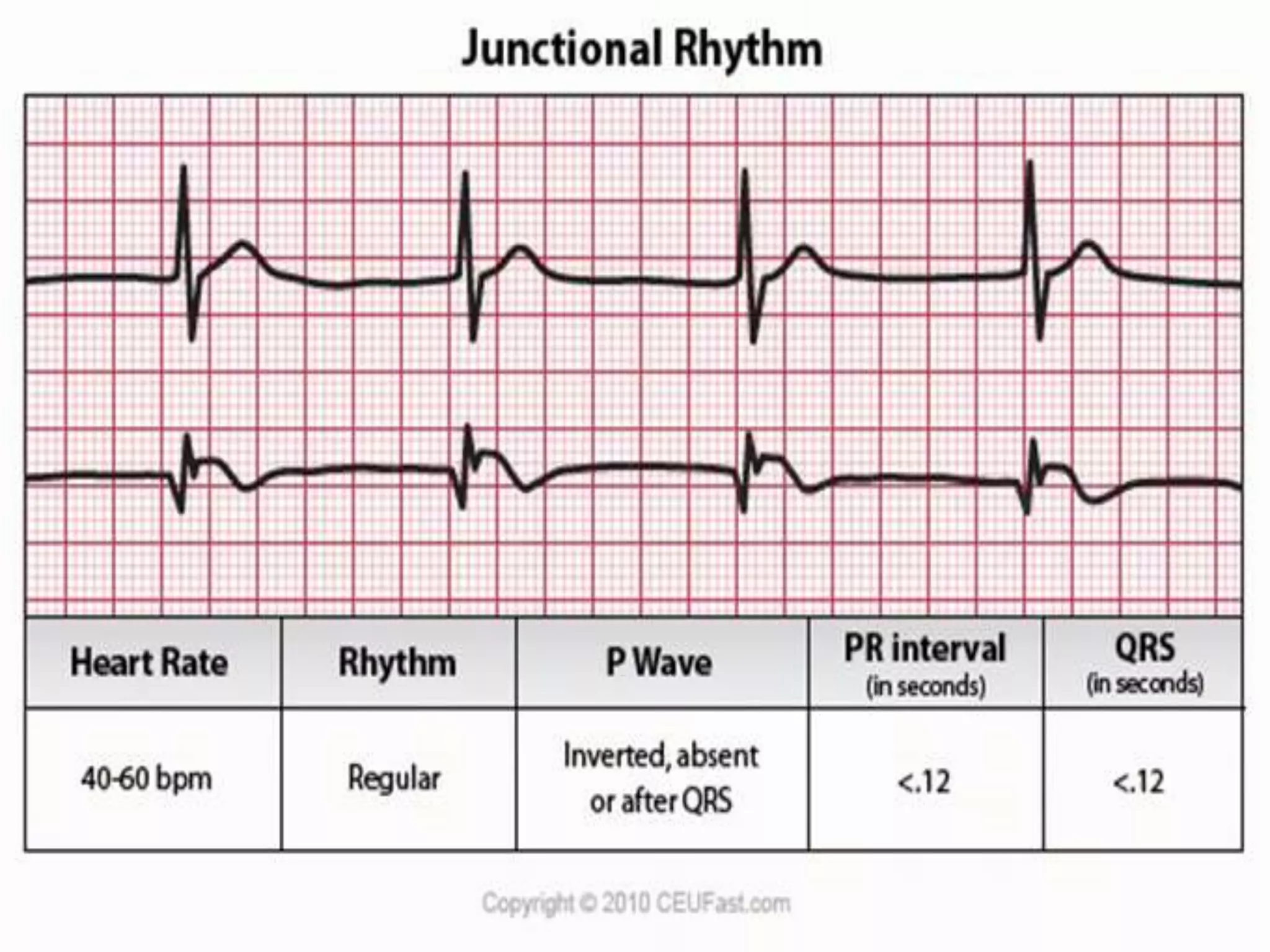
This document provides information on various cardiac dysrhythmias, including their causes, types, and management. It discusses junctional rhythms arising from the AV junction and their two major types - disturbances in automaticity and disturbances in conduction. Various types of AV blocks are described including first, second (Mobitz I and II), and third degree heart block. Other arrhythmias covered include bundle branch blocks, ventricular arrhythmias, pre-excitation syndromes like Wolf-Parkinson-White syndrome, and sudden cardiac death. The management of dysrhythmias through pharmacotherapy, defibrillation, ablation, and pacemakers is also summarized.