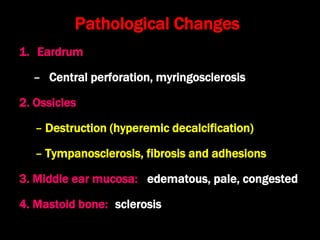
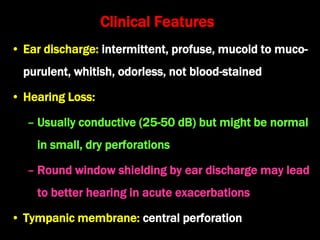
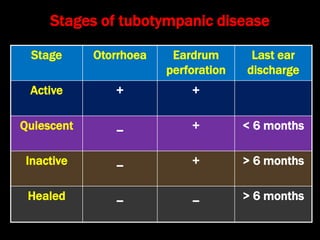
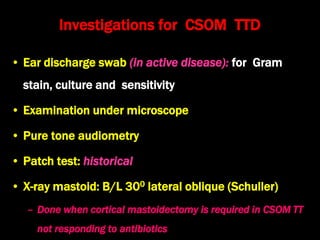
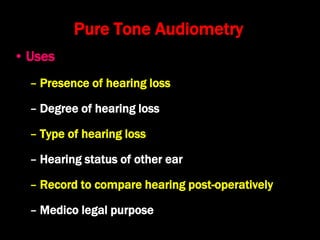
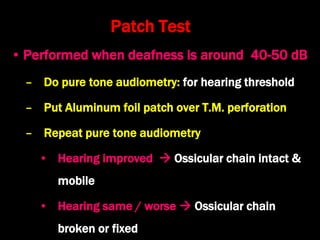
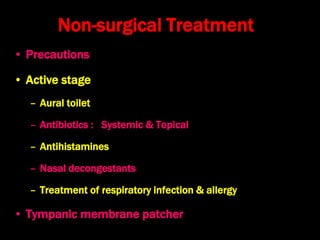
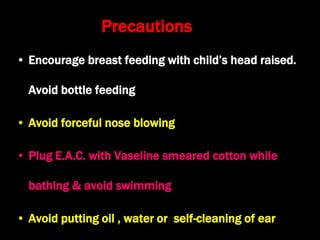
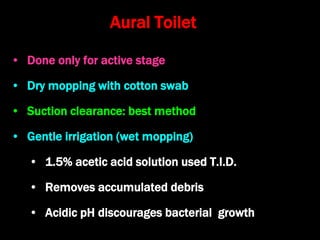
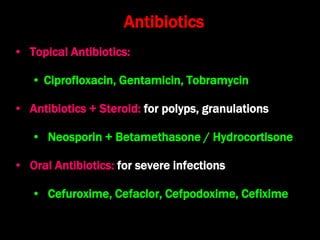
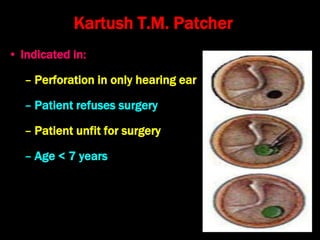
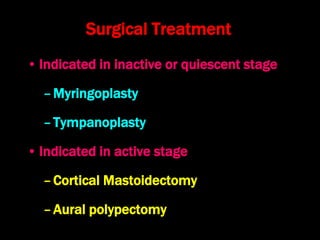
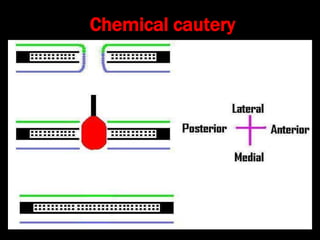
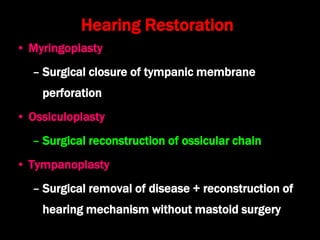
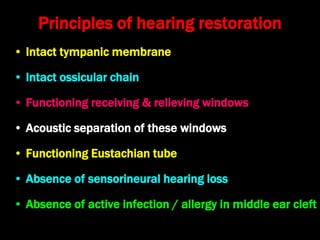
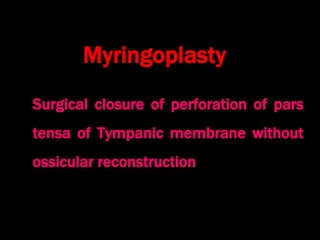
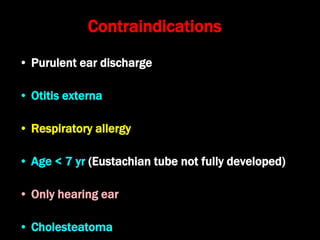
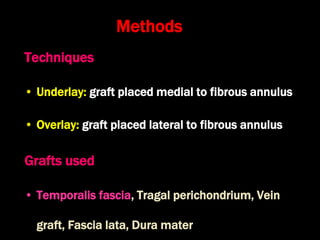
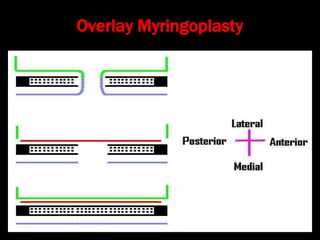
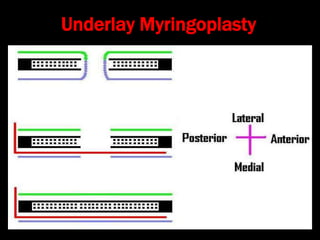
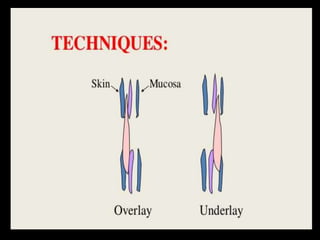
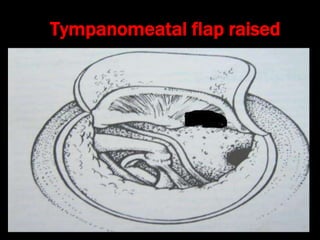
