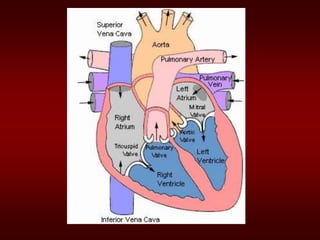
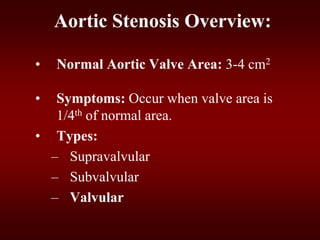
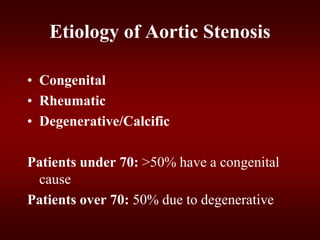
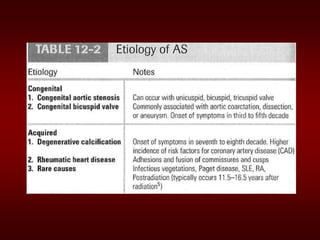
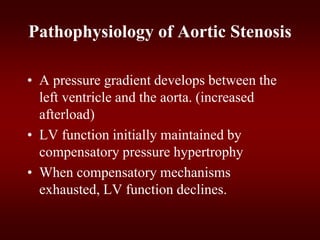
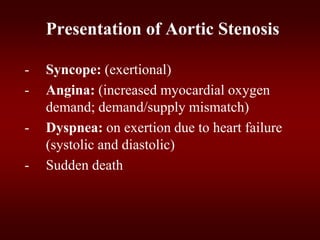
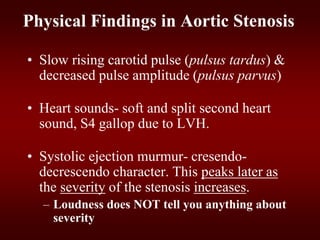
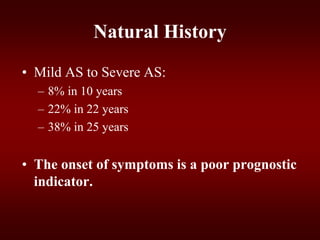
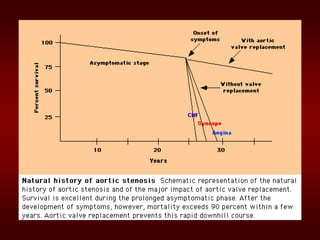
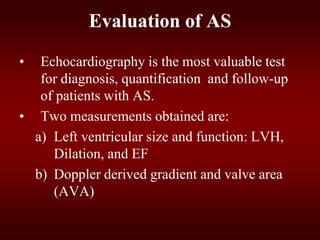
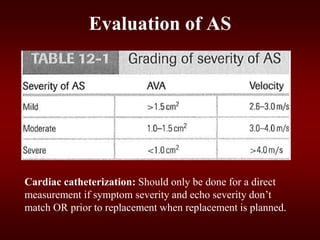
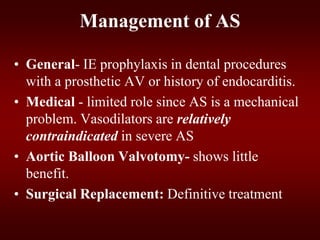
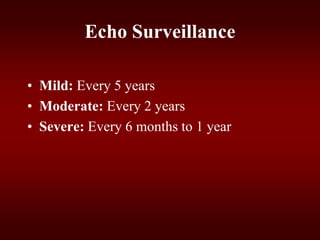
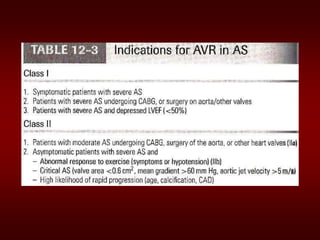
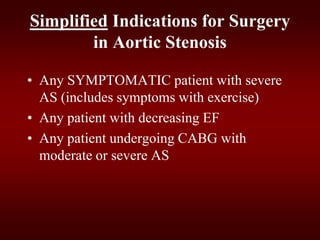
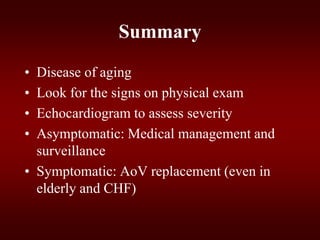
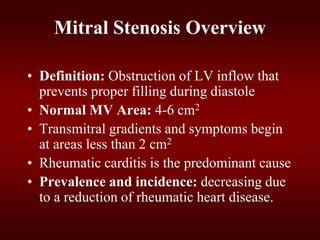
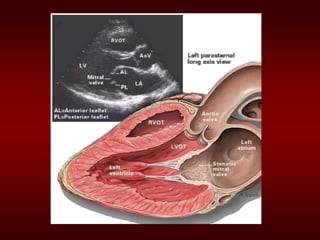
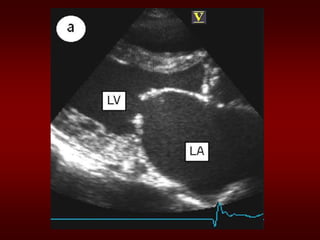
