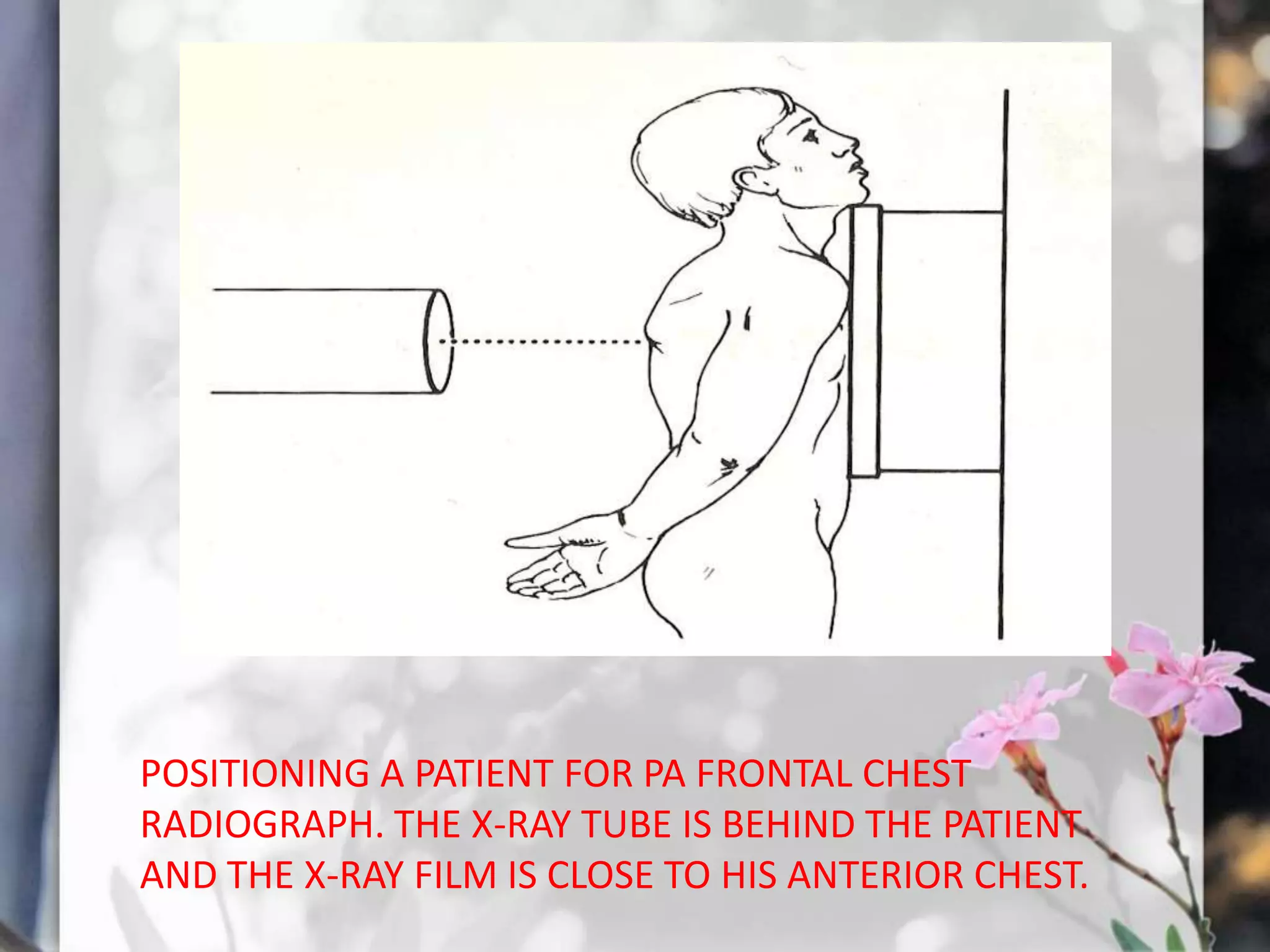
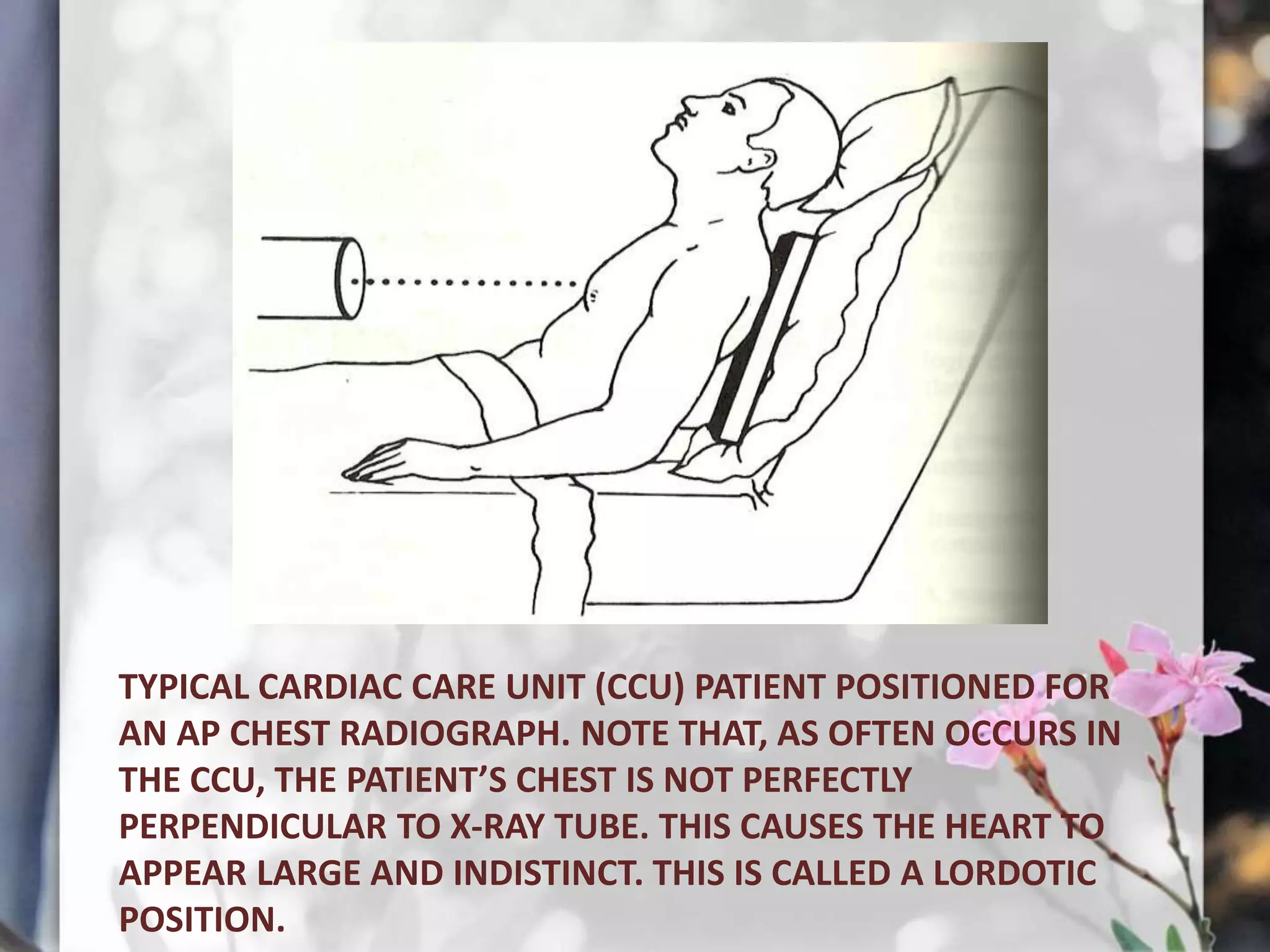
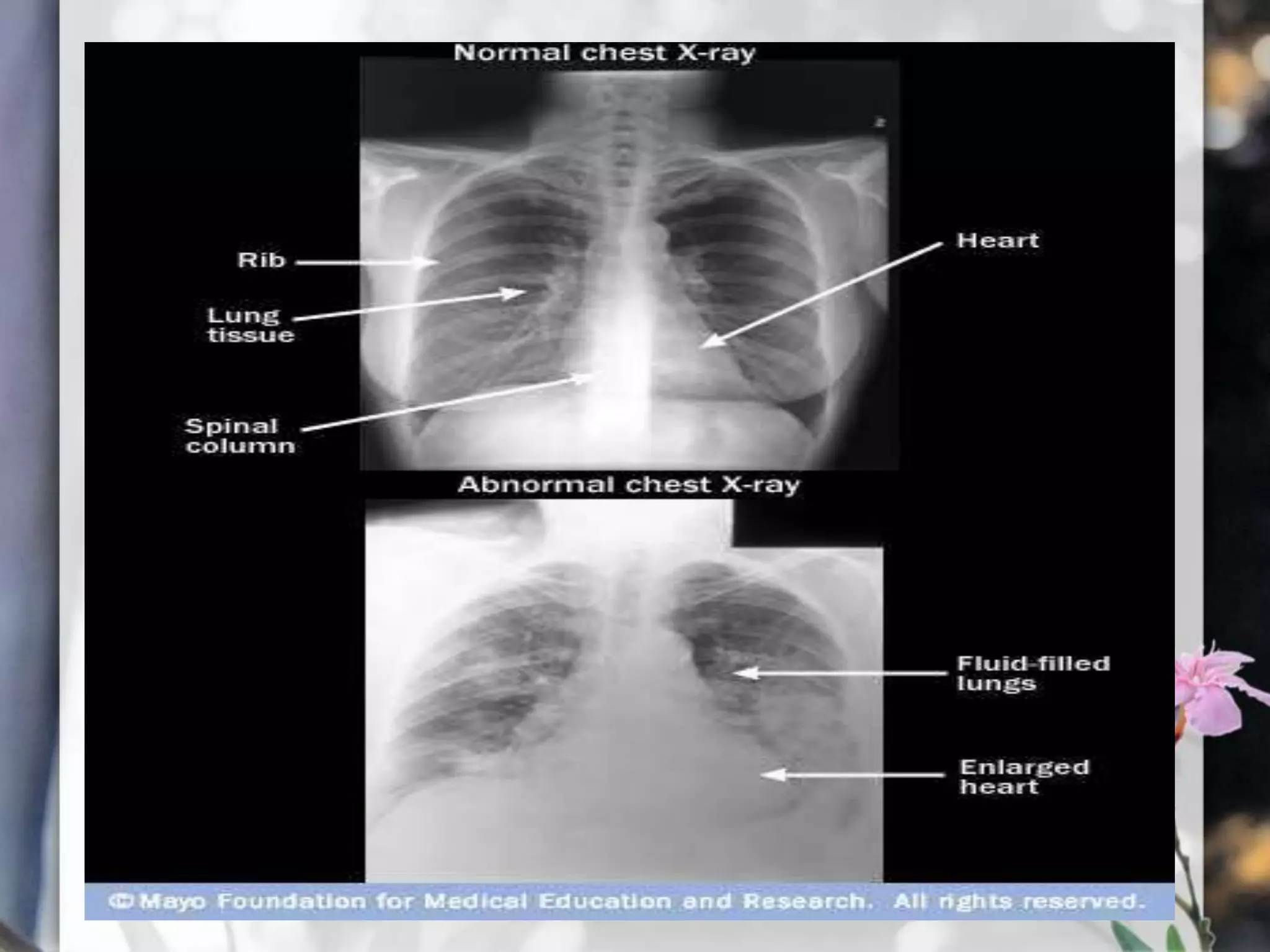
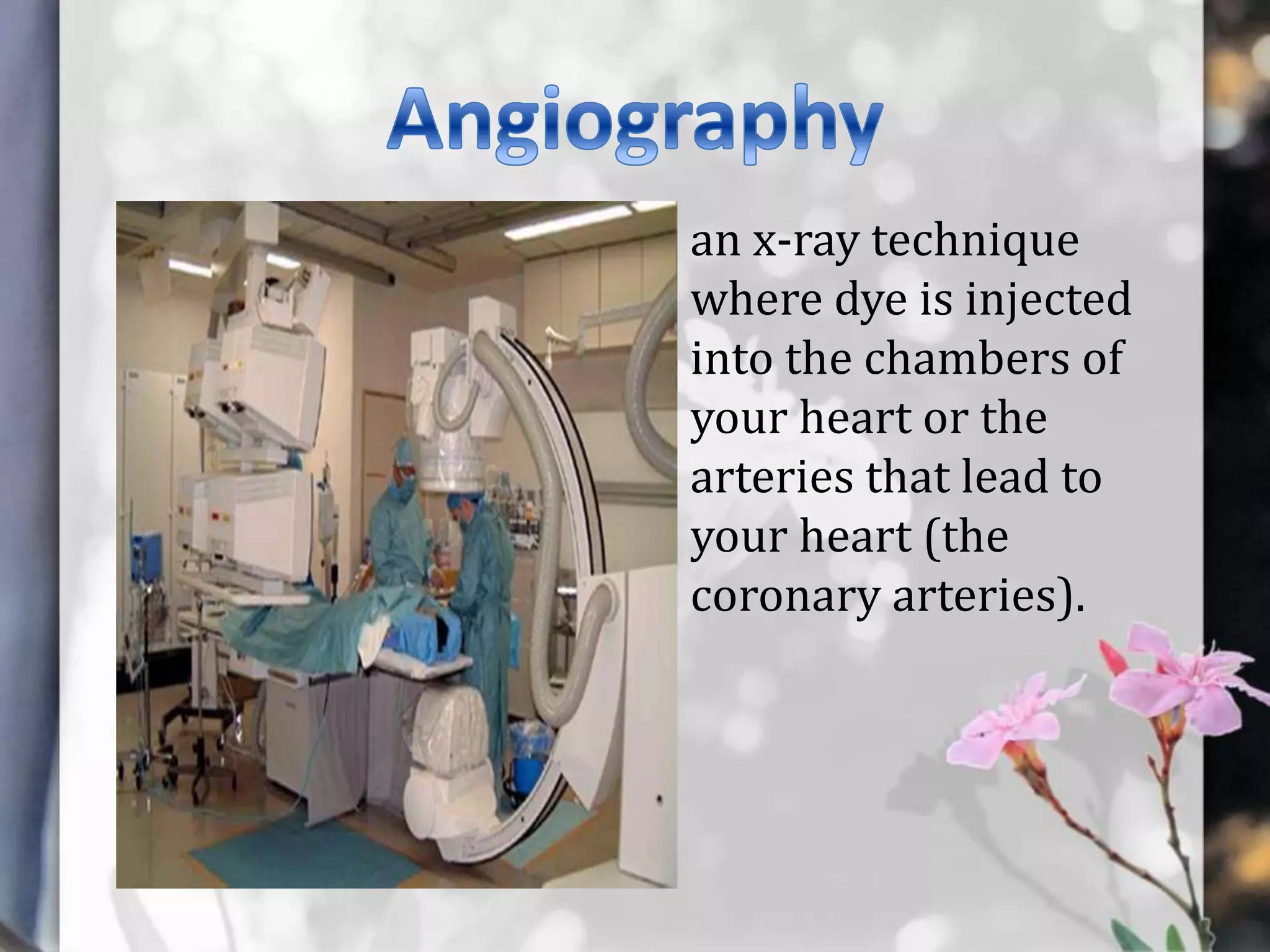
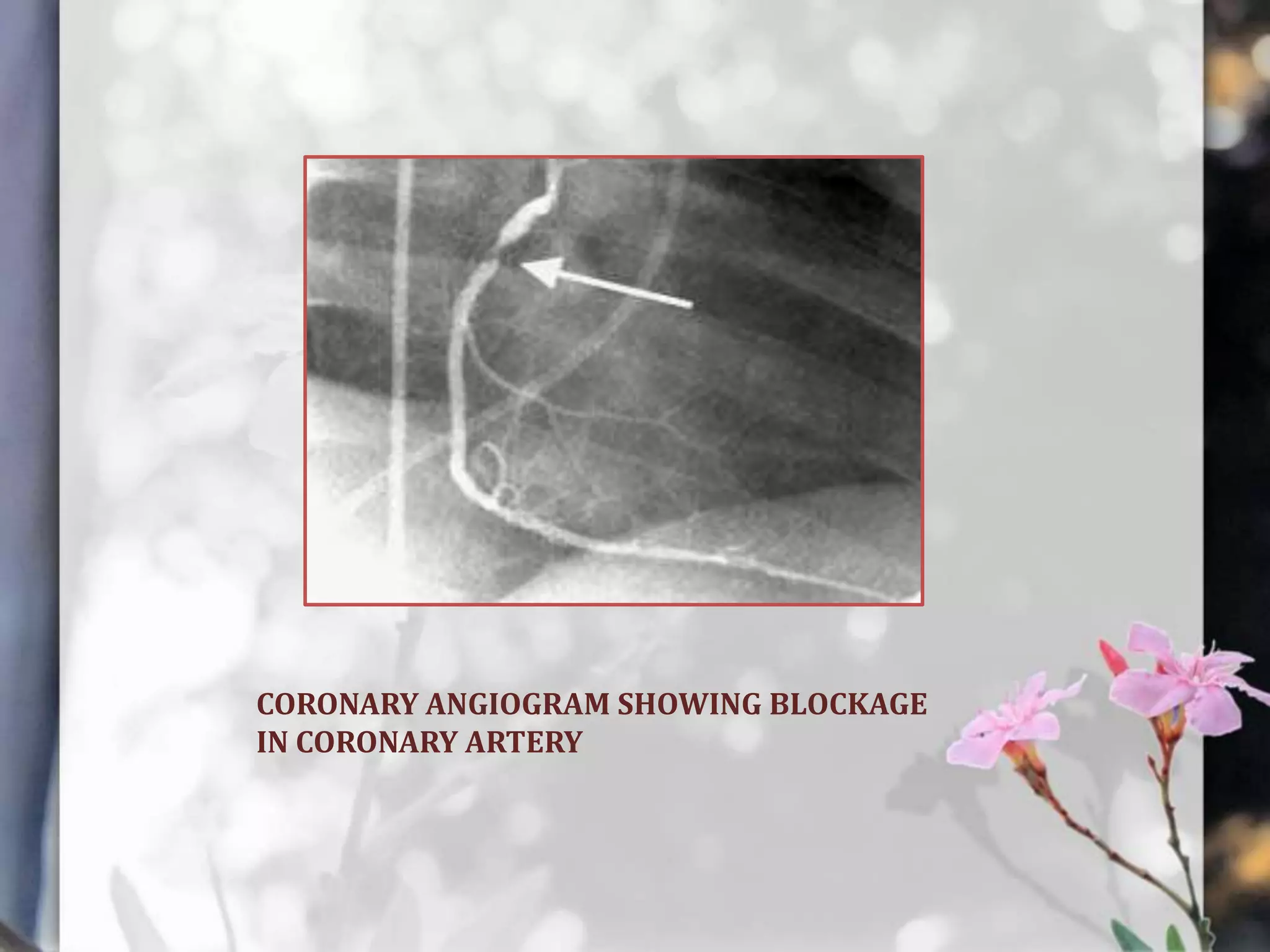
