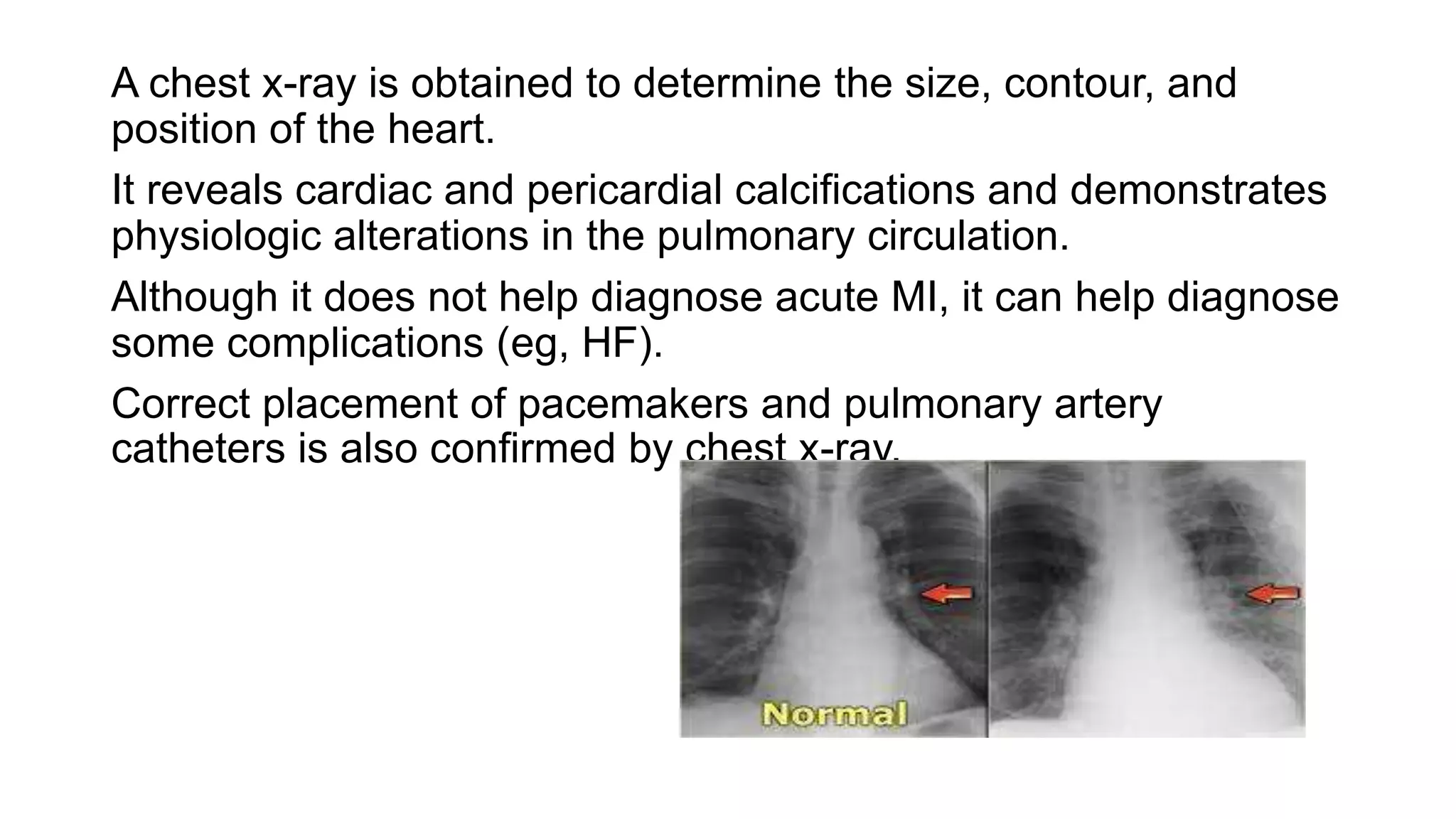
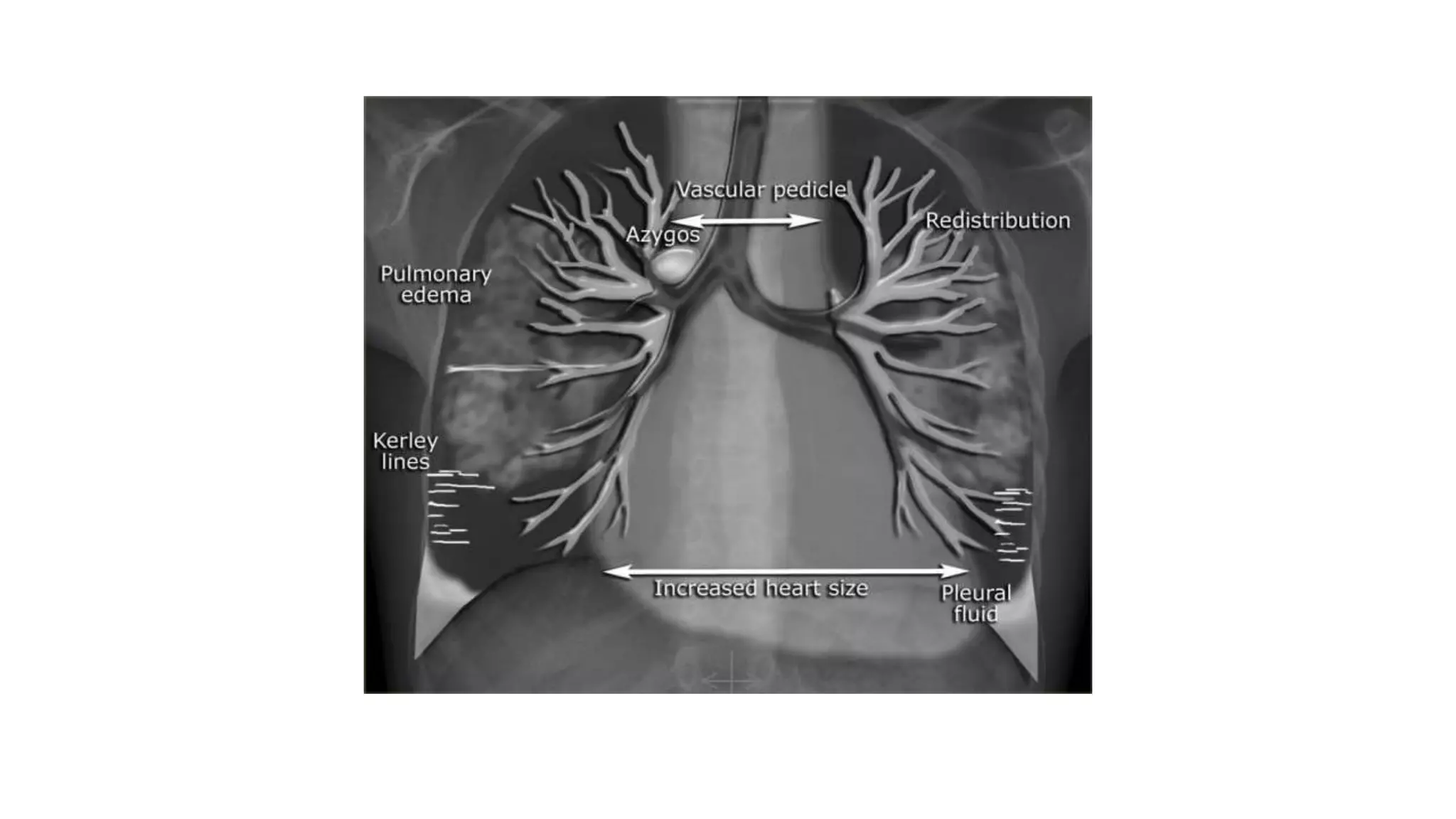
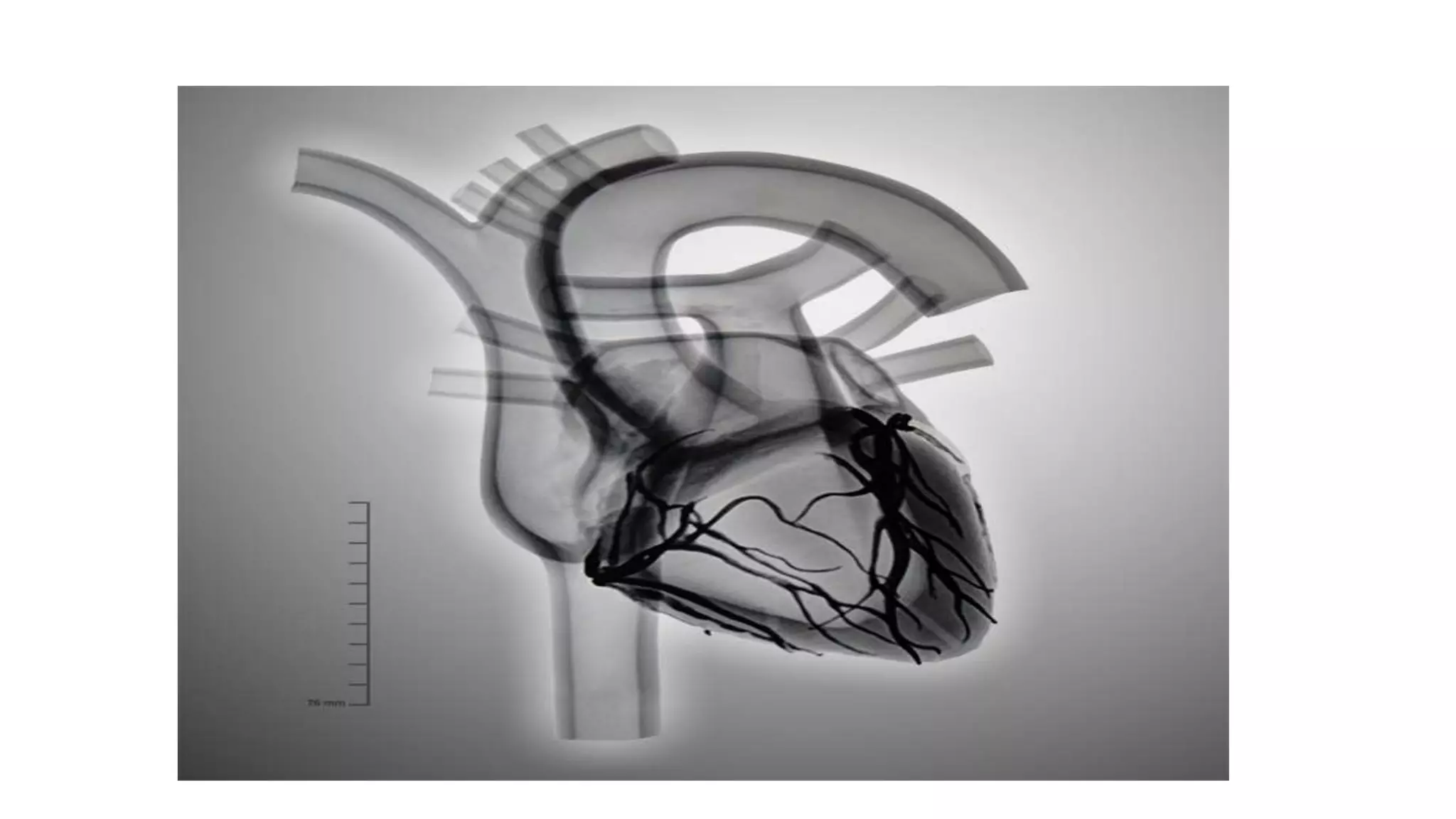
