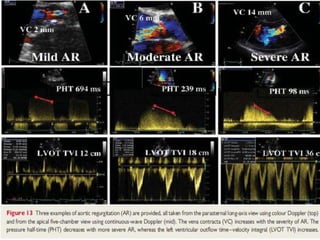
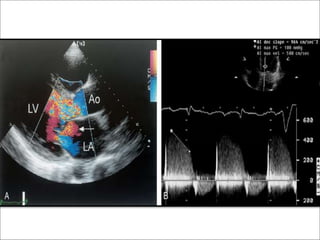
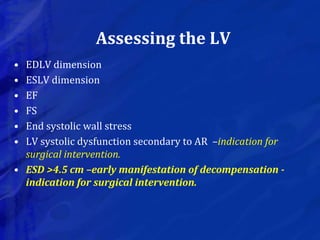
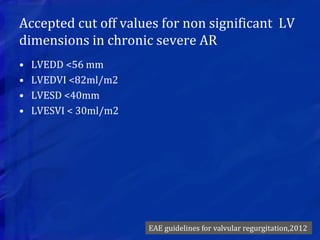
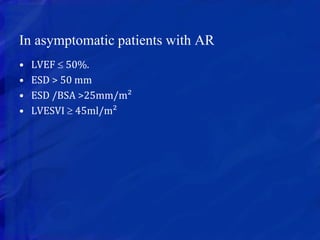
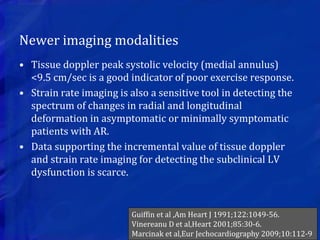
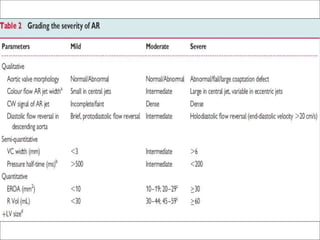
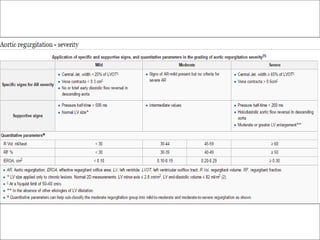
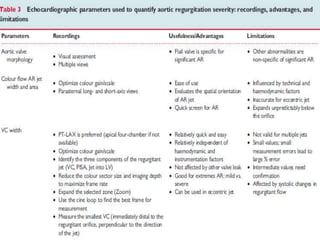
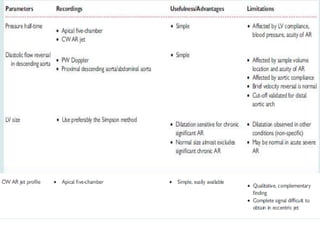
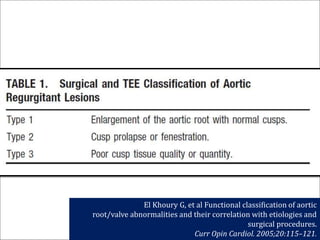
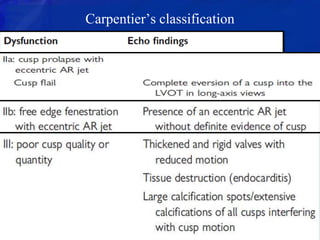
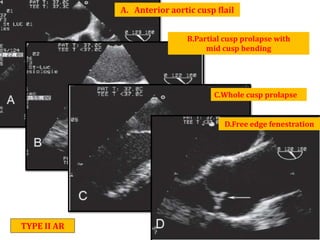
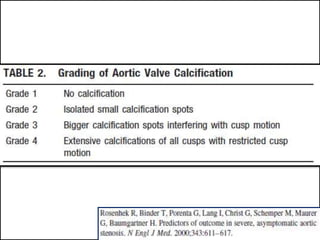
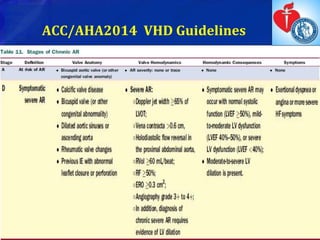
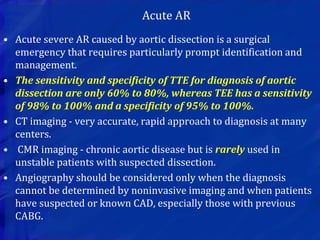
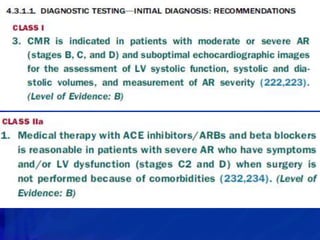
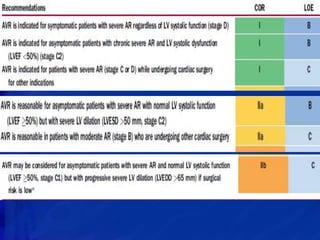
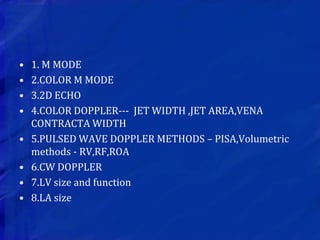
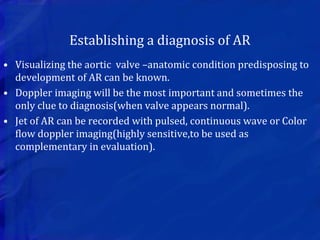
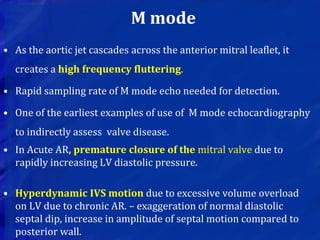
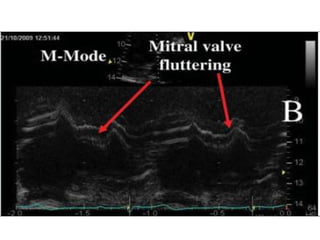
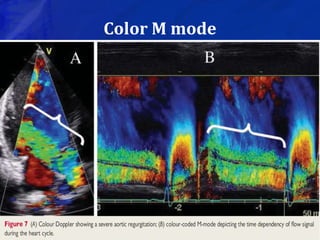
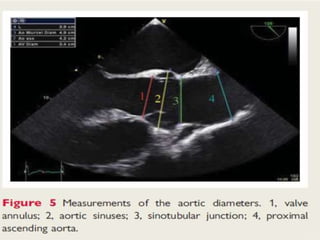