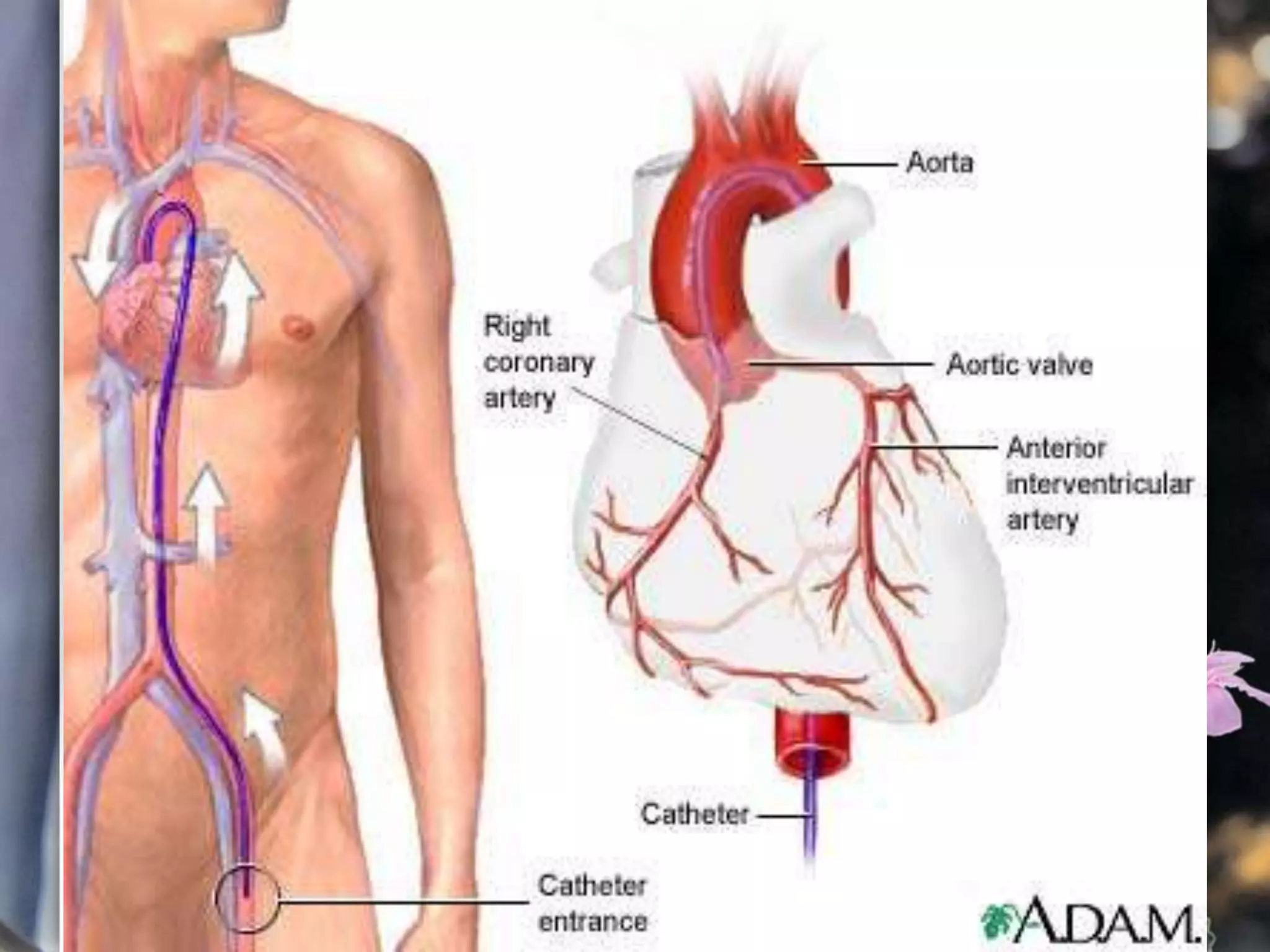
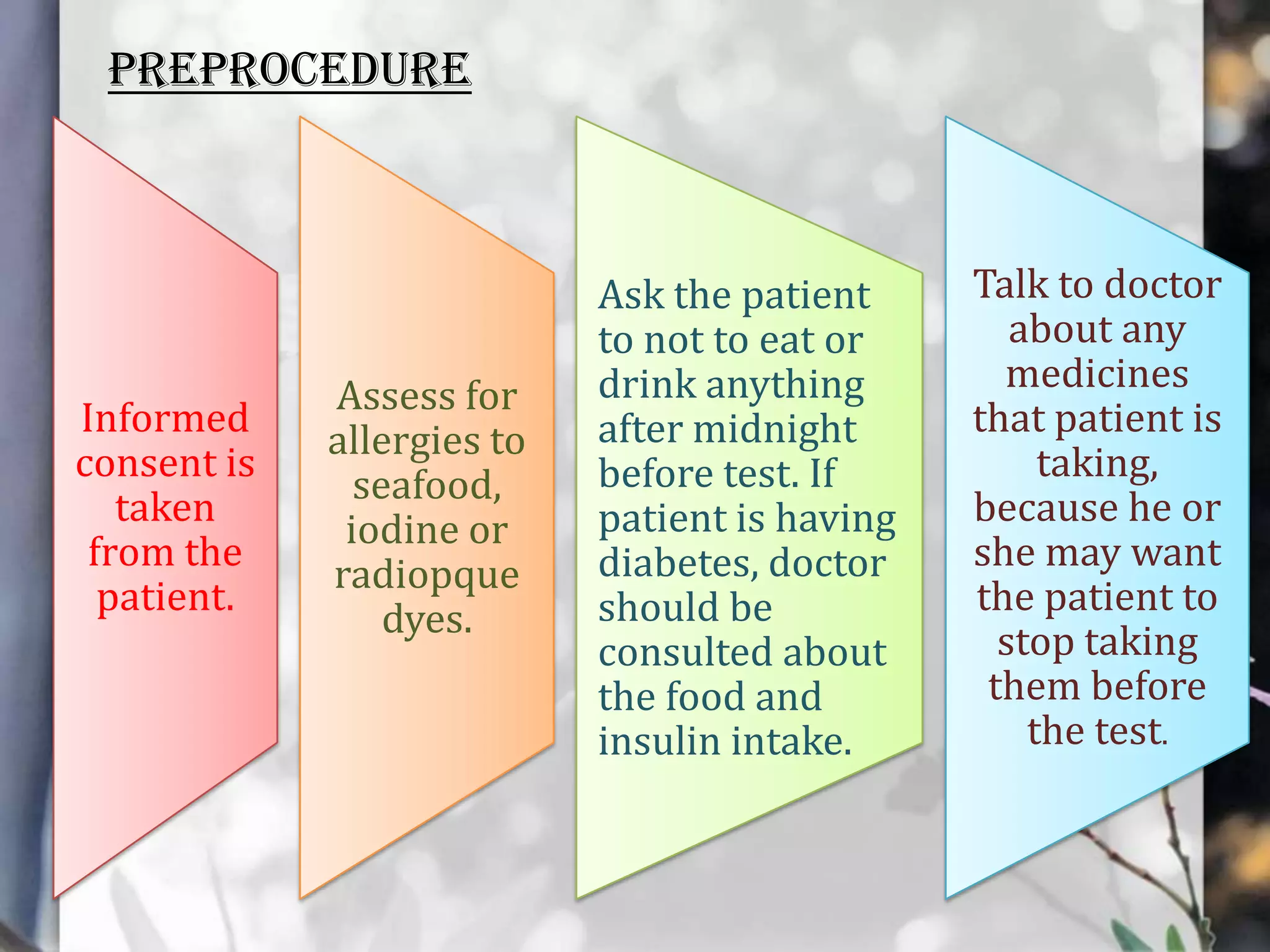
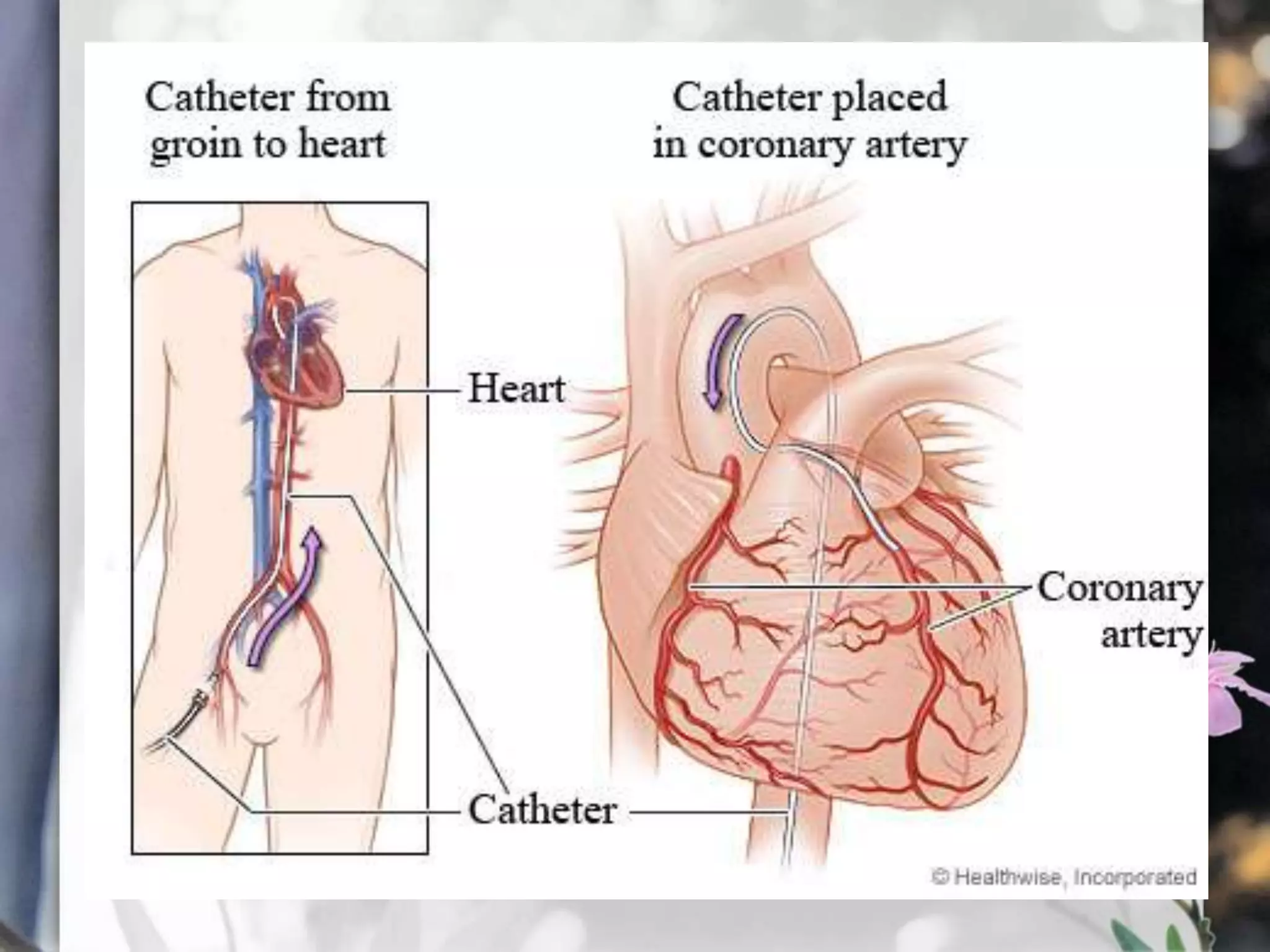
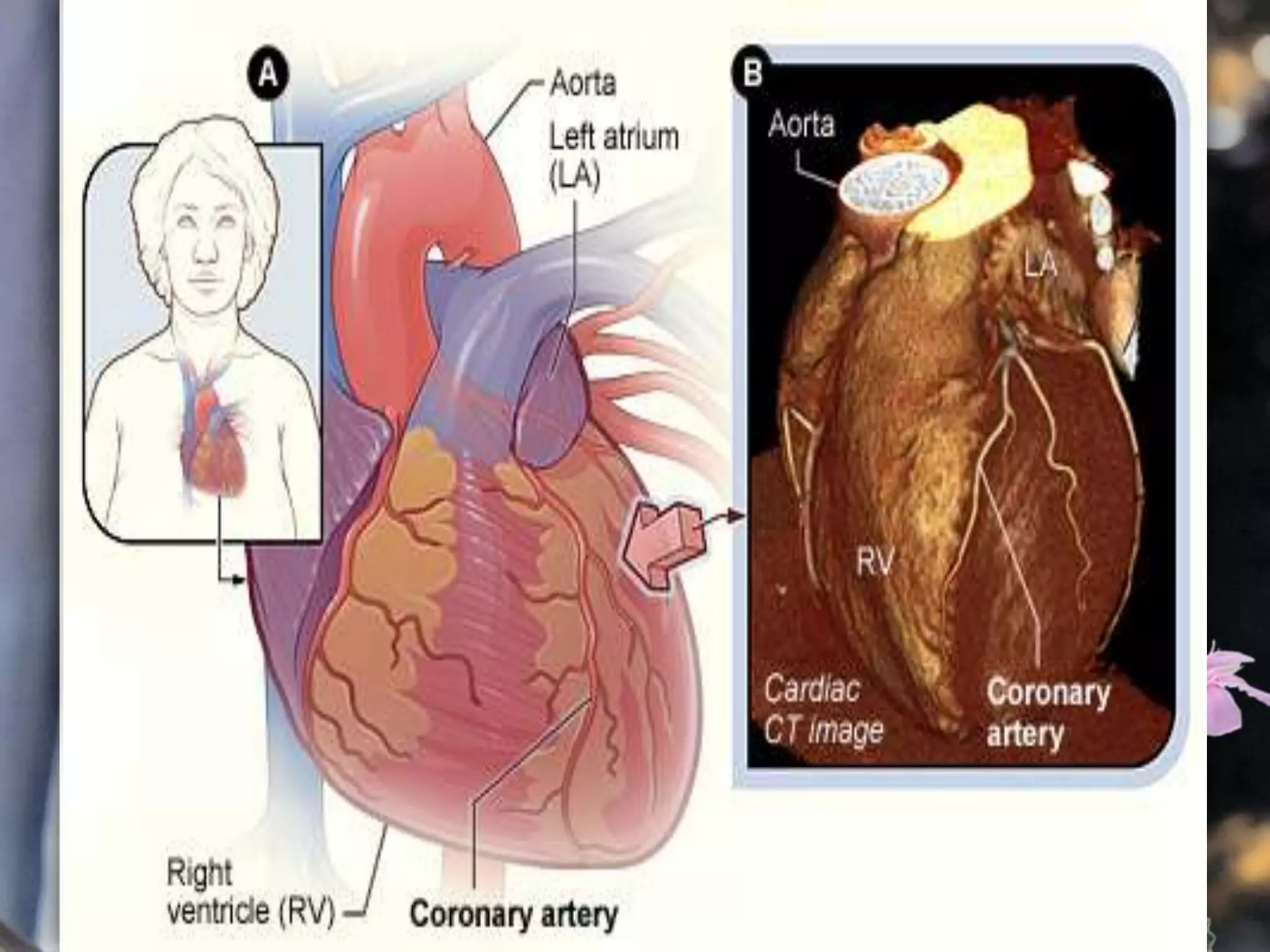
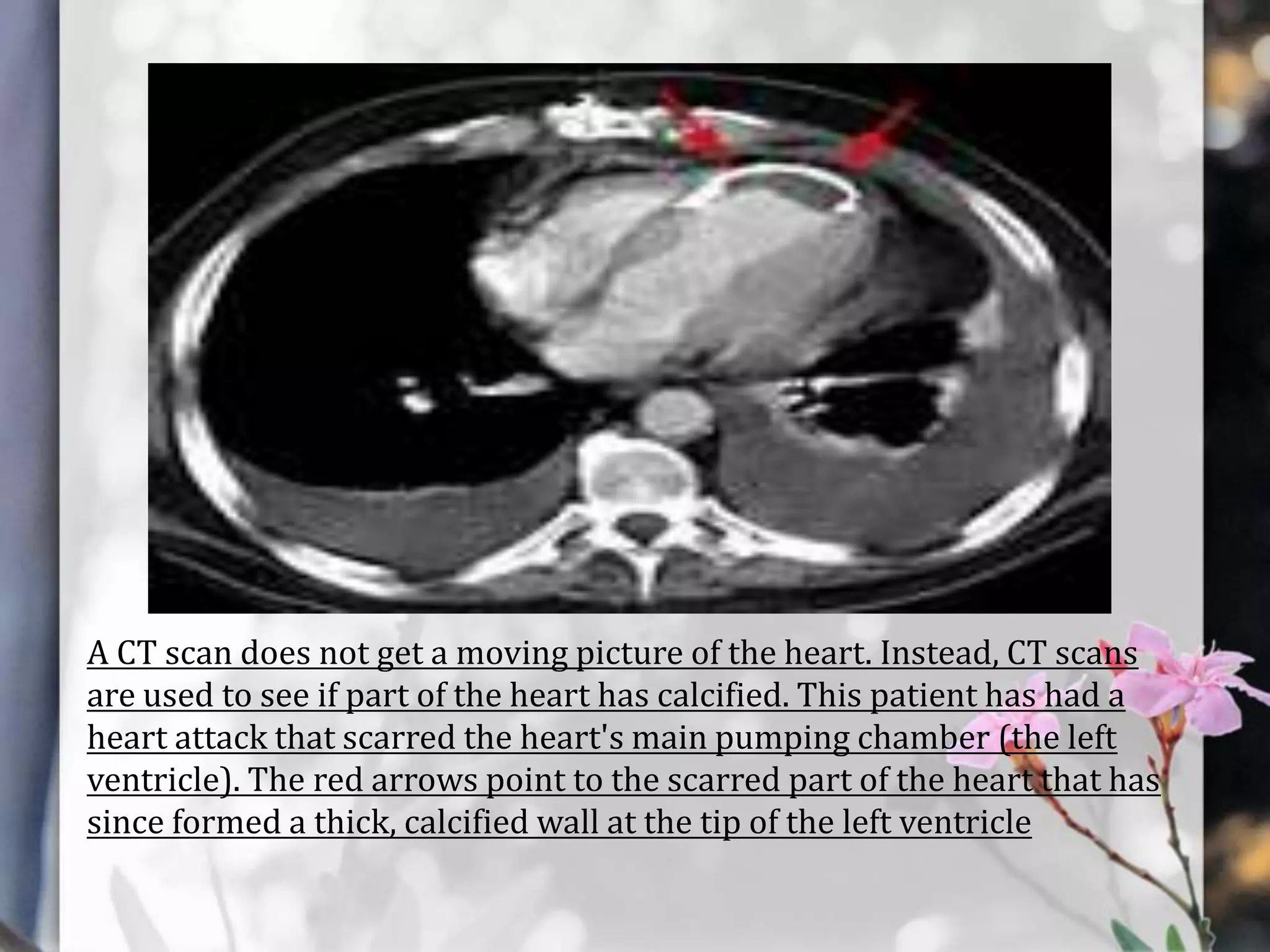