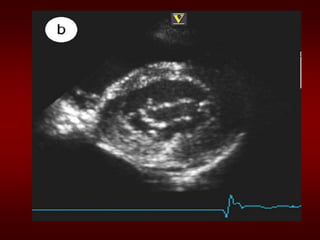
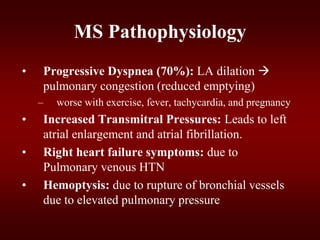
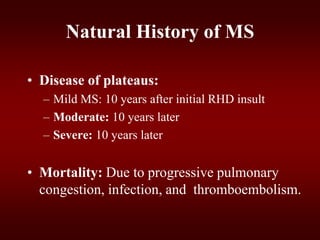
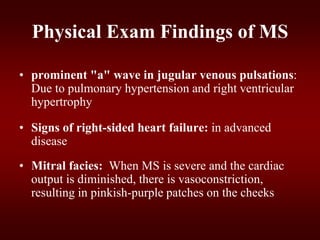
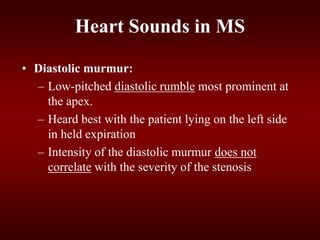
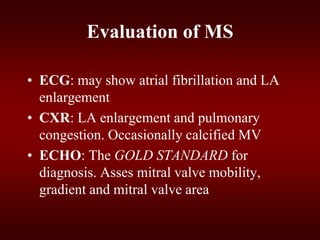
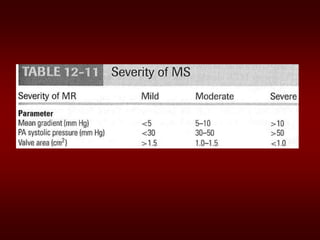
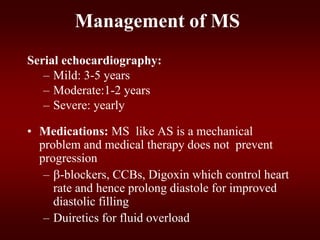
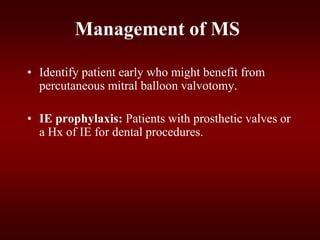
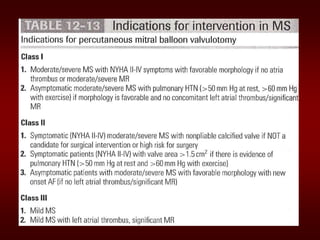
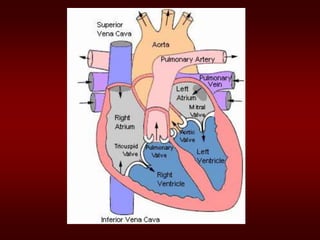
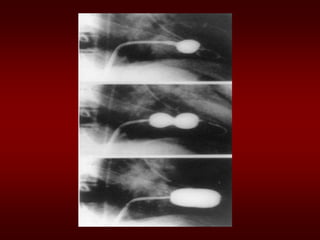
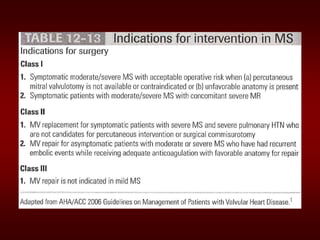
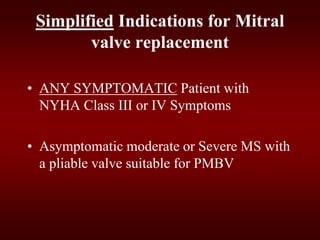
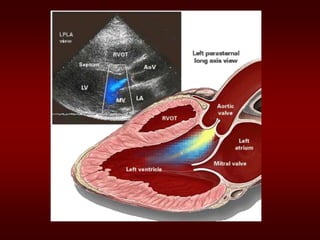
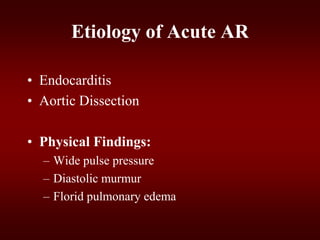
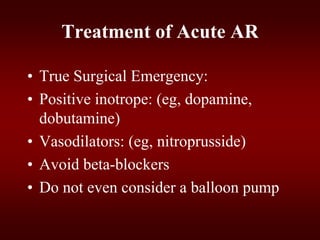
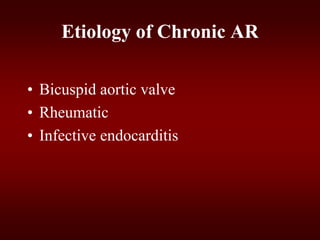
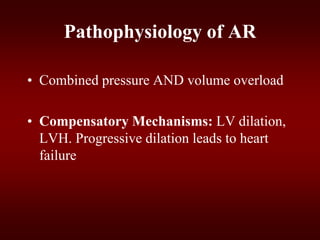