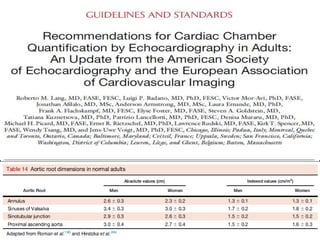
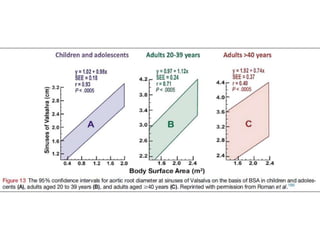
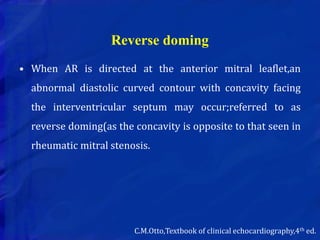
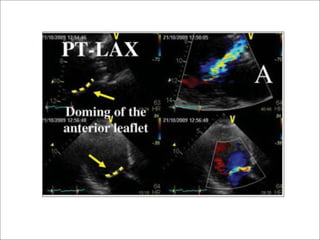
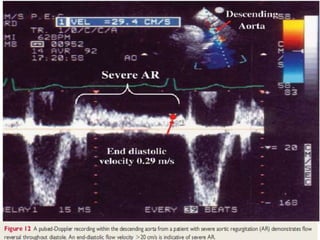
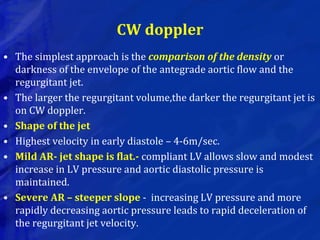
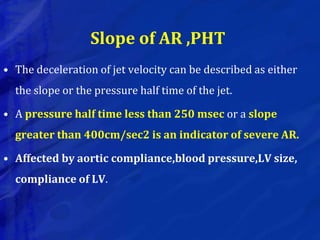
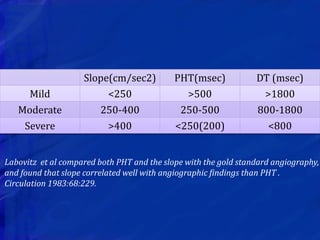
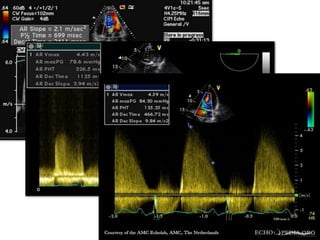
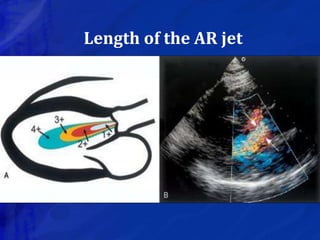
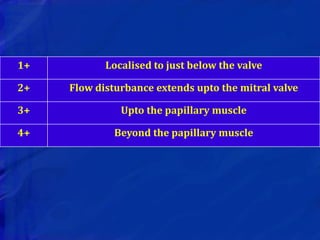
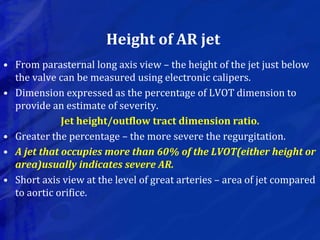
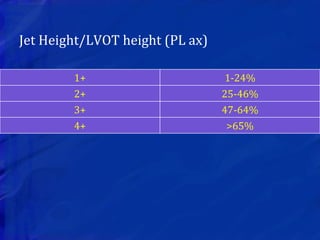
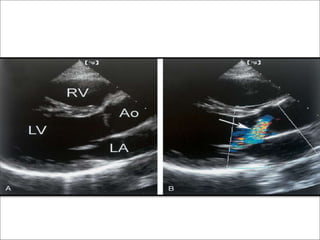
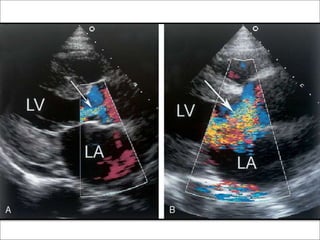
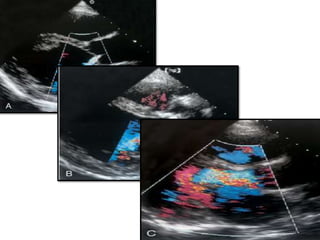
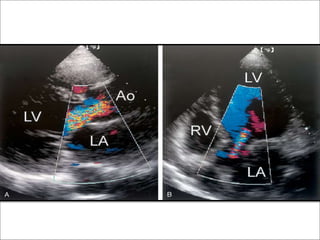
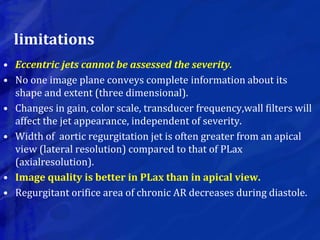
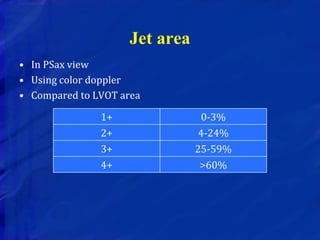
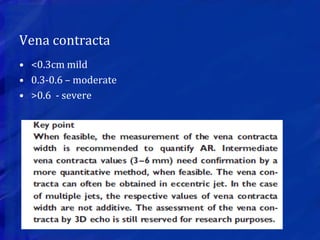
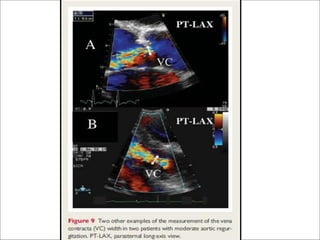
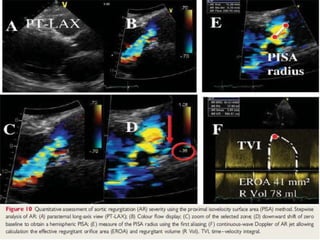
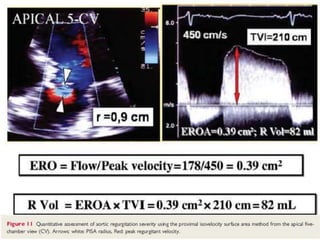
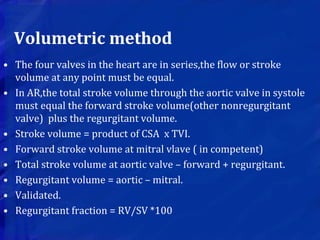