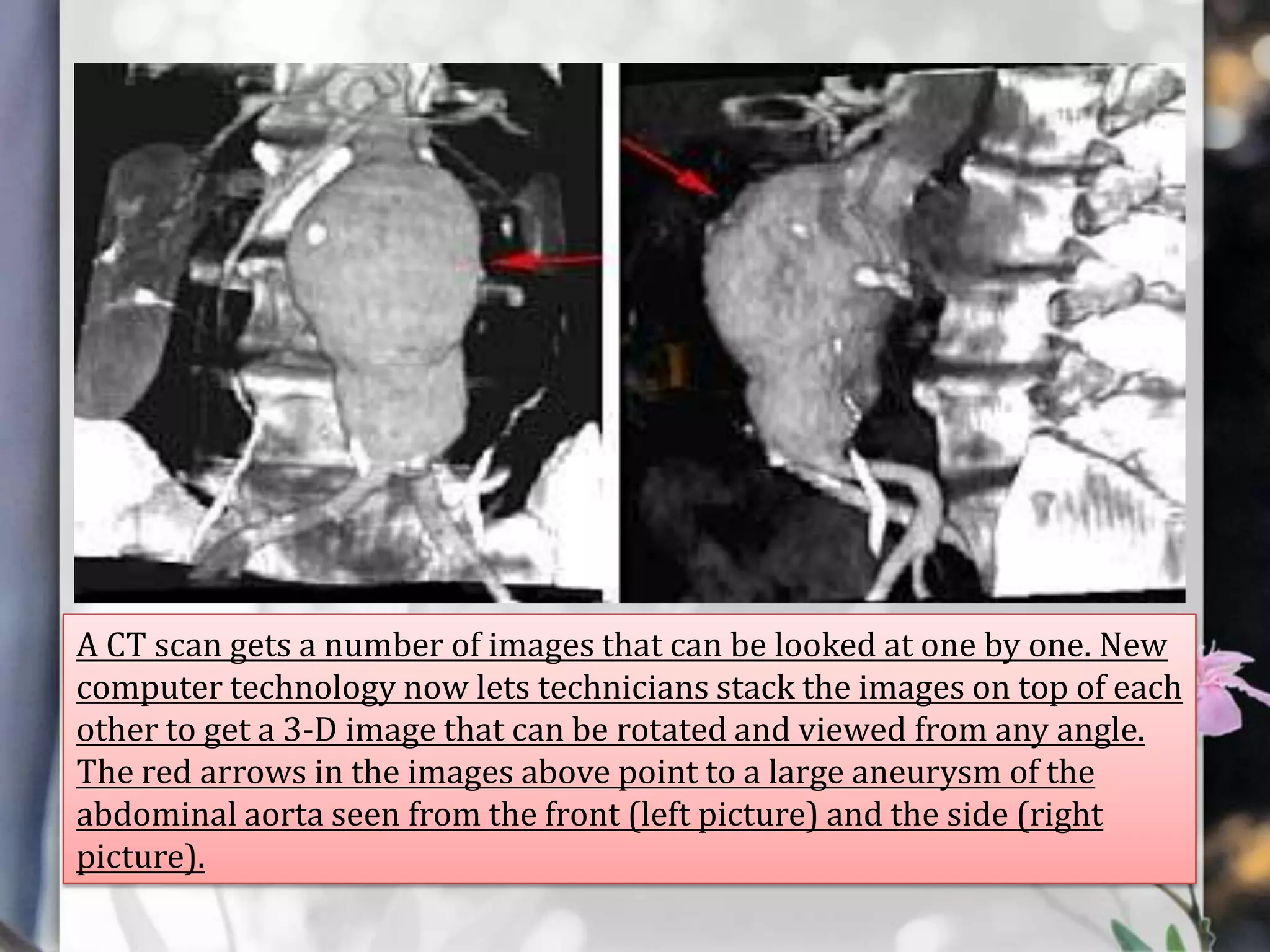
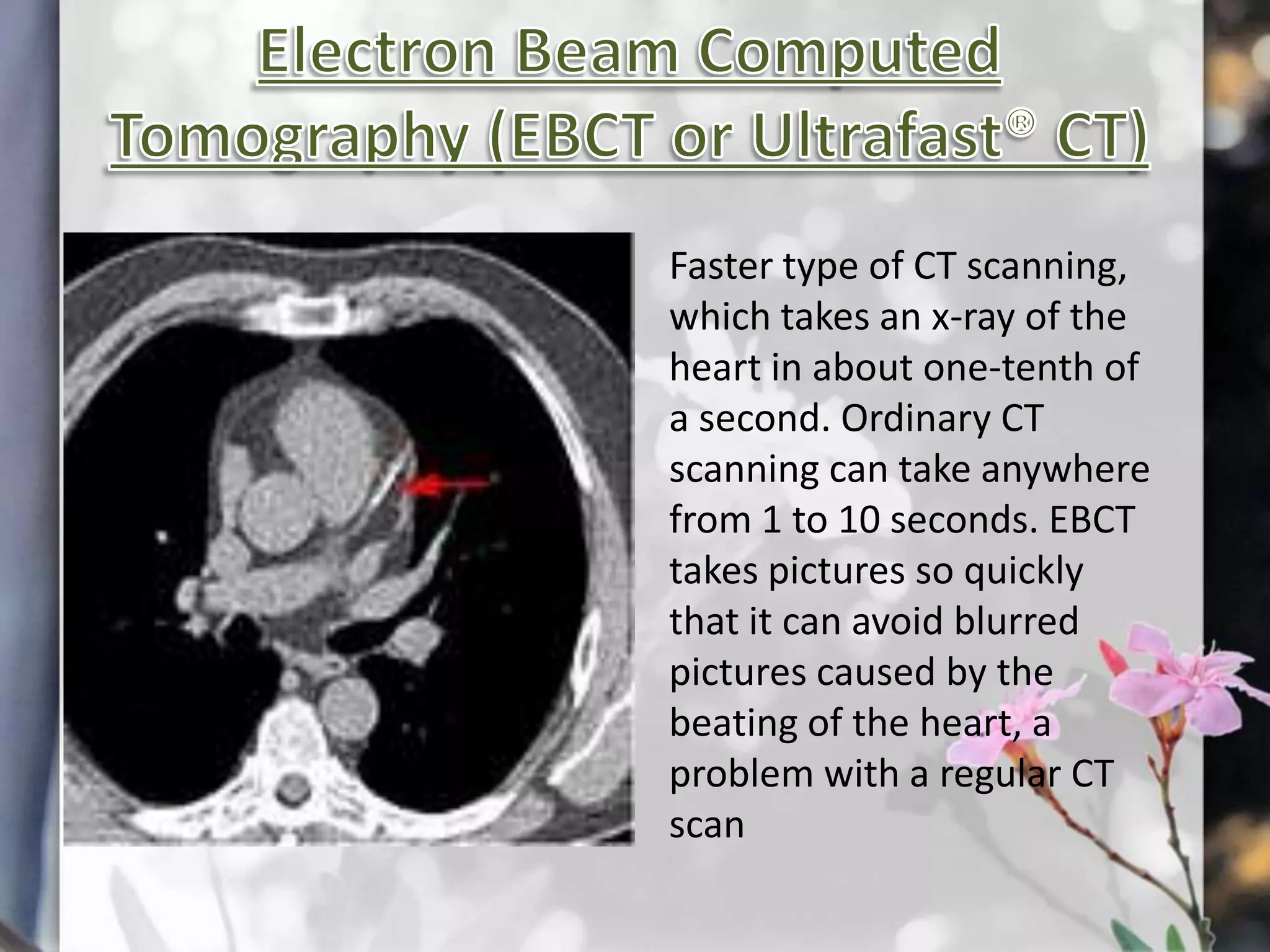
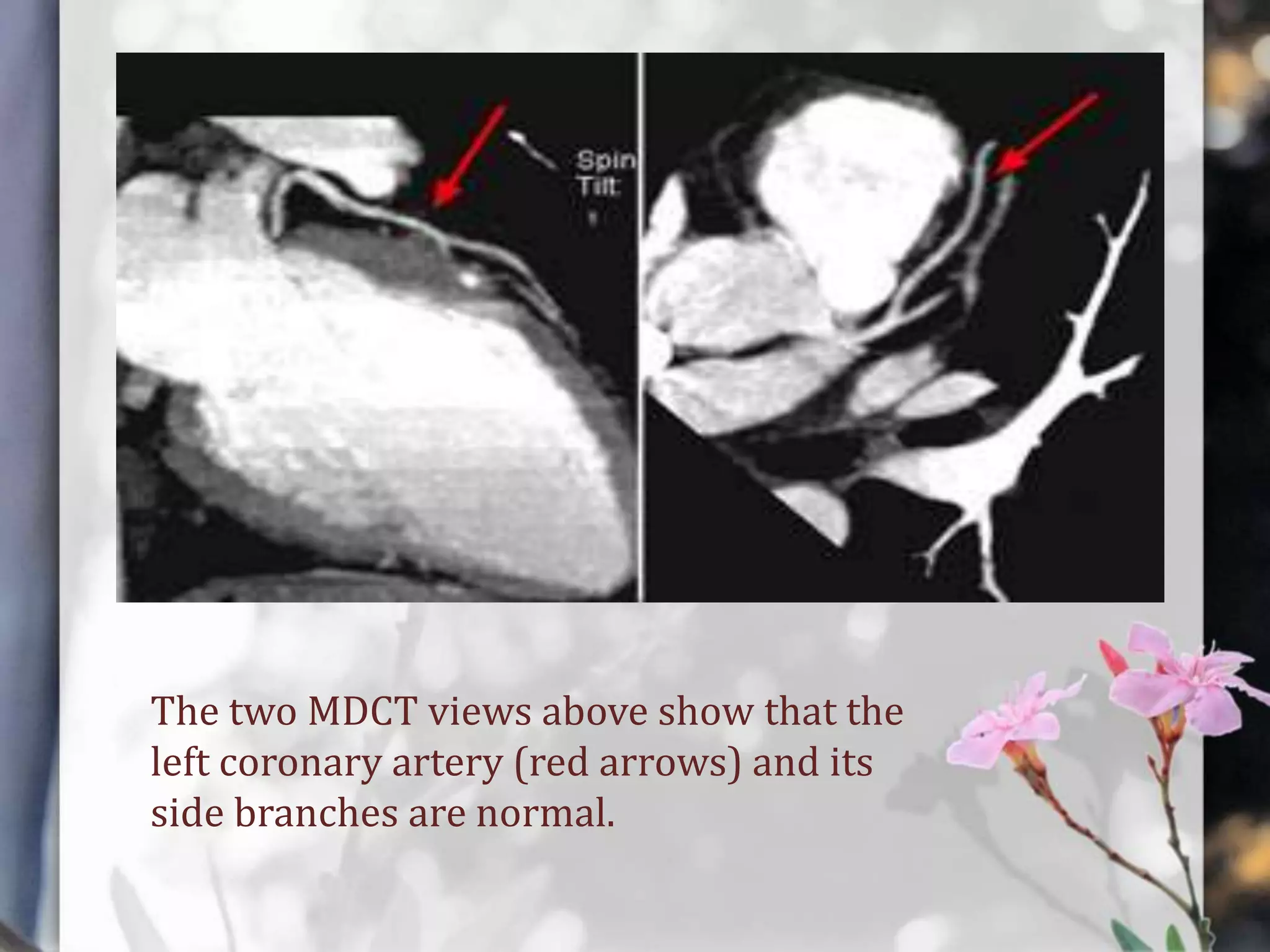
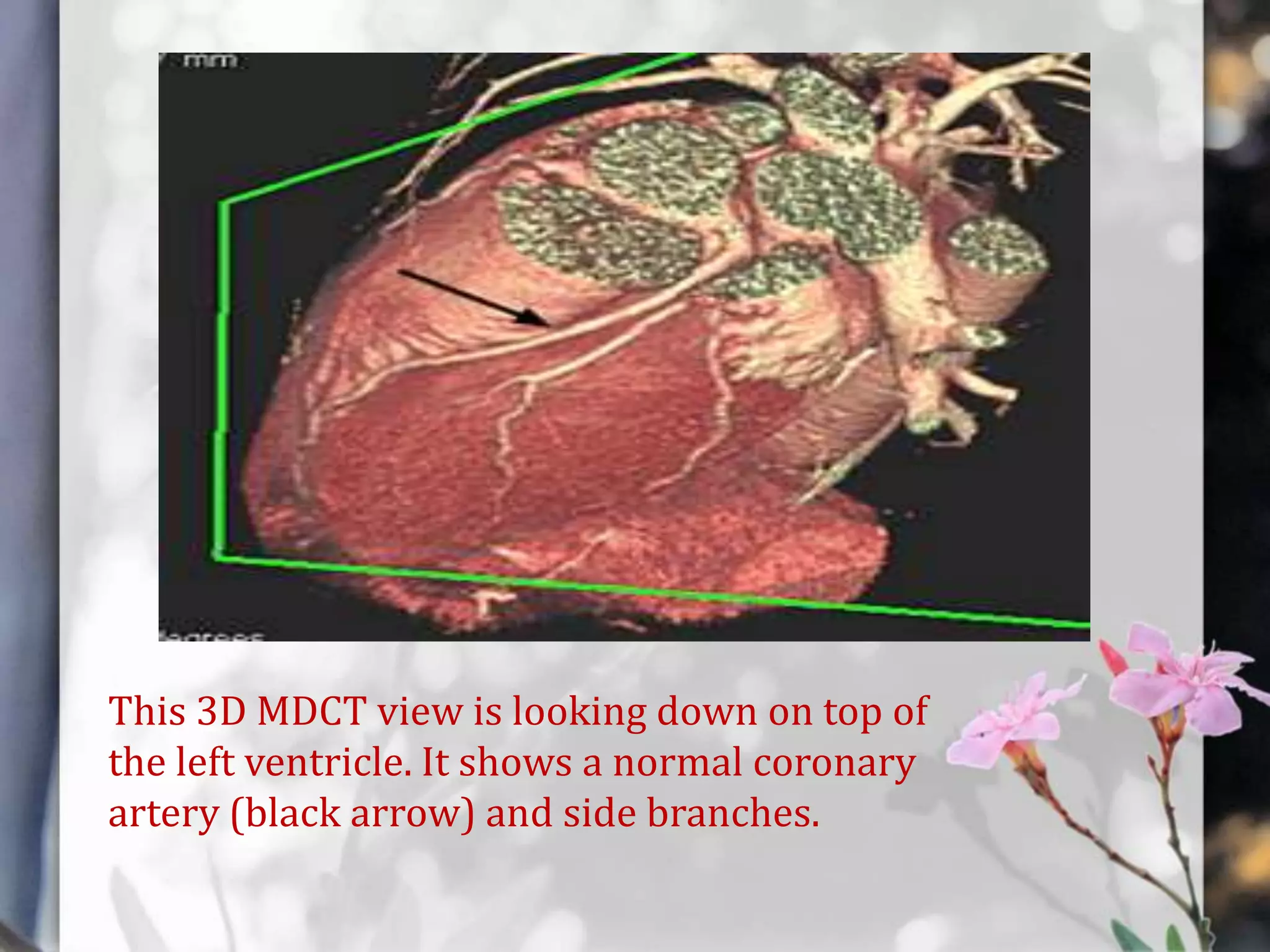
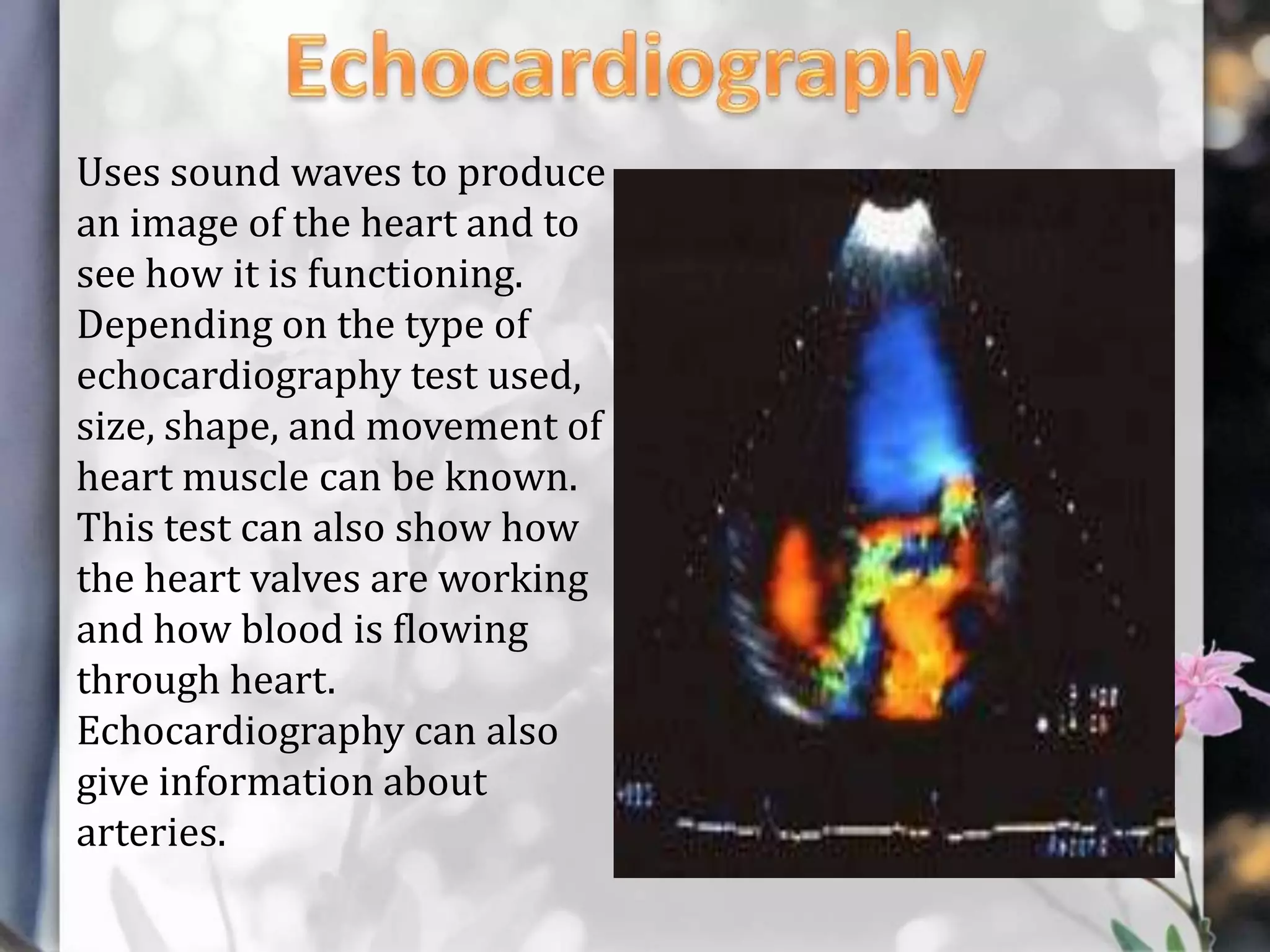