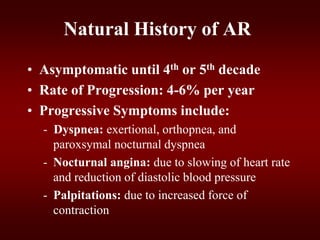
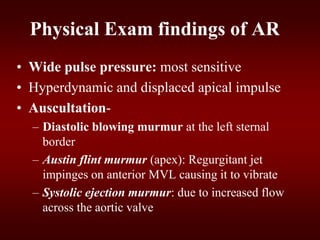
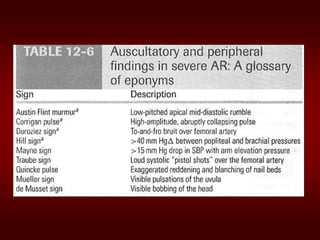
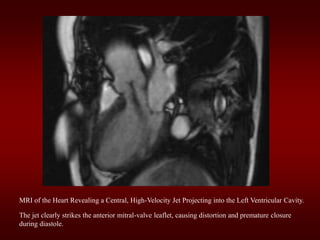
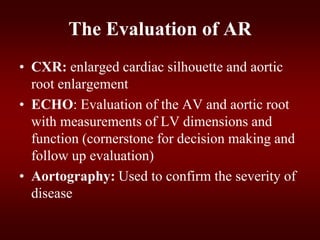
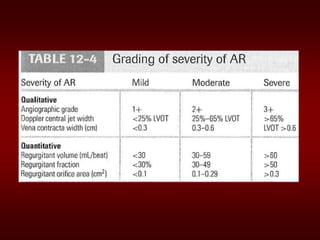
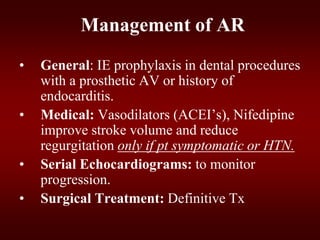
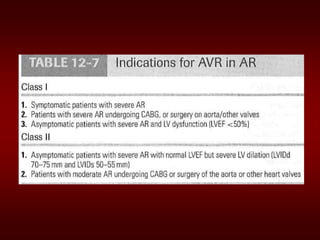
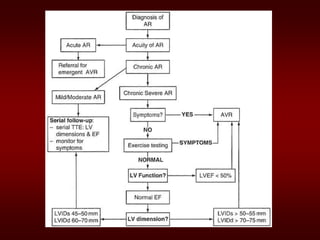
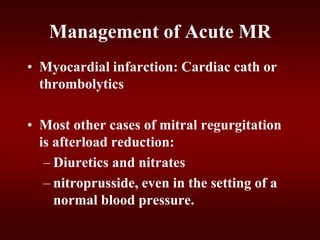
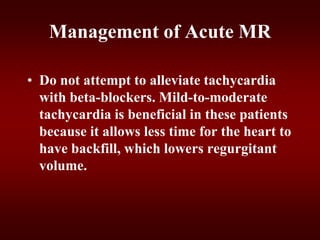
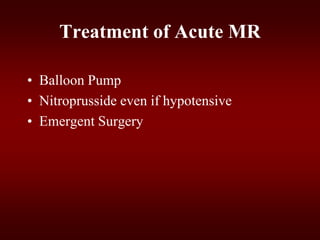
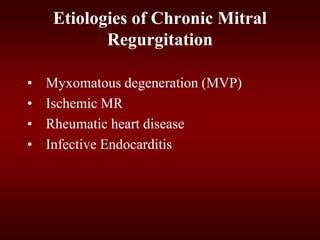
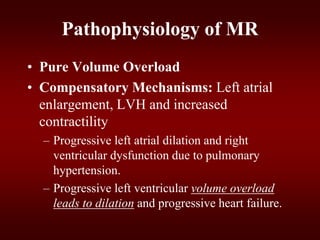
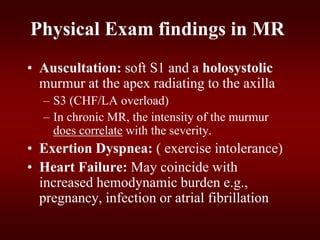
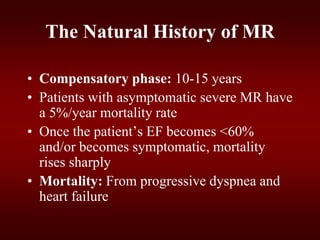
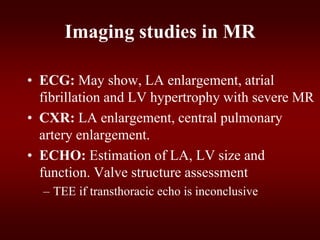
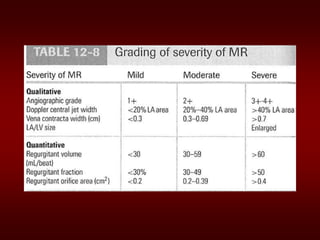
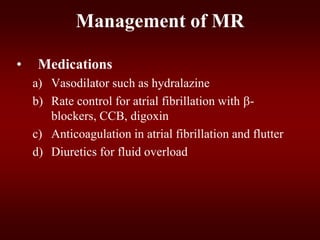
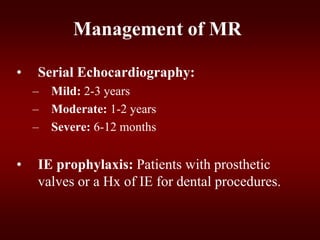