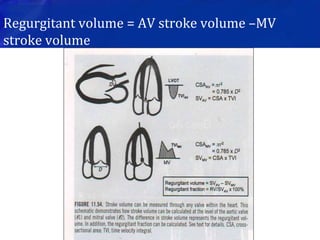
This echocardiographic evaluation document discusses the assessment of aortic regurgitation (AR) using echocardiography. It begins by outlining the etiologies of AR including congenital, acquired, and specific causes like rheumatic heart disease. It then details the echocardiographic approach to evaluating AR, including M-mode, 2D imaging, and various Doppler techniques to assess presence, etiology, severity, and effects on ventricular size and function. Cut-off values are provided to determine severity and guidelines for intervention in chronic AR based on left ventricular dimensions. The differences in acute versus chronic AR are also summarized.



![Regurgitant fraction
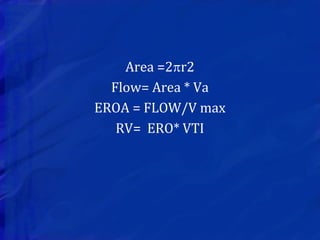
• Xie et al – simple method for calculation.
• Only mitral and aortic VTI are required.
• RF = {1 – (1/0.77)} [VTI mitral /VTI aortic]](https://image.slidesharecdn.com/echoinar-180722061302/85/ECHOCARDIOGRAM-IN-AORTIC-REGURGITATION-AR-66-320.jpg)