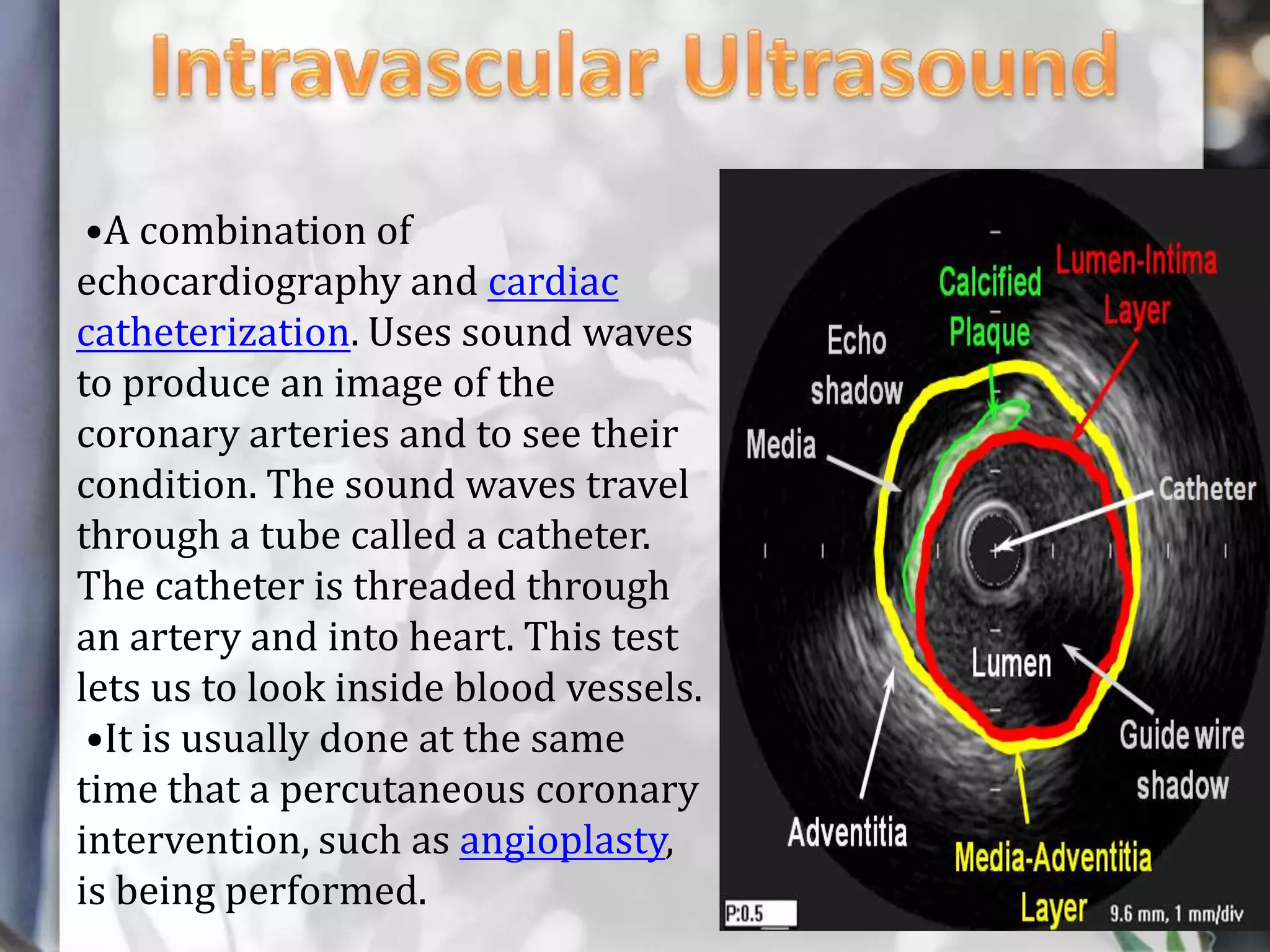
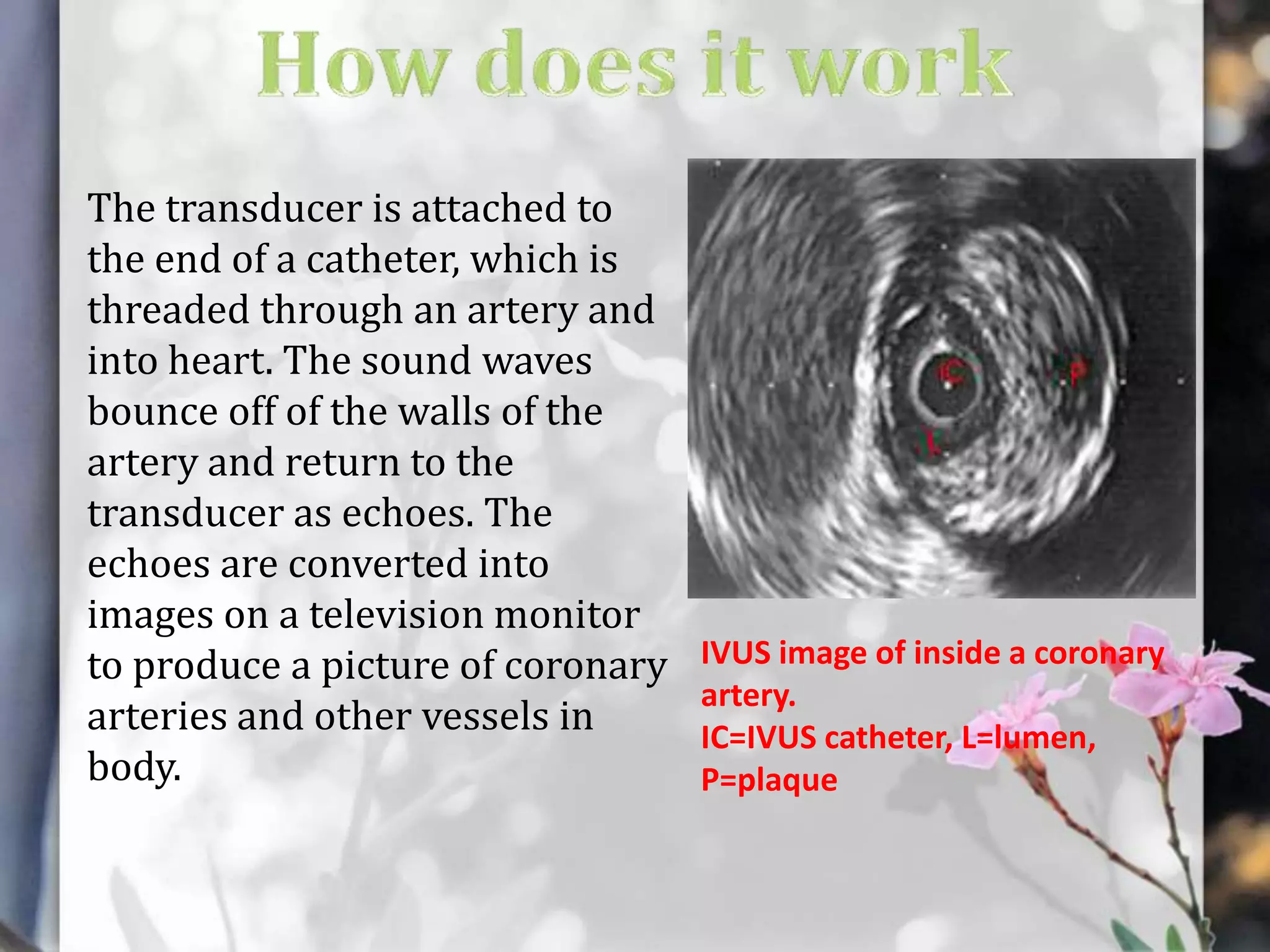
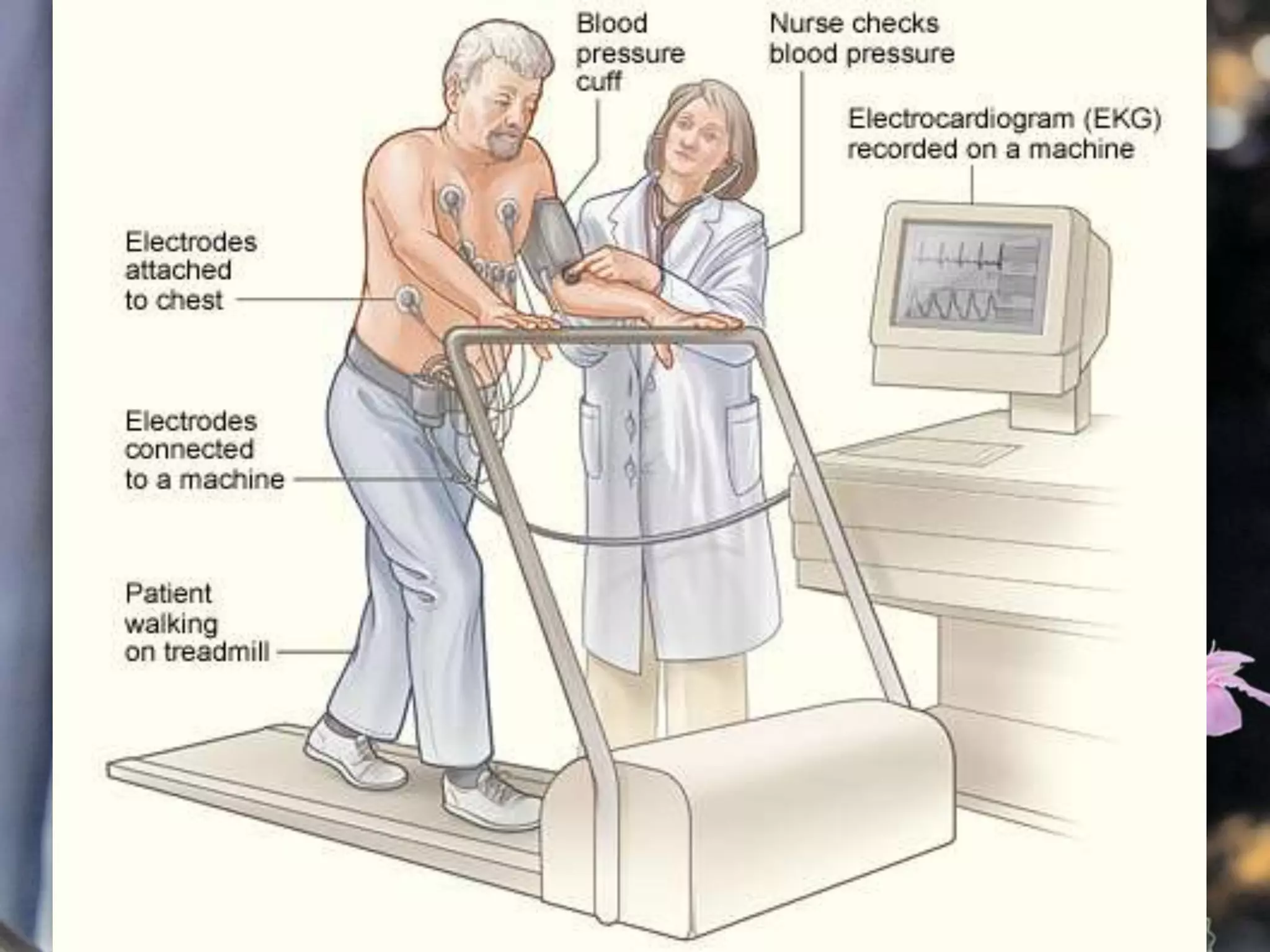
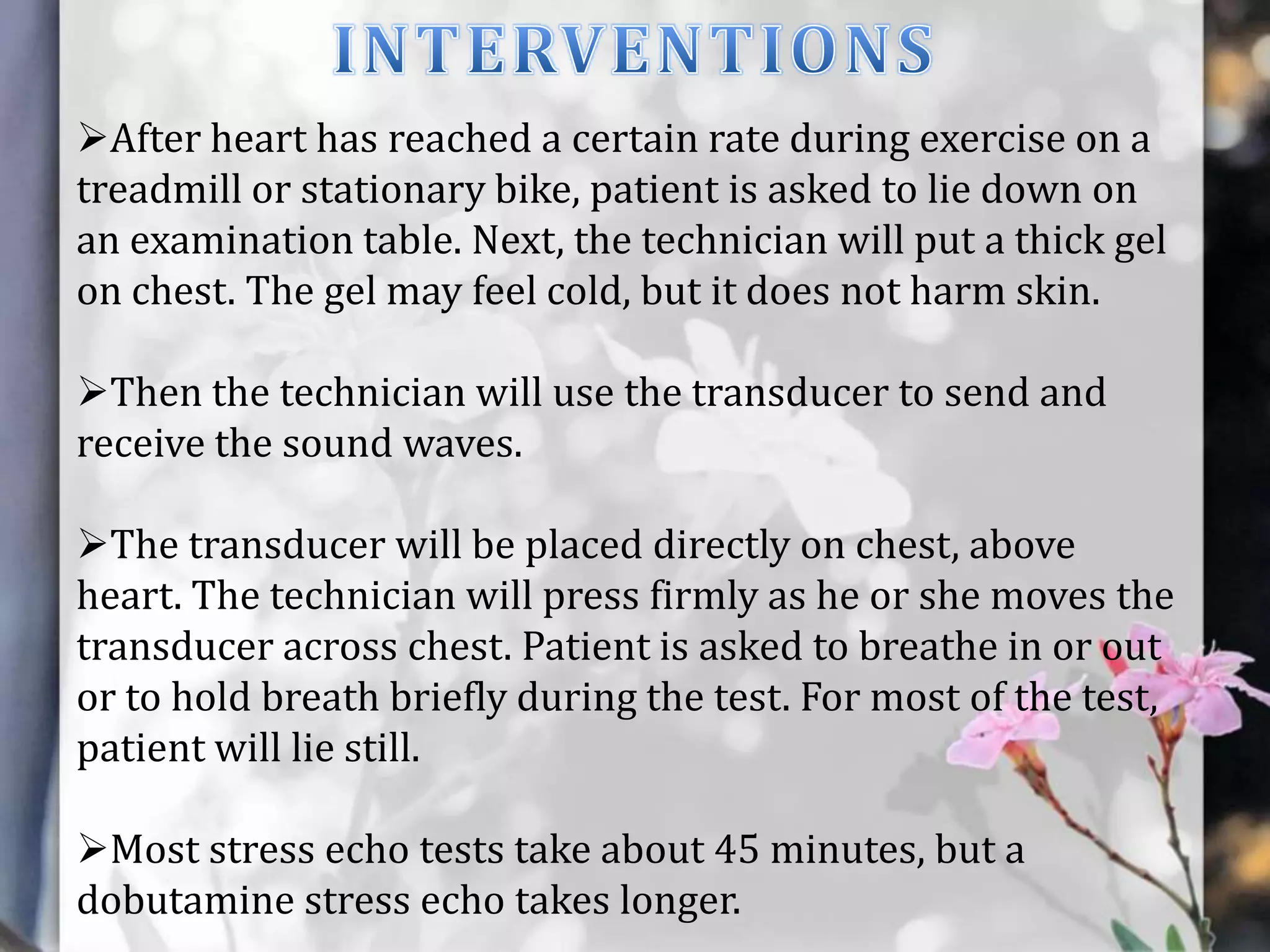
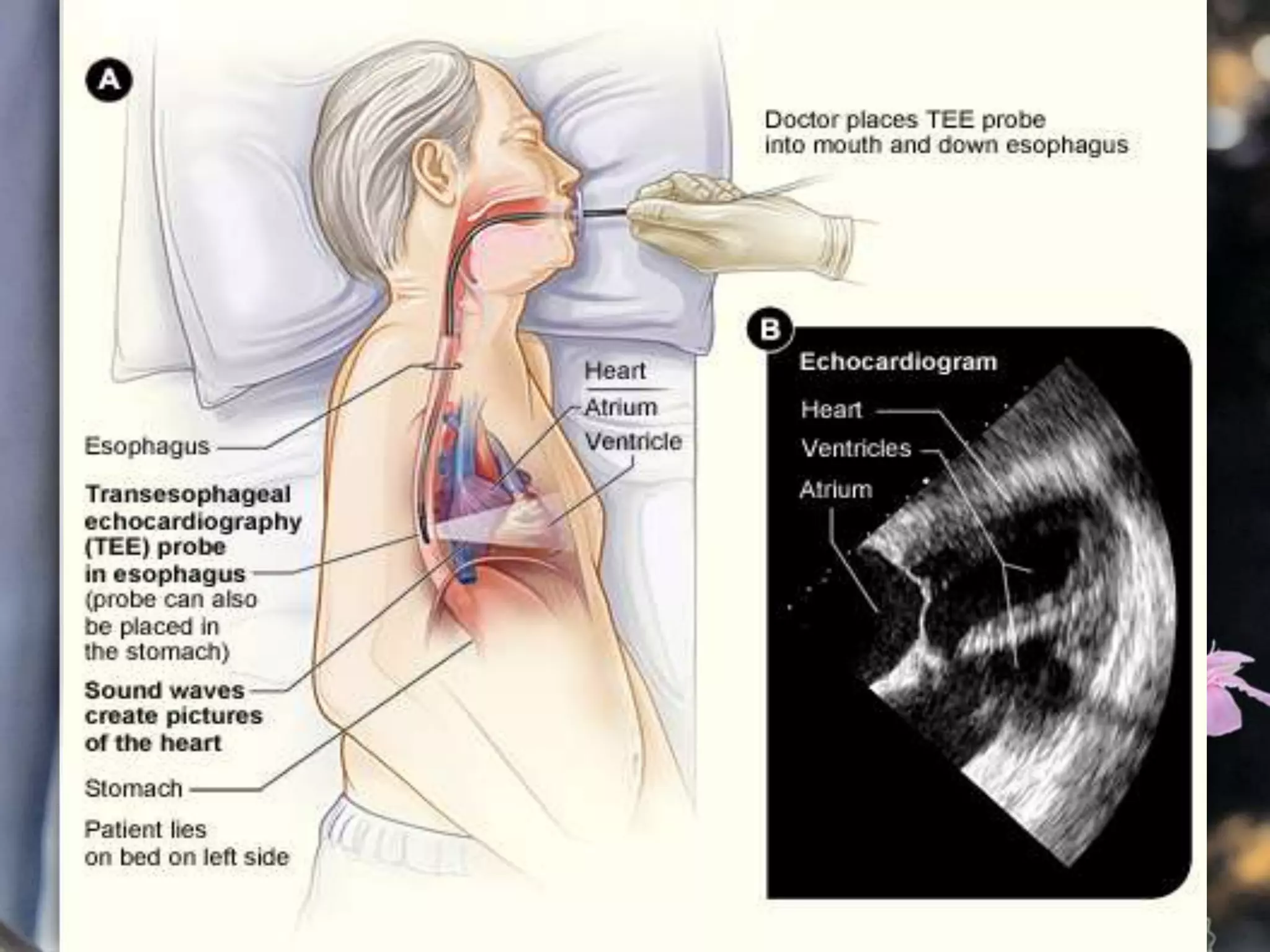