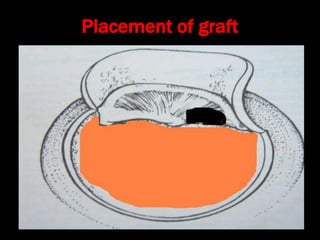
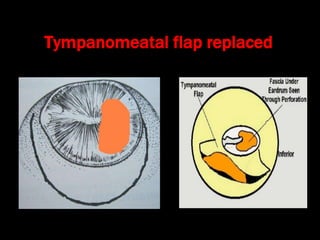
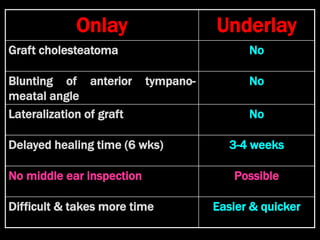
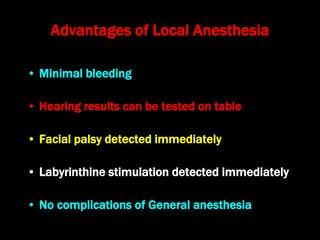
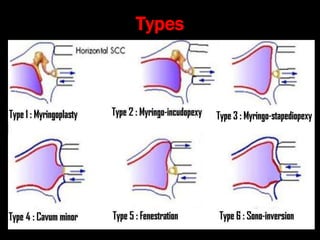
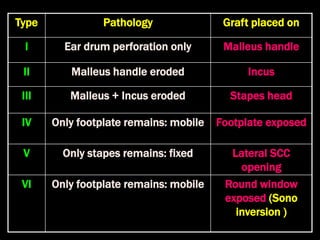
This document discusses chronic suppurative otitis media tubotympanic disease (CSOM TT). It defines CSOM TT as a pyogenic middle ear infection lasting over 3 months with persistent tympanic membrane perforation and ear discharge. It describes the types and sizes of tympanic membrane perforations, stages of the disease, predisposing factors, pathological changes, clinical features, investigations including audiometry and microscopy, and treatment approaches including non-surgical and surgical options like myringoplasty and tympanoplasty. Surgical treatment aims to close perforations, restore hearing, and stop ear discharge.