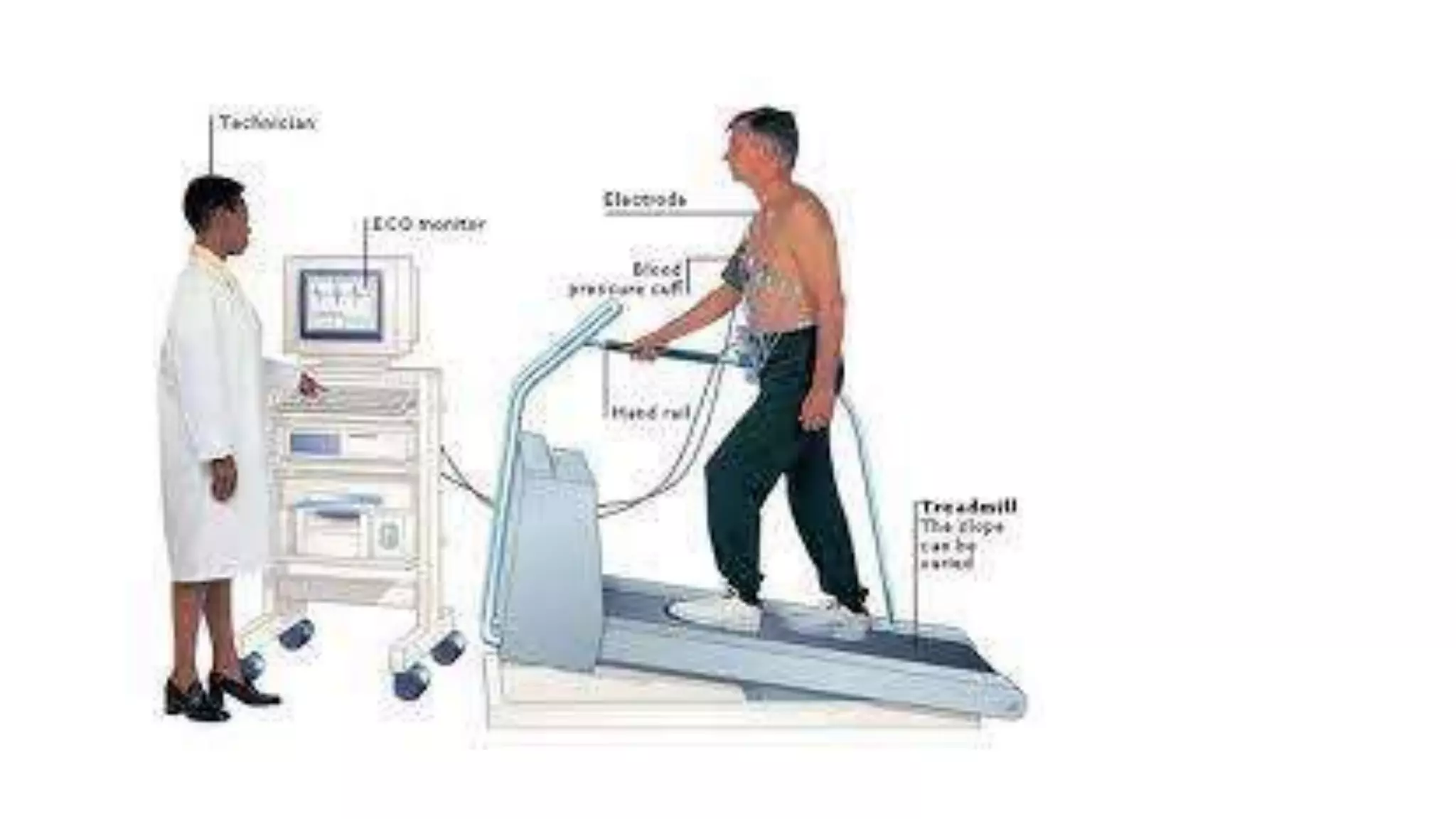
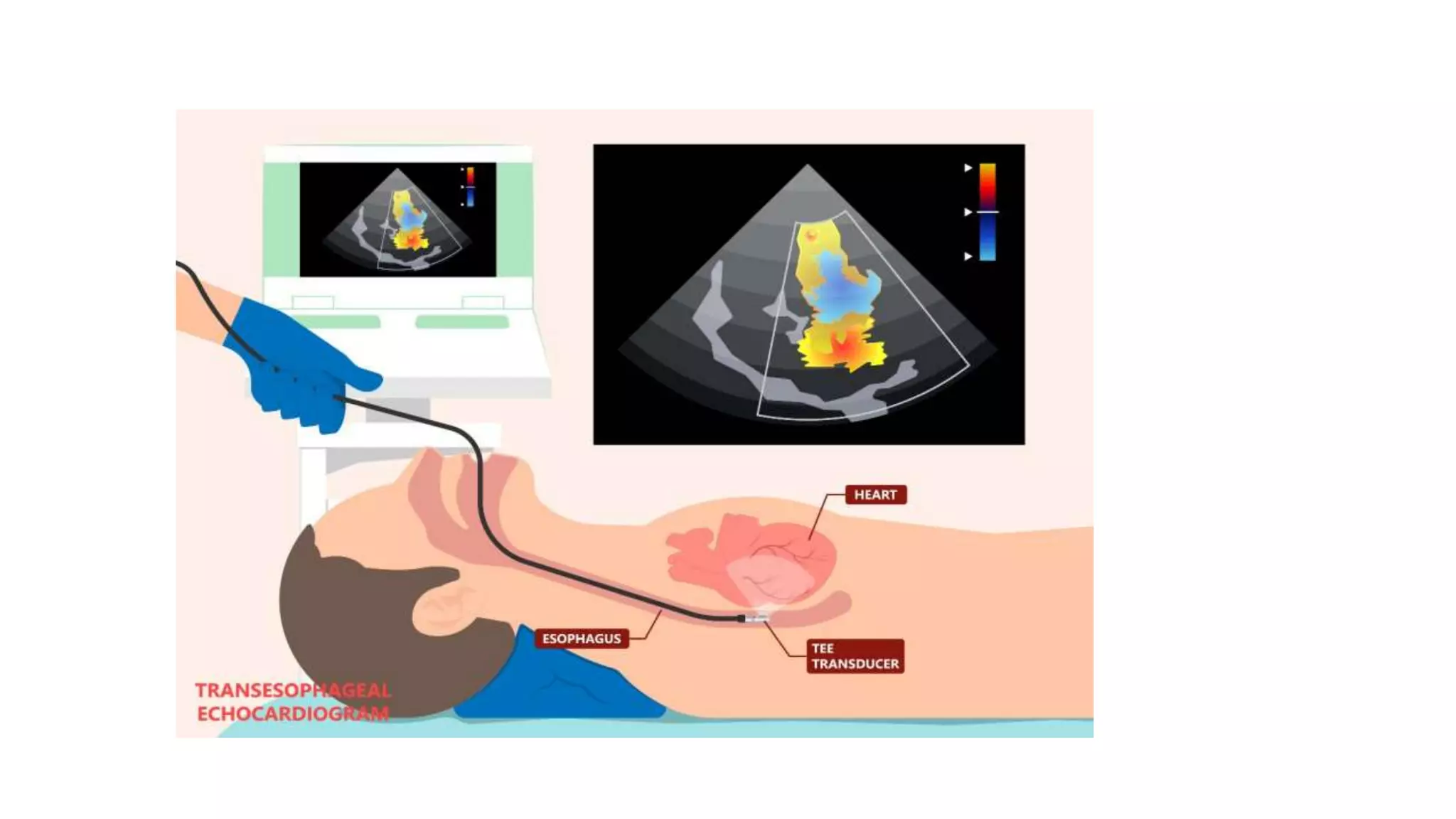
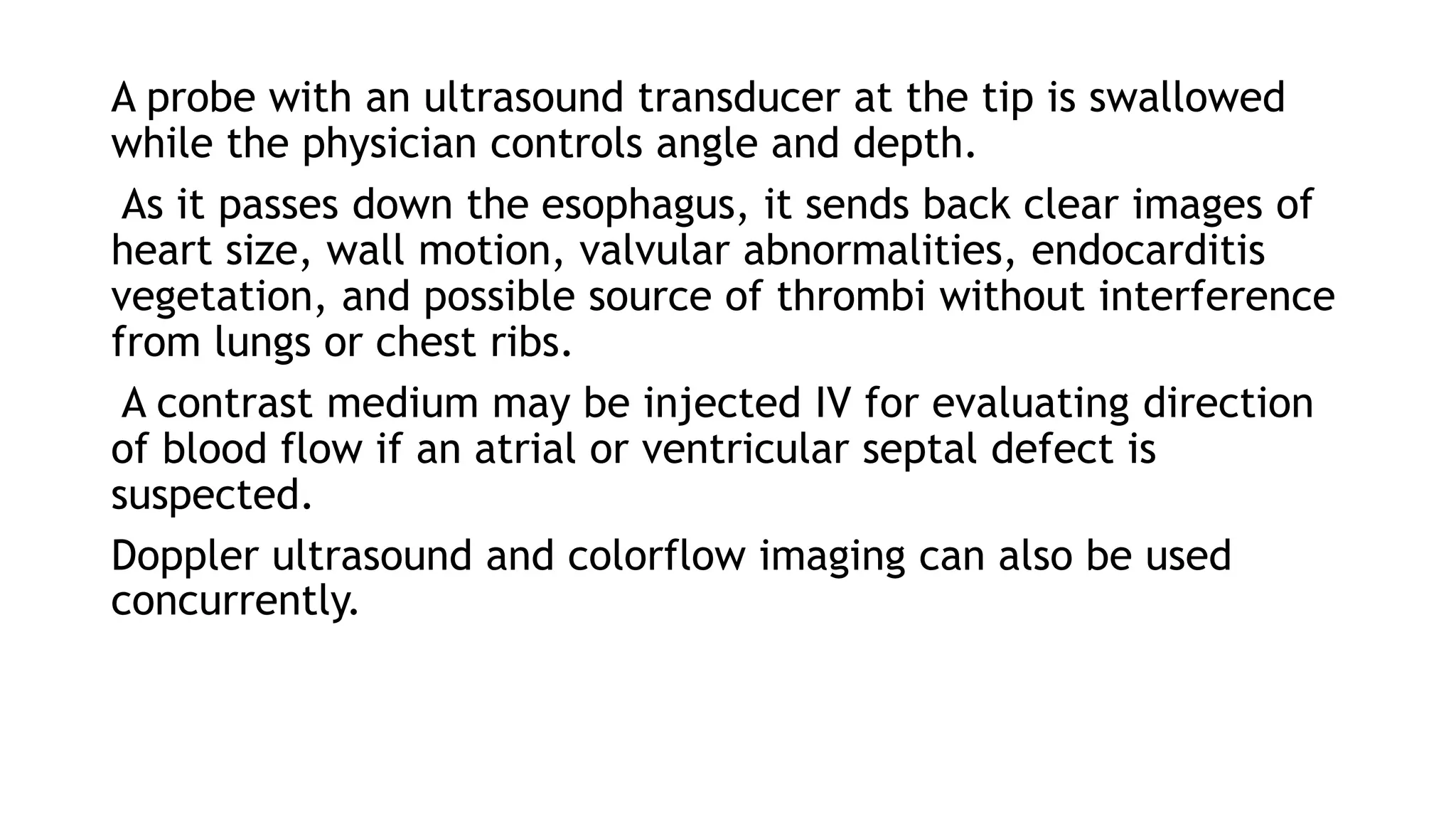
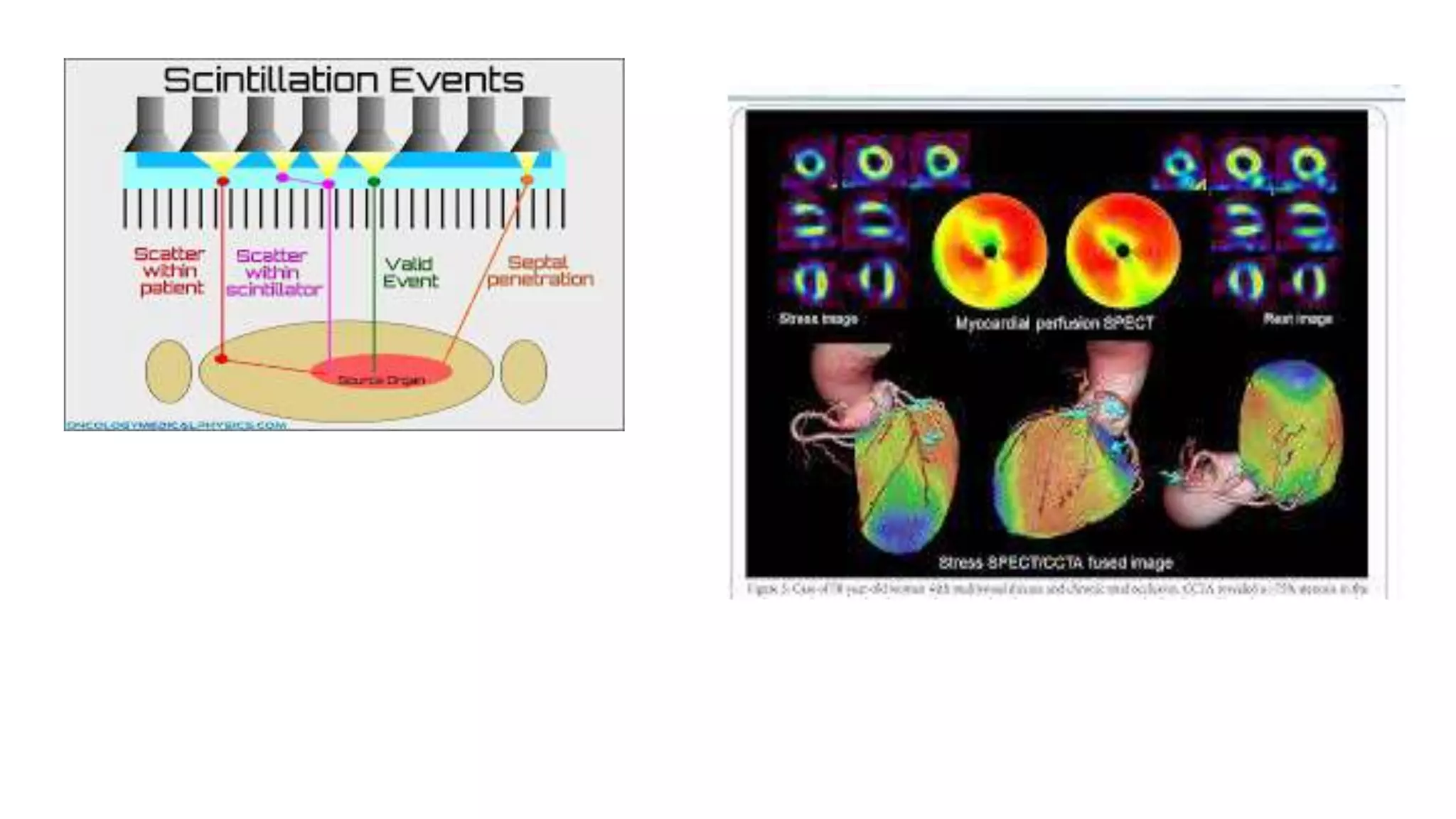