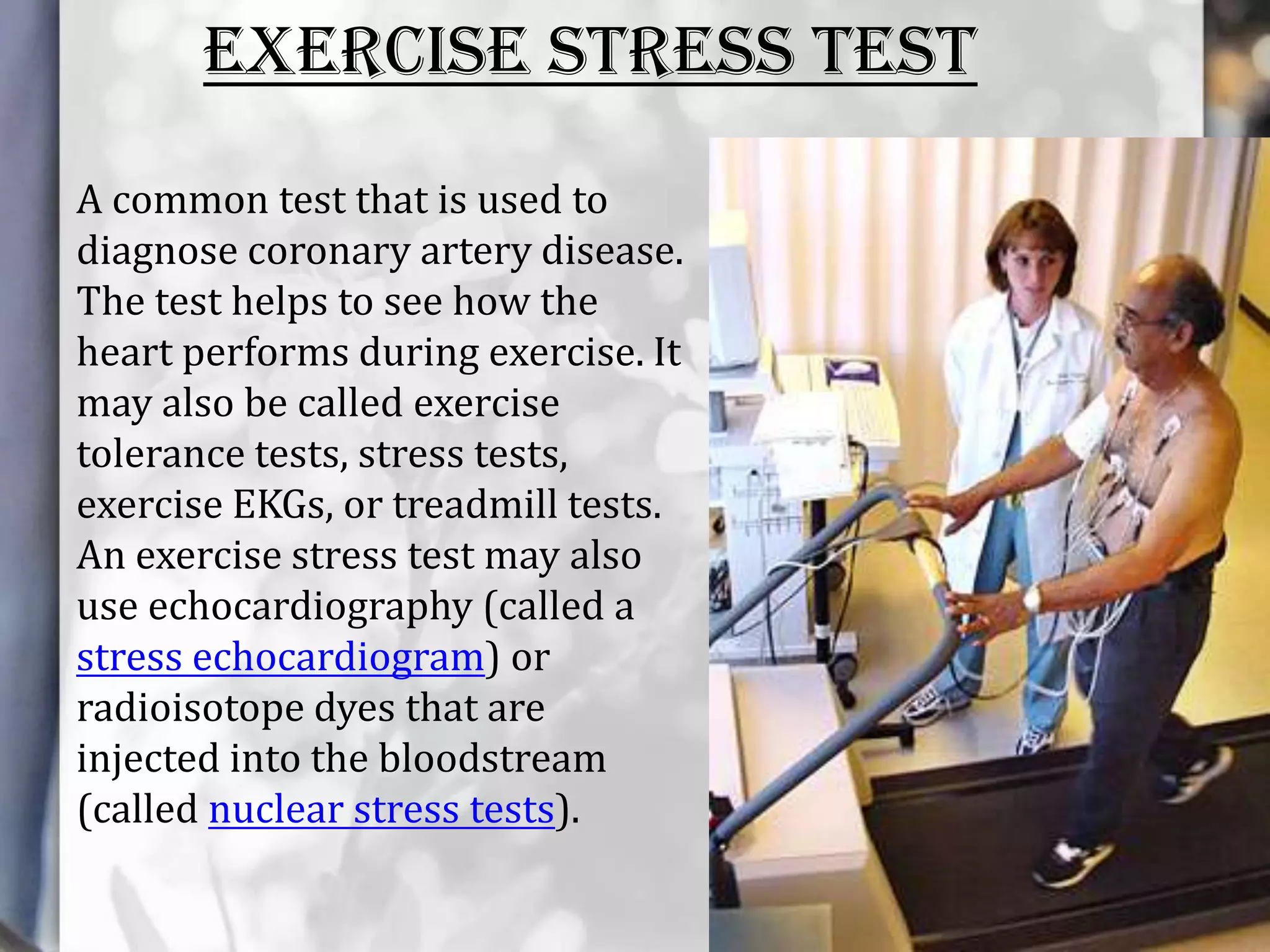
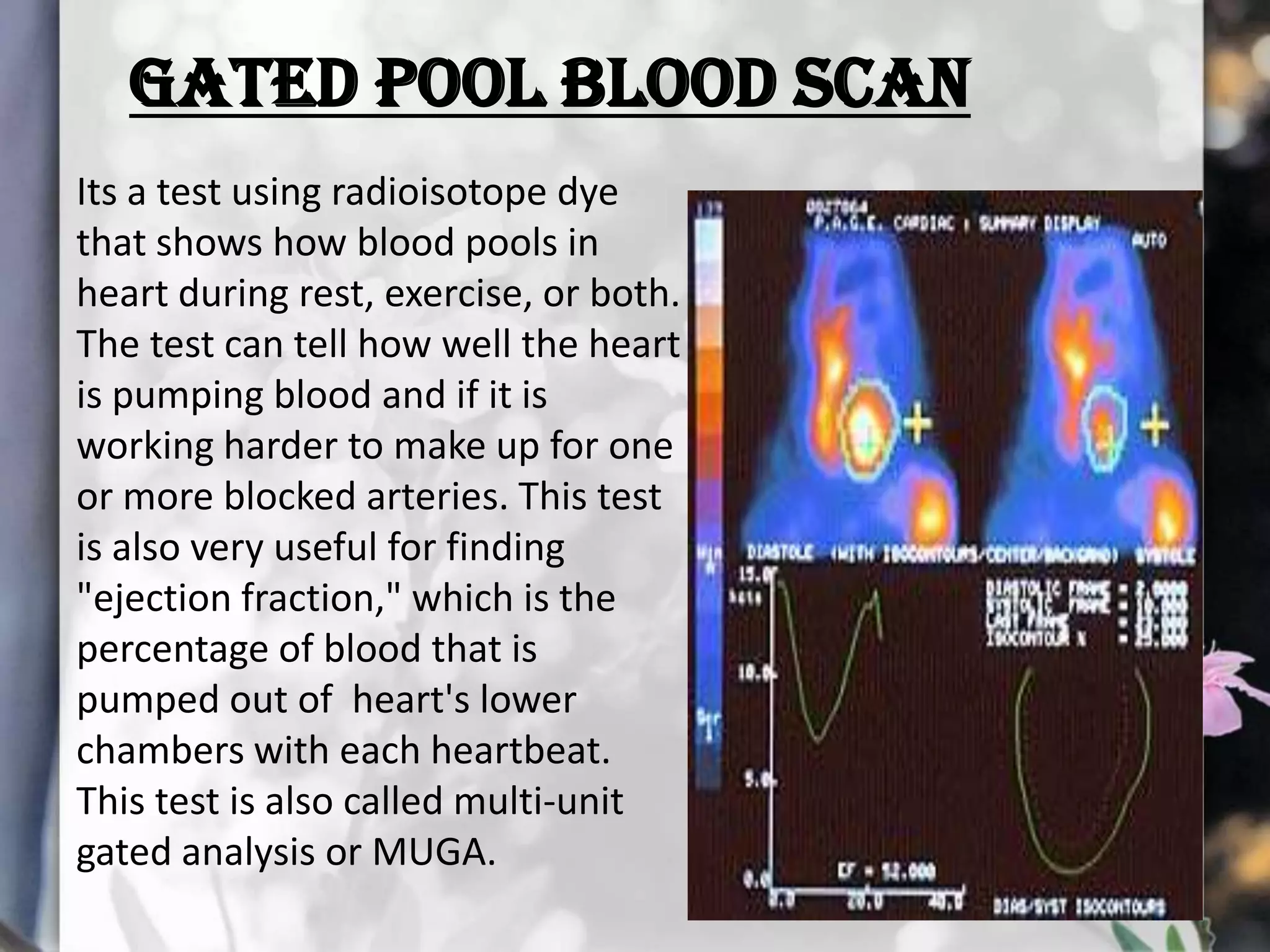
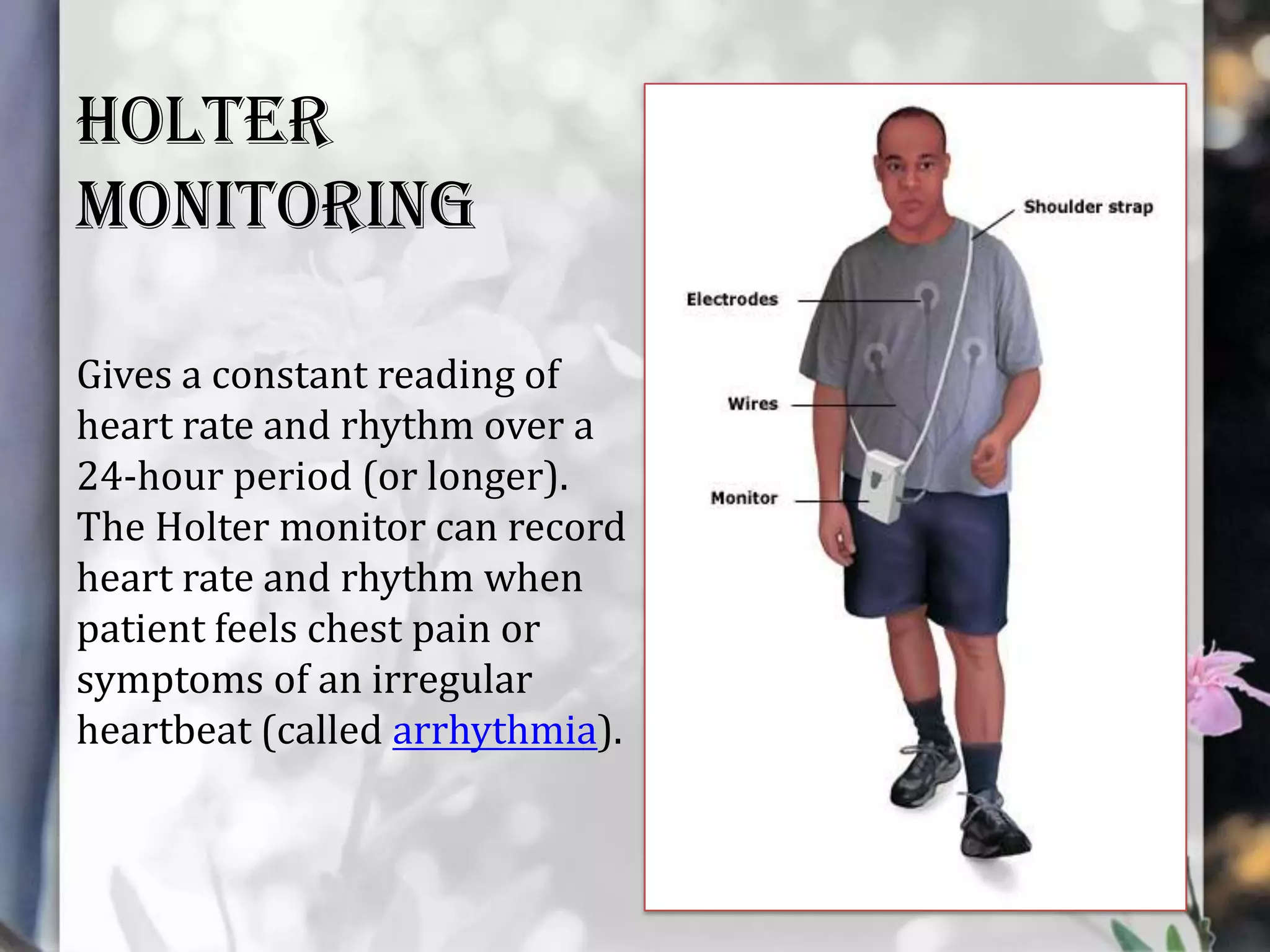
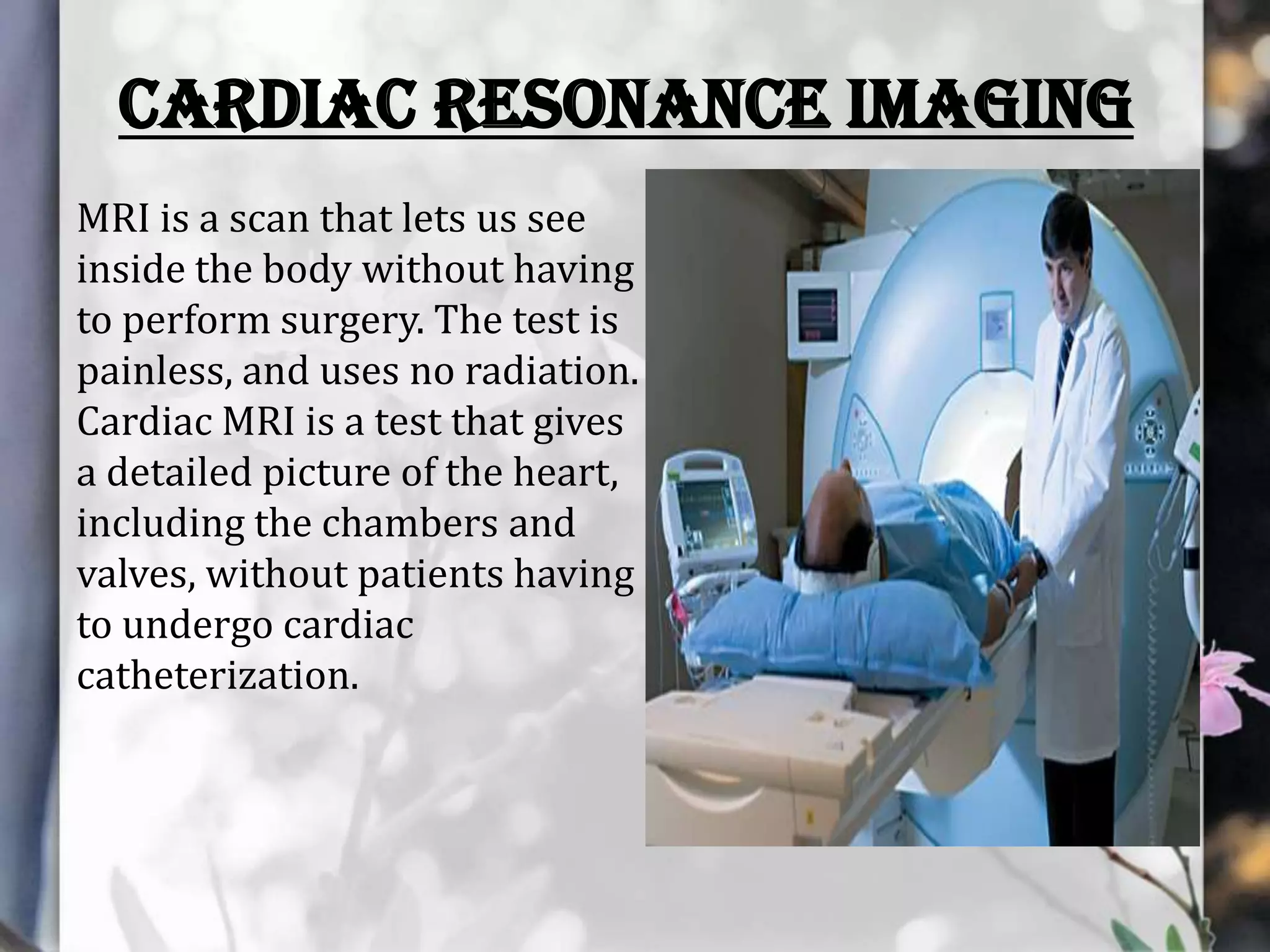
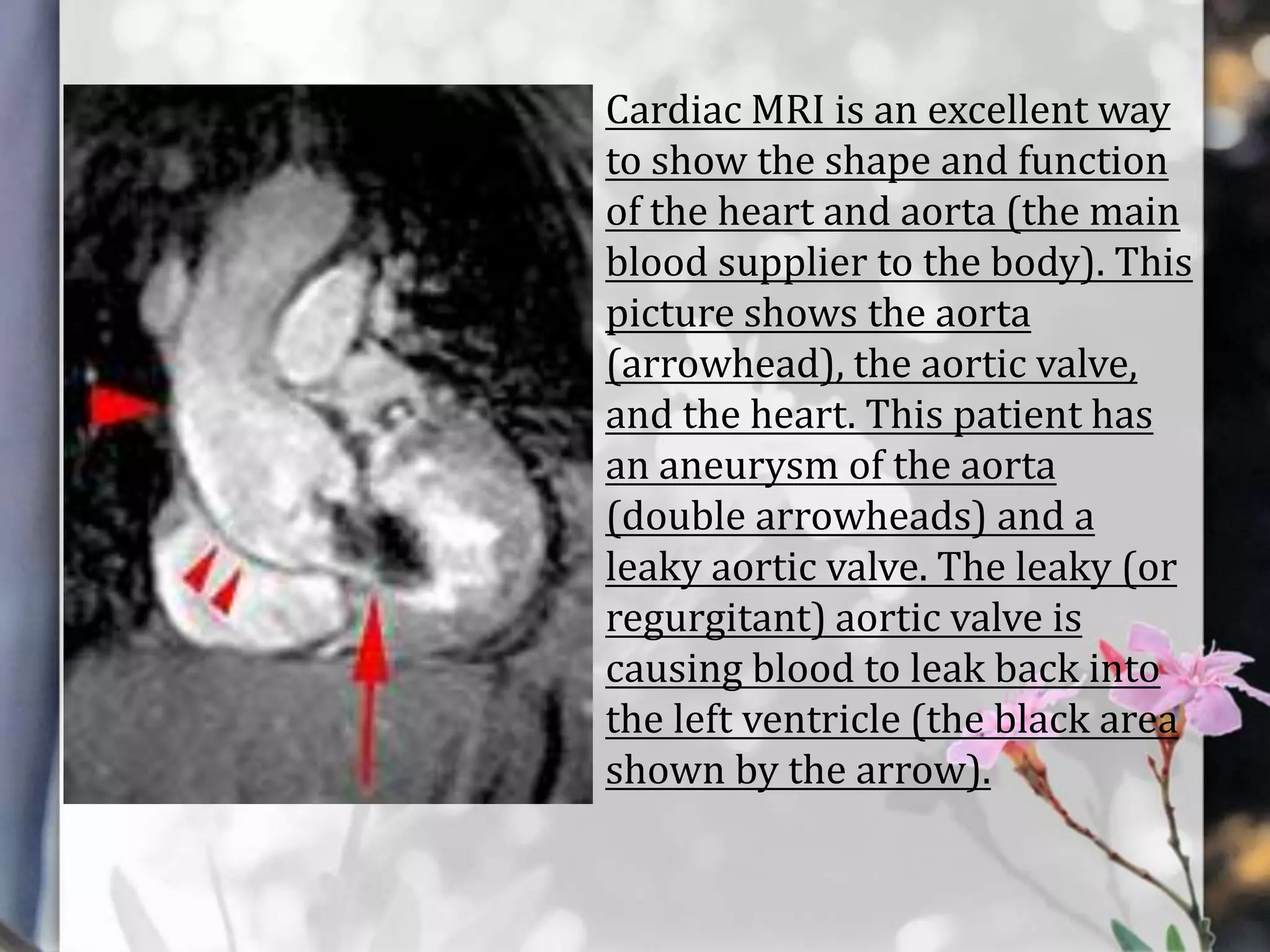
