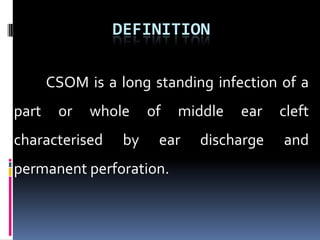
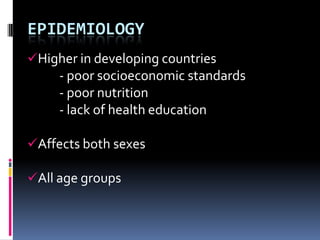
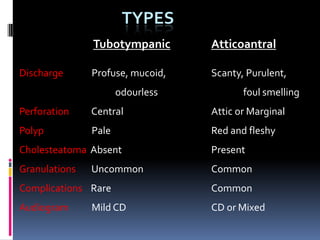
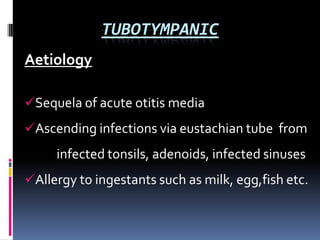
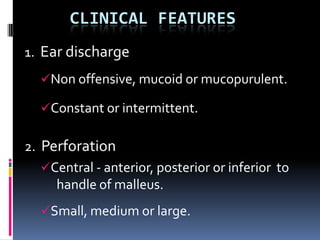
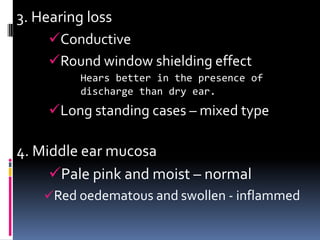
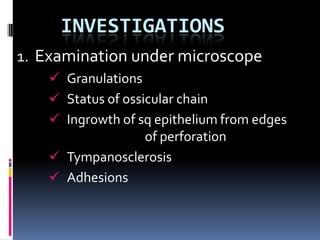
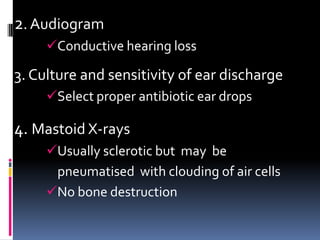
Chronic Suppurative Otitis Media (CSOM) is a persistent ear infection characterized by discharge and perforation of the eardrum, primarily affecting individuals in developing countries due to poor health conditions. It has various types based on discharge characteristics, complications, and audiometric findings, with potential causes including prior acute otitis media and allergies. Treatment focuses on infection control, removal of discharge, and restoring hearing through medical or surgical interventions.