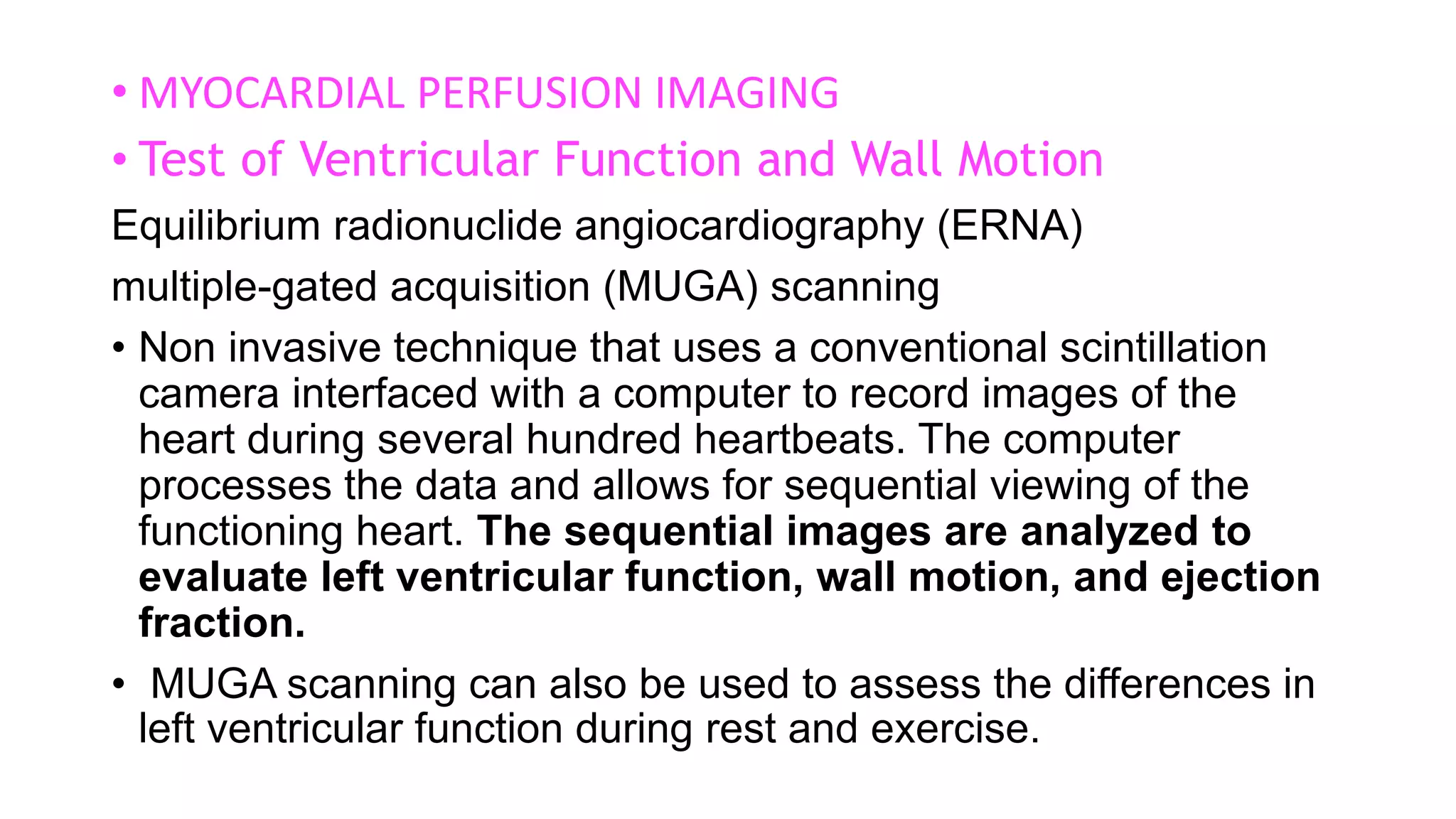
A chest x-ray can determine the size, position, and contour of the heart and reveal cardiac abnormalities, though it cannot diagnose an acute myocardial infarction. It is also used to confirm correct placement of devices like pacemakers. Fluoroscopy allows real-time visualization of heart pulsations and movement of instruments through the body during a procedure. Stress tests evaluate for coronary artery disease and assess heart function by monitoring the patient's heart rate and symptoms during increasing physical exertion or pharmacologically induced stress. Echocardiography uses ultrasound to examine cardiac structures and function noninvasively. Radionuclide imaging injects radioactive tracers to evaluate perfusion and function through gamma camera imaging.