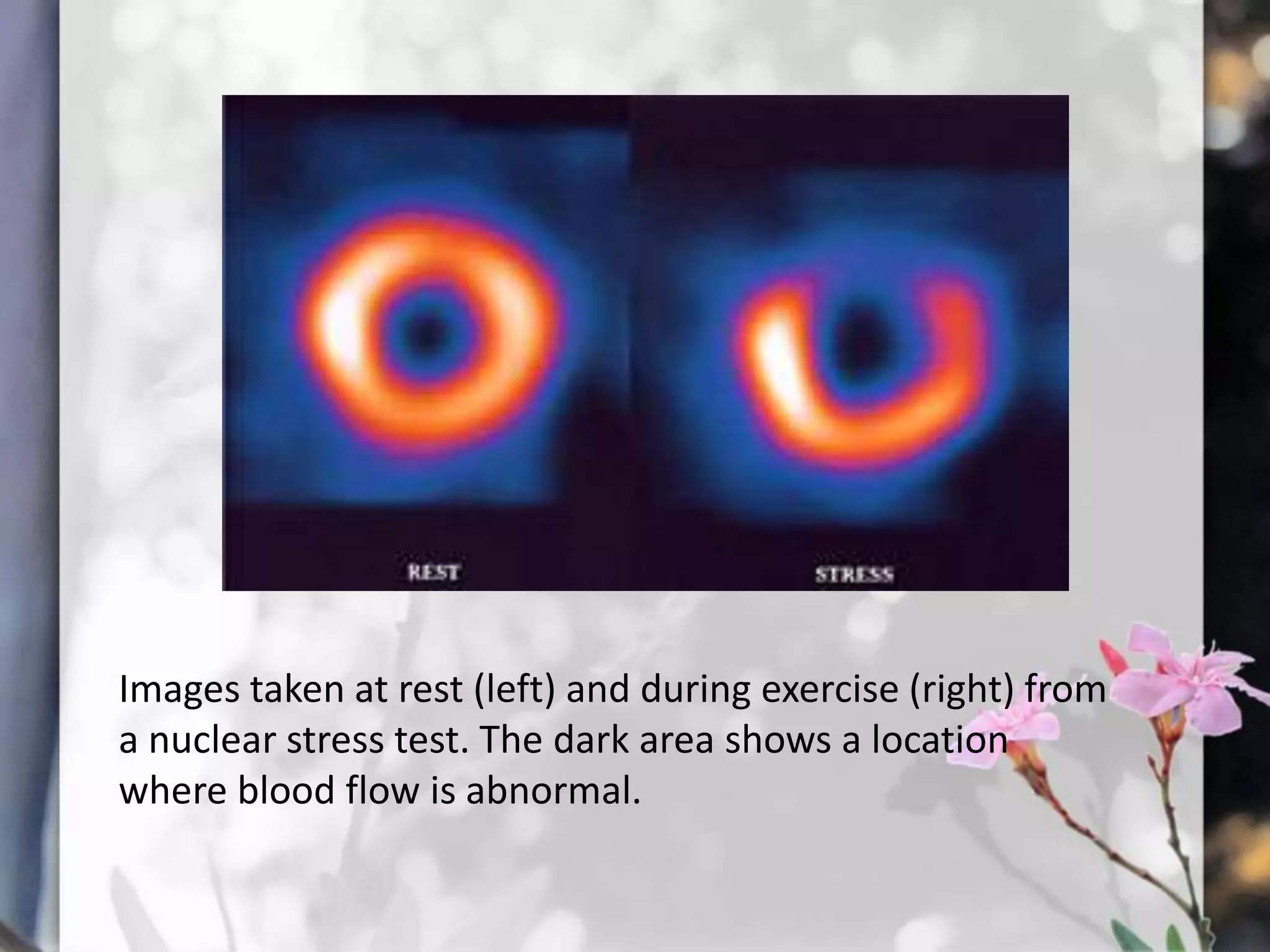
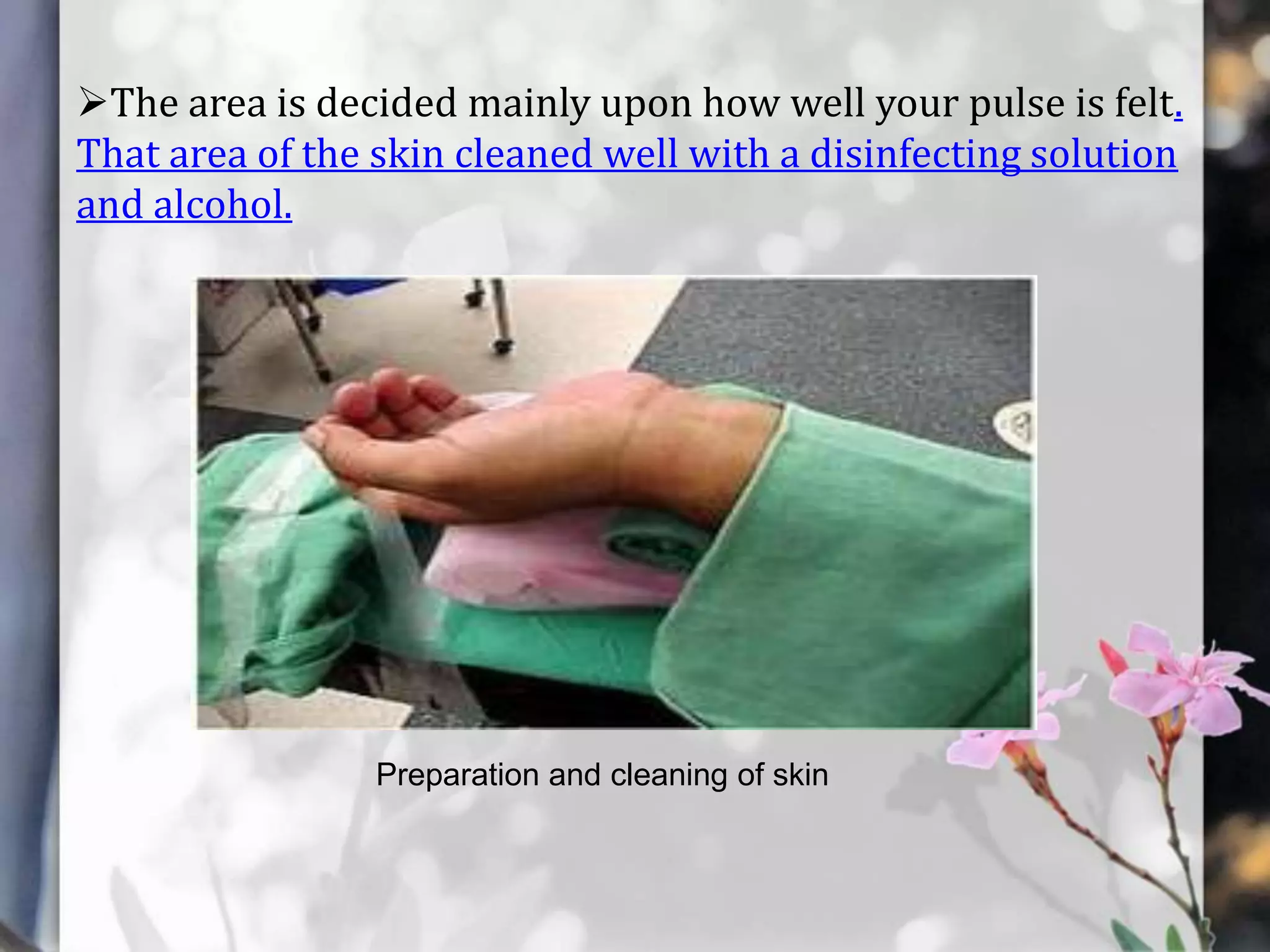
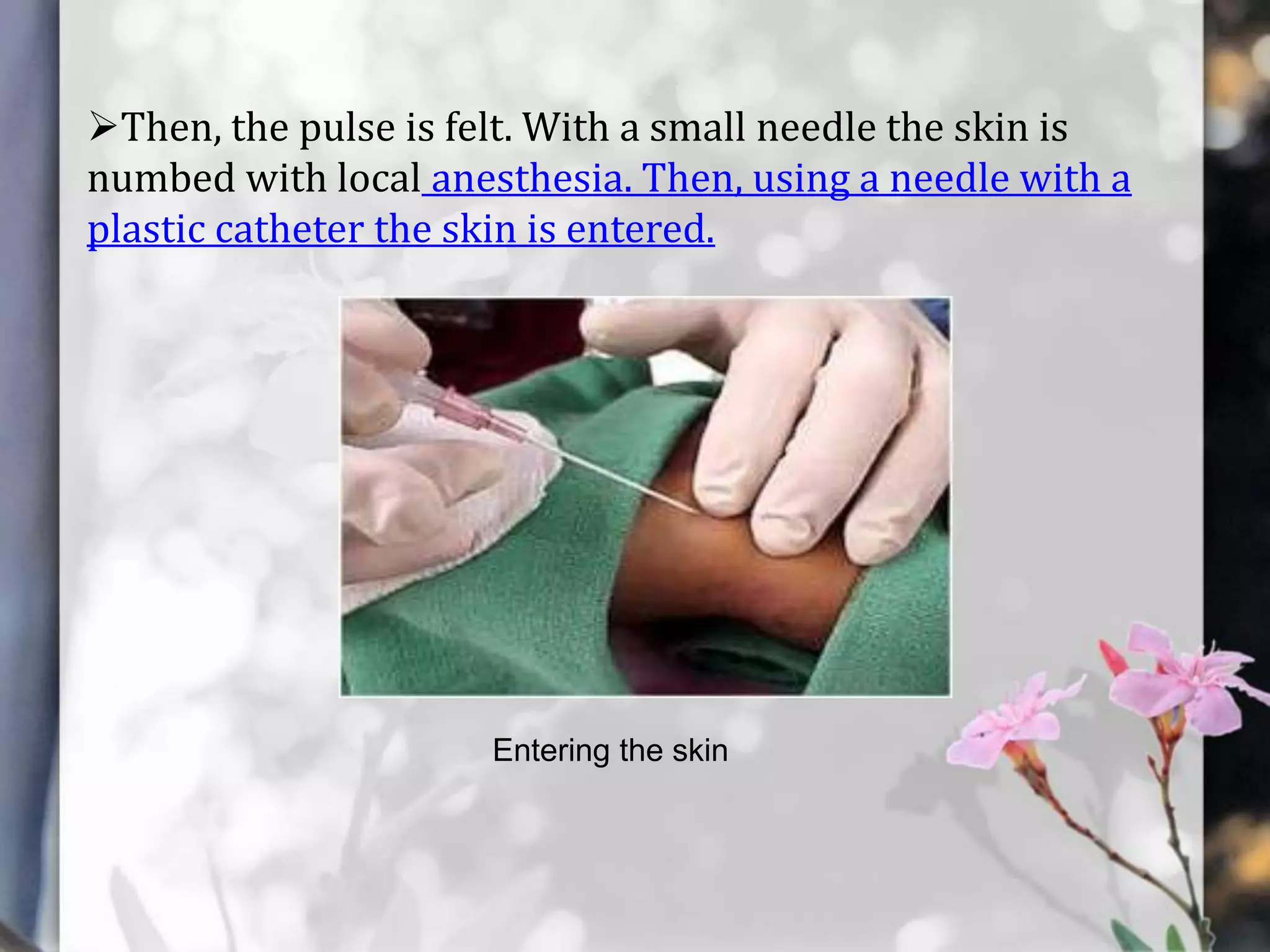
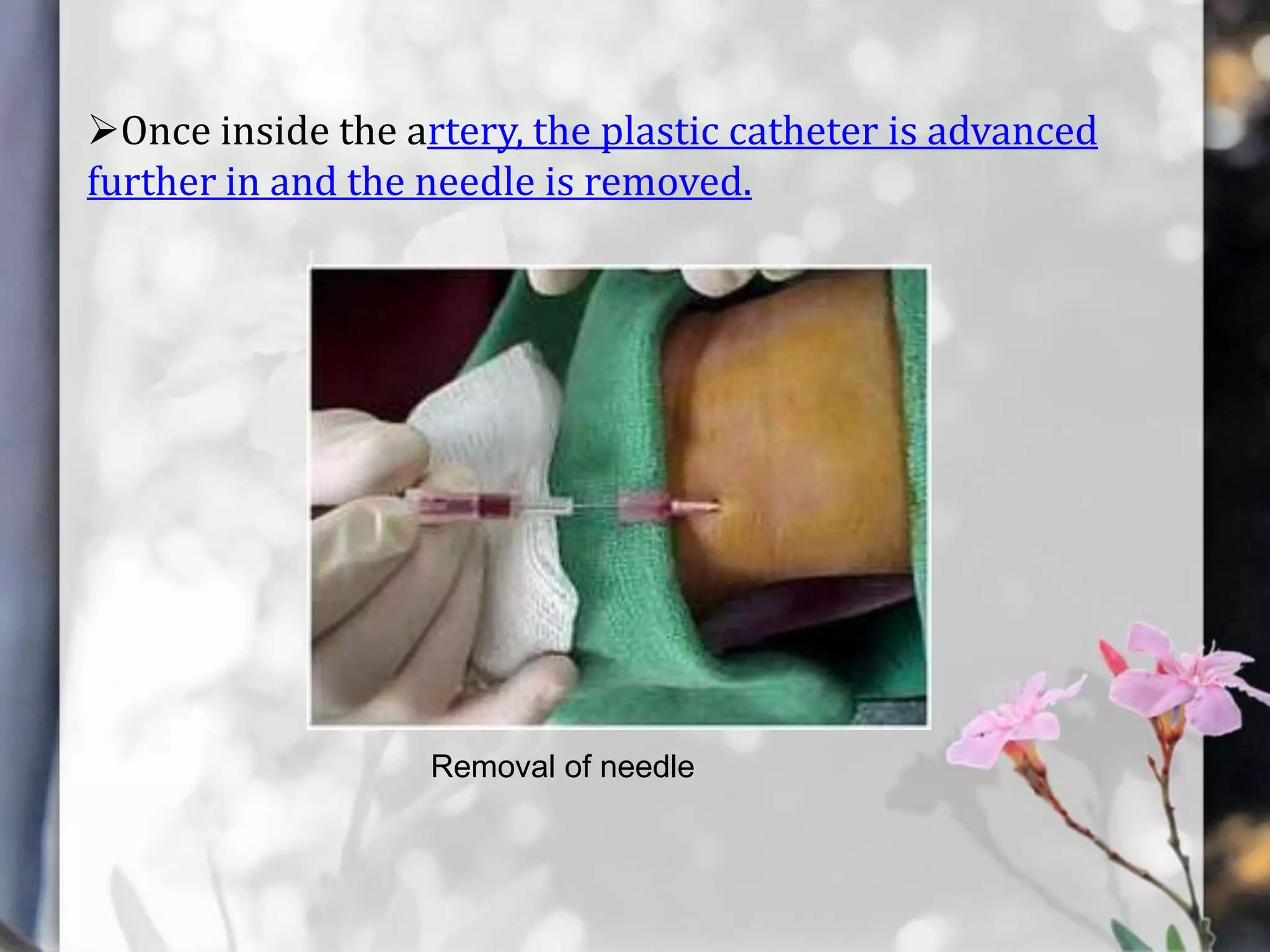
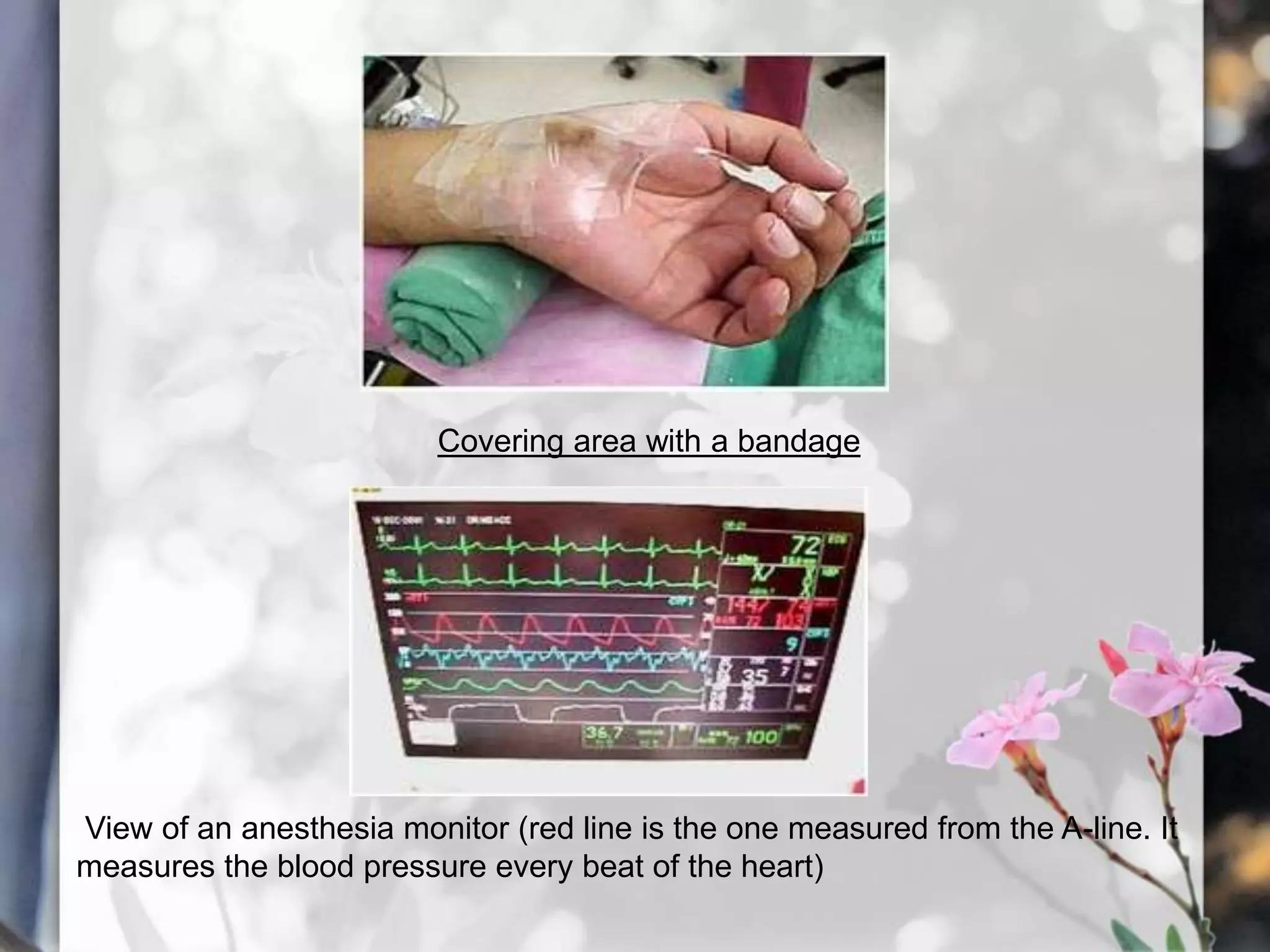
This document describes various cardiac diagnostic tests including imaging tests and blood tests. It provides details on procedures like chest x-rays, echocardiograms, cardiac catheterization, CT scans, and blood tests like cardiac enzymes and electrolyte levels. Precise positioning of patients and monitoring of vital signs during and after procedures is emphasized to obtain clear images and ensure patient safety.