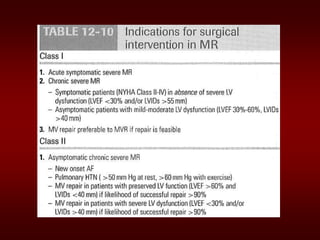
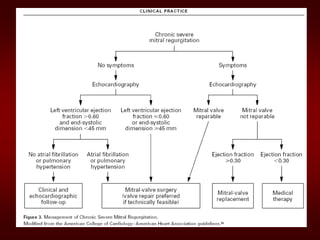
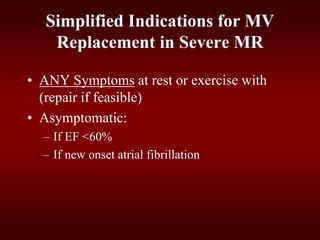
This document discusses valvular heart disease, focusing on aortic stenosis, mitral stenosis, aortic regurgitation, and mitral regurgitation. It covers the etiology, pathophysiology, presentation, evaluation, and management of each condition. For aortic and mitral stenosis, the goals are to recognize symptoms of severe disease and identify patients who need valve replacement. For regurgitant lesions, treatment focuses on supporting cardiac function medically until symptoms appear or structural deterioration occurs, then referring for surgical intervention. Echocardiography plays a key role in diagnosing severity and monitoring progression.