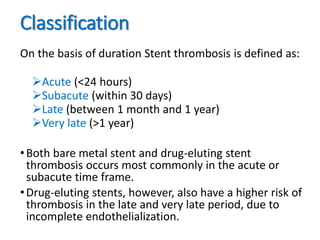
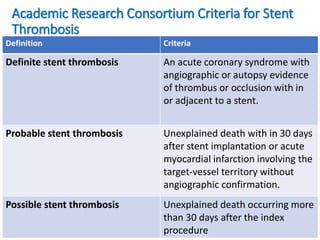
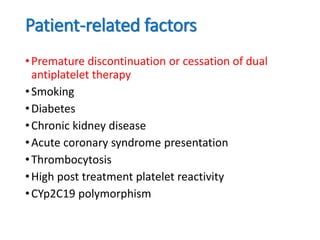
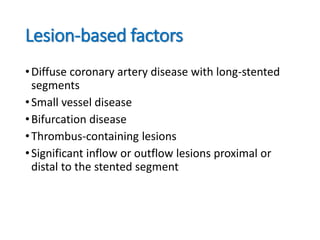
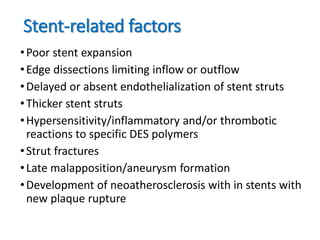
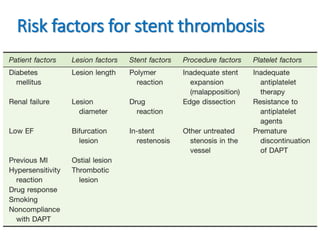
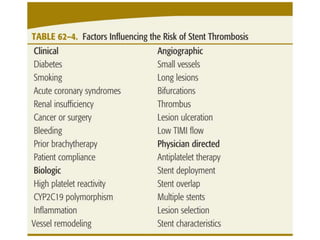
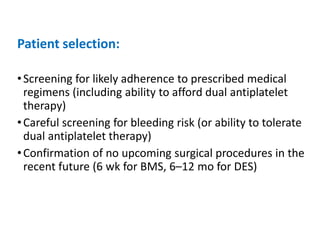
Stent thrombosis is a rare but serious complication of percutaneous coronary intervention (PCI) with mortality rates between 25-40%. It is classified based on timing (acute, subacute, late, very late) and etiology (primary, secondary). Risk factors include premature discontinuation of dual antiplatelet therapy, smoking, diabetes, chronic kidney disease, acute coronary syndrome, and high platelet reactivity. Strategies to minimize stent thrombosis involve careful patient selection, optimal stent deployment, adherence to potent dual antiplatelet regimens, and treatment involving emergent thrombectomy with escalated antiplatelet therapy.